Abstract
Purpose
Major spine surgery with multilevel instrumentation is followed by large amount of opioid consumption, significant pain and difficult mobilization in a population of predominantly chronic pain patients. This case–control study investigated if a standardized comprehensive pain and postoperative nausea and vomiting (PONV) treatment protocol would improve pain treatment in this population.
Methods
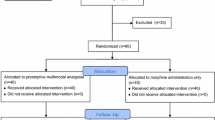
A new regimen with acetaminophen, NSAIDs, gabapentin, S-ketamine, dexamethasone, ondansetron and epidural local anesthetic infusion or patient controlled analgesia with morphine, was introduced in a post-intervention group of 41 consecutive patients undergoing multilevel (median 10) instrumented spinal fusions and compared with 44 patients in a pre-intervention group.
Results
Compared to patients in the pre-intervention group, patients treated according to the new protocol consumed less opioid on postoperative day (POD) 1 (P = 0.024) and 2 (P = 0.048), they were mobilized earlier from bed (P = 0.003) and ambulation was earlier both with and without a walking frame (P = 0.027 and P = 0.027, respectively). Finally, patients following the new protocol experienced low intensities of nausea, sedation and dizziness on POD 1–6.
Conclusions
In this study of patients scheduled for multilevel spine surgery, it was demonstrated that compared to a historic group of patients receiving usual care, a comprehensive and standardized multimodal pain and PONV protocol significantly reduced opioid consumption, improved postoperative mobilization and presented concomitant low levels of nausea, sedation and dizziness.


Similar content being viewed by others
References
Pumberger M, Chiu YL, Ma Y et al (2012) National in-hospital morbidity and mortality trends after lumbar fusion surgery between 1998 and 2008. J Bone Joint Surg Br 94:359–364
Rajaee SS, Bae HW, Kanim LE et al (2012) Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 37:67–76
Buvanendran A, Thillainathan V (2010) Preoperative and postoperative anesthetic and analgesic techniques for minimally invasive surgery of the spine. Spine (Phila Pa 1976) 35:S274–S280
Gottschalk A, Freitag M, Tank S et al (2004) Quality of postoperative pain using an intraoperatively placed epidural catheter after major lumbar spinal surgery. Anesthesiology 101:175–180
Gottschalk A, Durieux ME, Nemergut EC (2011) Intraoperative methadone improves postoperative pain control in patients undergoing complex spine surgery. Anesth Analg 112:218–223
Loftus RW, Yeager MP, Clark JA et al (2010) Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology 113:639–646
Kehlet H, Dahl JB (1993) The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 77:1048–1056
White PF, Kehlet H (2010) Improving postoperative pain management: what are the unresolved issues? Anesthesiology 112:220–225
Kehlet H (2005) Postoperative opioid sparing to hasten recovery: what are the issues? Anesthesiology 102:1083–1085
Kim JC, Choi YS, Kim KN et al (2011) Effective dose of peri-operative oral pregabalin as an adjunct to multimodal analgesic regimen in lumbar spinal fusion surgery. Spine (Phila Pa 1976) 36:428–433
Ziegeler S, Fritsch E, Bauer C et al (2008) Therapeutic effect of intrathecal morphine after posterior lumbar interbody fusion surgery: a prospective, double-blind, randomized study. Spine (Phila Pa 1976) 33:2379–2386
Nielsen PR, Jorgensen LD, Dahl B et al (2010) Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil 24:137–148
Julious SA, George S, Campbell MJ (1995) Sample sizes for studies using the short form 36 (SF-36). J Epidemiol Community Health 49:642–644
Deyo RA, Mirza SK, Martin BI et al (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303:1259–1265
Blumenthal S, McAfee PC, Guyer RD et al (2005) A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine (Phila Pa 1976) 30:1565–1575
Zigler J, Delamarter R, Spivak JM et al (2007) Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine (Phila Pa 1976) 32:1155–1162
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79:168–173
Rasmussen S, Krum-Moller DS, Lauridsen LR et al (2008) Epidural steroid following discectomy for herniated lumbar disc reduces neurological impairment and enhances recovery: a randomized study with two-year follow-up. Spine (Phila Pa 1976) 33:2028–2033
Jirarattanaphochai K, Jung S, Thienthong S et al (2007) Peridural methylprednisolone and wound infiltration with bupivacaine for postoperative pain control after posterior lumbar spine surgery: a randomized double-blinded placebo-controlled trial. Spine (Phila Pa 1976) 32:609–616
De Oliveira GSJ, Almeida MD, Benzon HT et al (2011) Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology 115:575–588
Lunn TH, Kristensen BB, Andersen LO et al (2011) Effect of high-dose preoperative methylprednisolone on pain and recovery after total knee arthroplasty: a randomized, placebo-controlled trial. Br J Anaesth 106:230–238
Dahners LE, Mullis BH (2004) Effects of nonsteroidal anti-inflammatory drugs on bone formation and soft-tissue healing. J Am Acad Orthop Surg 12:139–143
Sucato DJ, Lovejoy JF, Agrawal S et al (2008) Postoperative ketorolac does not predispose to pseudoarthrosis following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 33:1119–1124
Dodwell ER, Latorre JG, Parisini E et al (2010) NSAID exposure and risk of nonunion: a meta-analysis of case-control and cohort studies. Calcif Tissue Int 87:193–202
Maund E, McDaid C, Rice S, Wright K, Jenkins B, Woolacott N (2011) Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs for the reduction in morphine related side-effects after major surgery: a systematic review. Br J Anaesth 106:292–297
Conflict of interest
Benny Dahl is funded by a grant from the Danish Strategic Research Council (#2142-08-0017). No other funding was received for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mathiesen, O., Dahl, B., Thomsen, B.A. et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 22, 2089–2096 (2013). https://doi.org/10.1007/s00586-013-2826-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2826-1