Abstract
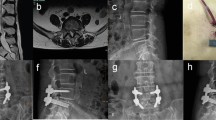
Minimally invasive lumbar fusion techniques have been developed in recent 20 years. The goals of these procedures are to reduce approach-related soft tissue injury, postoperative pain, and disability while allowing the surgery to be conducted in an effective manner. There have been no prospective clinical reports published on the comparison of minimally invasive transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression or a traditional open approach. A prospective clinical study was performed by evaluating the clinical and radiographic results of minimally invasive transforaminal lumbar interbody fusion as an alternative new technique in the revision surgery for patients previously treated by open procedure. 52 patients (28 M, 24 F) with an average age of 55.7 (31–76) were prospectively evaluated. All patients who had previous discectomy (n = 13), hemilaminectomy (n = 16), laminectomy (n = 12) and facetectomy (n = 11) underwent monosegmental and bisegmental minimally invasive transforaminal lumbar interbody fusion (MiTLIF) (n = 25) or open transforaminal lumbar interbody fusion (OTLIF) (n = 27) by two experienced surgeons at one hospital, from March 2006 to October 2008 (minimum 12-month follow-up). The following data were compared between the two groups: the clinical and radiographic results, operative time, blood loss, X-ray exposure time, postoperative back pain, and complications. Clinical outcome was assessed using the visual analogue scale and the Oswestry disability index (ODI). The operative time and clinical and radiographic results were basically identical in both groups. Comparing with the OTLIF group, the MiTLIF group had significantly less blood loss and less postoperative back pain at the second day postoperatively. The radiation time was significantly longer in the MiTLIF group. Complications included three cases of small dural tear in the MiTLIF group. There were five cases of dural tear and two cases of superficial wound infection in the OTLIF group. One case of nonunion was observed from each group. Minimally invasive TLIF is a safe and effective procedure for treatment of selected revision patients previously treated by open surgery with some potential advantages. However, this technique needs longer X-ray exposure time.

Similar content being viewed by others
References
Cloward RB (1982) History of PLIF: forty years of personal experience. In: Lin PM (ed) Posterior lumbar interbody fusion. Charles C Thomas, Springfield, pp 58–71
Cloward RB (1953) The treatment of ruptured intervertebral discs by vertebral body fusion: Part I—indications, operative technique, after care. J Neurosurg 10:154–168
Steffee AD, Sitkowski DJ (1988) Posterior lumbar interbody fusion and plates. Clin Orthop 227:99–102
Harms JG, Jeszenszky D (1998) The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol 6:88–89
Humphreys SC, Hodges SD, Patwardhan AG et al (2001) Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine 26:567–571
Kawaguchi Y, Matsui H, Tsuji H (1996) Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine 21:941–944
Kawaguchi Y, Matsui H, Tsuji H (1994) Back muscle injury after posterior lumbar spine surgery. Part 2: histologic and histochemical analyses in humans. Spine 19:2598–2602
Sihvonen T, Herno A, Paljiarvi L et al (1993) Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 18:575–581
Styf JR, Willen J (1998) The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine 23:354–358
Isaacs RE, Podichetty VK, Santiago P et al (2005) Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine 3:98–105
Schwender JD, Holly LT, Rouben DP et al (2005) Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 18(Suppl):S1–S6
Scheufler KM, Dohmen H, Vougioukas VI (2007) Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery 60:203–212
Ozgur BM, Yoo K, Rodriguez G et al (2005) Minimally invasive technique for transforaminal lumbar interbody fusion (TLIF). Eur Spine J 14:887–894
Schizas C, Tzinieris N, Tsiridis E et al (2008) Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop 33:1683–1688
Peng CWB, Yue WM, Poh SY, Yeo WM et al (2009) Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine 34:1385–1389
Kambin P (1993) Arthroscopic microdiscectomy of the lumbar spine. Clin Sports Med 12:143–150
Lee SH, Choi WG, Lim SR et al (2004) Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis. Spine J 4:644–649
Mayer TG, Vanharanta H, Gatchel RJ et al (1989) Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine 14:33–36
Arts MP, Nieborg A, Brand R et al (2007) Serum creatine phosphokinase as an indicator of muscle injury after various spinal and nonspinal surgical procedures. J Neurosurg 7:282–286
Selznik LA, Shamji MF, Isaacs RE (2009) Minimally invasive interbody fusion for revision lumbar surgery. J Spinal Disord Tech 22:207–213
Ringel F, Stoffel M, Stuer C et al (2006) Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 59(4 Suppl 2):ONS361–ONS366
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication.
Rights and permissions
About this article
Cite this article
Wang, J., Zhou, Y., Zhang, Z.F. et al. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J 20, 623–628 (2011). https://doi.org/10.1007/s00586-010-1578-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-010-1578-4