Abstract
Thoracoplasty in combination with spine fusion is an established method to address the rib cage deformity in idiopathic scoliosis. Most reports about thoracoplasty and scoliosis correction focused on Harrington or CD instrumentation. We report a retrospective analysis of 21 consecutive patients, who were treated with pedicle screw instrumentation for idiopathic thoracic scoliosis and concomitant thoracoplasty. Minimal follow up was 24 (24–75) months. Indication for thoracoplasty was clinical rib prominence of more than 15°. In average there was a 44% correction of clinical rib hump, from 18 (15–25°) to 10° (0–18°) (p<0.0001) and a 40% correction of radiological rib hump, from 15 (5–20°) to 9°(2–15°) (p<0.0001). The preoperative pulmonary function, accessed by forced vital capacity (FVC) and one-second forced expiratory volume (FEV1), remained unchanged at the last follow up. The distal end of fusion was the end vertebra of the curve in 83.3% and the end vertebra plus one in 16.7% of the patients. There was a 68% correction of instrumented primary thoracic curves, from 60 (45–85°) to 19°(5–36°) (p<0.0001), and a 45% correction of non-instrumented secondary lumbar curves, from 40 (28–60°) to 22°(8–38°) (p<0.0001). Apical vertebral rotation (AVR) of the thoracic curves improved 54%, from 24 (10–35°) to 11° (5–20°) (p<0.0001). The tilt of lowest instrumented vertebra (LIV) improved 68%, from 28 (20–42°) to 9°(3–20°) (p<0.0001). There was no significant change in sagittal profile of the spine. Analysis with SRS-24 questionnaire showed that the majority of the patients were very satisfied with the outcome. A matched control group (n=21) operated by the same surgeon with the same operation technique but without concomitant thoracoplasty was chosen for comparison. The scoliosis correction in the two groups was comparable. The patients without thoracoplasty had 37% spontaneous improvement of the clinical rib hump.
Similar content being viewed by others
Introduction
Body contour and body form are important factors for self esteem in young people. The convex rib prominence is often of the major source of cosmetic concern to patients with thoracic scoliosis [5]. Thoracoplasty by means of multiple rib resection is an established method to address the rib cage deformity in thoracic idiopathic scoliosis [1, 4, 5, 15]. Reports about thoracoplasty were in conjunction with instrumentation of scoliosis using Harrington or CD instrumentation [5, 8, 15, 19]. The use of pedicle screws for correction of scoliosis is safe and leads to better curve correction [7, 11, 12, 16, 17]. There are no reports about the results of thoracoplasty together with scoliosis correction using thoracic pedicle screws. About 21 consecutive patients were retrospectively analysed, concerning deformity correction, rib hump correction, changes in lung function and patients’ satisfaction with SRS-24 questionnaire. The results were compared to a matched group of 21 patients without thoracoplasty.
Materials and methods
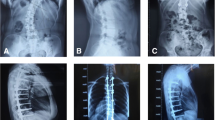
About 21 patients (19 females and 2 males) were operated for thoracic idiopathic scoliosis with pedicle screw instrumentation and concomitant convex thoracoplasty from 1996 to 2001 in our institution. The indication for scoliosis correction was a thoracic curve greater than 45°. Additional thoracoplasty was indicated when there was a rib prominence of more than 15°. The degree of rib hump was measured clinically with a scoliometer in standing forward bending position [3]. Preoperative and postoperative data were obtained from hospital medical records. Mean age at the time of operation was 15.9 (11–33) years. According to the King classification [10] there were 14 type II curves, five type III curves, one type IV, and one type V curves. Risser stage at the time of surgery was one in one patient, two in three patients, three in nine patients, four in seven patients, and five in one patient. All surgical interventions were done by the senior author (KM). Scoliosis was first corrected from posterior, followed by thoracoplasty in the same anaesthesia. All the operations were done under continuous neuromonitoring with SSEP and MEP. Pedicle screw alone constructs with stainless steel Universal Spine System (Synthes) were used for scoliosis correction. Thoracic pedicle screws were inserted using anatomical landmarks and funneling technique. Main proportion of the correction of the scoliosis was done through translation and derotation of the apex using the side-opening monoaxial pedicle screws on the concave side of the curve. Cantilevering on the convex side of the curve was used in rigid curves to assist in derotation. Rod derotation was not applied. Thoracoplasty was performed through the same posterior midline skin incision. Through subcutaneous lateral dissection on the convex side, the ribs forming the rib hump were exposed lateral to the trapezius muscle, which was then retracted medially. After strict subperiosteal exposure a length of 2.5 cm was resected from each rib. Pleura was protected by intact periosteum. An average of five ribs was resected per patient. The ends of the ribs were left in the periosteal sheath, without explicit fixation to the soft tissue or other ribs. The resected ribs were used for spinal fusion. Wound closure was done with a suction drain. Two epidural catheters were inserted by the surgeon at the end of the operation for the postoperative analgesia. No chest drains were inserted primarily. A total of 212 pedicle screws were used in 21 patients for scoliosis correction. The average number of pedicle screws per patient was 10 (9–12) and the average number of segments fused per patient was 9 (7–10). The lowest level of instrumentation was T11 in three patients, T12 in nine patients, L1 in five patients and L2 in four patients. Ambulation began on first day without bracing. The follow up assessment was done by two independent observers (BW, FH) not involved in the care of the patients. The patients were clinically examined and asked to respond to a self-rating questionnaire (SRS-24) [6]. Radiological data were analysed from upright full spine anteroposterior and lateral radiographs preoperatively, 6 weeks postoperatively and at the latest follow up. Radiological measurement of the rib hump was done on tangential films (“rib hump” view)[8, 13] taken preoperatively and at the last follow up (Fig. 1). The thoracic kyphosis was measured from T4 to T12 and the lumbar lordosis from L1 to S1. Forced vital capacity (FVC) and 1-s forced expiratory volume (FEV1) were measured preoperatively and at the last follow up.
The results of these patients were compared to the results of a control group (n=21) matched for age, type and size of scoliosis, duration of follow up, operated by the same surgeon in the same institution with the same correction technique using pedicle screws but without concomitant thoracoplasty as the preoperative clinical rib hump was less than 15°. There were nine King type II, four type III, three type IV, and five type V curves. Average Risser stage was 3 (0–5). In the control group a total of 202 pedicle screws were inserted, the average number of pedicle screws per patient being 9.6 (8–12) and the average number of segments fused 8.6 (7–10). The lowest level of instrumentation was L2 in four, L1 in five, T12 in nine, and T11 in three patients. The data about the length of hospital stay, complications, scoliosis correction, change in clinical rib hump, and the scores of SRS-24 questionnaire were compared.
The distal end vertebra of the curve was chosen as distal fusion level if the end vertebra touched the centre sacral vertical line. When there were two parallel end vertebrae at the distal end of the curve, the lower one was chosen. One level distal to end vertebra was chosen if the end vertebra did not touch the centre sacral vertical line, which was the case in seven of the 42 patients in our present series.
Results
Average hospital stay for the thoracoplasty group was 14 (10–17) days. In two patients a thorax drain needed to be inserted on the 2nd postoperative day as pleural effusion was seen on routine chest radiographs. Serous effusion was drained in both patients and the drains could be removed after 2 days. We did not see any hemothorax. There were no other complications of thoracoplasty. There were no implant related complications or neurological complications. The mean preoperative Cobb angle of the thoracic curves was 60° (45–85°). The average flexibility was 47% (20–60%). There was a 68% correction of primary instrumented thoracic curves to 19° (4–35°) at 6 weeks postoperative to 19°(5–36°) at the last follow up (p<0.0001). There was no significant loss of correction. Apical vertebral rotation according to Perdriolle measurement [13] improved 54% from 24 (10–35°) to 11° (5–20°) postoperatively and to 11° (5–20°) at the last follow up (p<0.0001). The tilt of the lowest instrumented vertebra (LIV) improved 67.8% from 28 (20–42°) to 9° (0–20°) postoperatively and to 9° (3–20°) at the last follow up (p<0.0001). In King II curves the non-instrumented lumbar curves improved 45% from 40 (28–60°) to 20° (10–35°) postoperatively and to 22° (8–38°) at the last follow up (p<0.0001). The thoracic kyphosis changed from 27 (10–48)° to 29° (10–45°) and the lumbar lordosis changed from 56 (35–75°) to 58° (35–80°) at the last follow up. These changes were statistically not significant. The global coronal balance, determined by the horizontal distance from the C7 plumb line to the centre sacral vertical line, was 12 mm (0–35 mm) preoperatively, and 11 mm (0–24 mm) at the last follow up. There was a 40% improvement of the radiographic rib hump from 15 (5–20°) to 9° (2–18°) (p<0.0001) and a 44% improvement of the clinical rib hump from 18 (15–25°) to 10° (0–18°) at the last follow up (p<0.0001). The percentage of expected FVC% did not change significantly from preoperative 73 (42–106%) to 72% (49–92%) at the last follow up. The FEV1 was not affected by the operation as the slight increase from an average of 2306 to 2649 ml (n=16) was statistically not significant. 20 out of 21 patients responded to the SRS-24 questionnaire. Preoperative SRS-24 scores were not available due to the retrospective character of the study. The average total score of the questionnaire was 89 (40–112) out of a maximum of 120 possible points. For the subscore pain 25 (1–35), for the general self-image 12 (7–15), for the postoperative self-image 10 (4–15) and for the postoperative function 6 (2–10) points were determined. The score for the function from the back condition and the level of activity were 11 (6–13) and 12 (4–15), respectively and in patients satisfaction an average score of 12 (6–15) was achieved.
In the control group the average hospital stay was 11.3 days (8–17). There were no postoperative complications. The mean preoperative Cobb angle of the thoracic curve was 54° (38–80°). The average flexibility was 50% (20–60%). There was a 65% (22–97%) correction of the thoracic curve to 14.2° (0–35°) at 6 weeks postoperative to 17.1° (2–35°) at the last follow up (p<0.0001). The apical vertebral rotation (AVR) in the control group improved 60.6% from 19.8 (10–35°) to 9.0° (0–20°) postoperatively and to 7.1 (0–25°) at the last follow up (p<0.0001). The LIV tilt improved 70%, from 26 (25–45°) to 7.7° (0–15°). In King II curves there was 54% improvement of the compensatory lumbar curves, from 39 (30–45°) to 17.8° (10–25°) at the last follow up. The average clinical rib hump of this group was 12.2° (8–14) preoperatively and 7.6° (5–12) at the last follow up. This represented a spontaneous improvement of 37%. A worsening of the rib hump was not observed in any patients. The radiological rib hump measurements for this group were not available as rib hump radiographs had been taken only in patients planned for thoracoplasty. The total score of the SRS-24 questionnaire (n=17) was 96 (66–112). The subscores were as follows: pain 29 (20–34), the general self-image 12 (9–15), the postoperative self-image 11 (9–14), the postoperative function 6 (2–10), the function from the back condition 13 (9–15), the level of activity 13 (5–15) and the patient’s satisfaction 12 (6–15) points. For the total score and in all the subscores the differences between the thoracoplasty group and the control group were not statistically significant. There were no complications related to pedicle screws in any patients in both groups.
Discussion
Reducing the rib deformity through resection of prominent ribs is an important factor for the patient’s satisfaction in scoliosis surgery. Thulbourne and Gillespie [18] showed that there is no strong correlation of the Cobb angle, the vertebral rotation, and the rib vertebral angle. In their series Harrington rod distraction had little effect of the rib hump deformity despite improvement of the Cobb angle. With the introduction of the CD instrumentation it was possible to obtain multidirectional correction of the spine but the rib hump deformity was not corrected [9] and could be addressed only by thoracoplasty [19]. Harvey suggested a primary thoracoplasty in patients instrumented with the CD instrumentation when the rib prominence exceeds 15° [8]. Recently it has been shown that the segmental pedicle screw instrumentation alone or in combination with the proximal hooks offers a better curve correction in idiopathic thoracic scoliosis and allows a shorter fusion [12]. Thoracic pedicle screw instrumentation for idiopathic thoracic scoliosis has been routinely used in our institution since 1995. We did not instrument every single vertebra in the curve. We used an average of ten screws per patient for an average of nine segments fused per patient. We used a stable foundation with three or four screws at the lower two vertebrae, two screws at the top vertebra, and screws on the concave side at the region of the apex (Fig. 2). The achieved correction was comparable to other reports using pedicle screw techniques [7, 12, 16]. The fusion ended at the distal Cobb end vertebra in 83.3% of the patients and one vertebra below the end vertebra in 16.7%. According to our experience it was not necessary to extend the fusion to one level below end vertebra as a standard. Distal end of the fusion was L2 in 19%, L1 in 24%, T12 in 43%, and T11 in 14% of the patients. The sagittal profile of the spine did not change significantly, which was in conformity with the results of Liljenqvist et al. [12]. Fusion of the thoracic spine selectively from posterior will probably not produce significance changes of thoracic kyphosis and lumbar lordosis. We had an average of 37% spontaneous improvement of clinical rib hump in patients without concomitant thoracoplasty. With our technique of thoracoplasty we achieved a 44% improvement of the clinical rib hump. Even though the patients of the control group were matched for age, size and form of scoliosis, they were different in size of clinical rib hump. To our knowledge there are no reports on comparative study of changes in rib hump with and without thoracoplasty. It has been generally agreed that rib resection should not be done before skeletal maturity, concerning the possibility of recurrence from the further rotation of the spine [2, 14]. There were four immature patients in our series, one with Risser 1 and three with Risser 2. We did not observe a rib hump recurrence in these patients. It is probably because of the limited amount of our rib resections (five per patient) and also because the fixation with thoracic pedicle screws might have arrested the spinal rotation during further growth. Caution should however be observed in very young patients with Risser 0. Resection of five ribs at the most prominent convex region did not increase morbidity although it prolonged the hospital stay for 2–3 days compared to the control group. According to our experience it was not necessary to insert a thorax drain routinely after the thoracoplasty. Pneumothorax was avoidable by leaving the periosteum intact to protect the pleura. The thorax could be drained when there were clinical or radiological indications for effusion, which was the case in two of the 21 patients (10%). In both cases pleural irritation was the cause of serous effusion. The long-term intercostal neuralgia as described by Broome et al. [2] in 29% of their patients was not observed in our series. This may be explained by the fact that we left the cut ends of the ribs free in the periosteal sheath instead of fixing them either directly to the soft tissue or to the segments caudally, thereby minimizing the possibility of damaging the neurovascular bundle. The vital capacity of the lungs measured by FVC% and FEV1 was not influenced by thoracoplasty.
Conclusions
The instrumentation with the pedicle screws is a reliable method and gives a good coronal and rotational correction in the idiopathic thoracic scoliosis. Instrumentation of every single vertebra in the curve is not necessary to achieve a good correction. Lumbar segments are saved by limiting the fusion to the lower end vertebra of the thoracic curve in majority of the cases. Patients with a preoperative rib hump of less than 15° have a 37% spontaneous improvement of the rib hump. Additional thoracoplasty corrects the rib deformity to 44% in patients with preoperative rib humps larger than 15°. The pulmonary function is unaffected by this procedure.
References
Barrett DS, MacLean JG, Bettany J, Ransford AO, Edgar MA (1993) Costoplasty in adolescent idiopathic scoliosis. Objective results in 55 patients. J Bone Joint Surg Br 75:881–885
Broome G, Simpson AH, Catalan J, Jefferson RJ, Houghton GR (1990) The modified schollner costoplasty. J Bone Joint Surg Br 72:894–900
Bunnell WP (1984) An objective criterion for scoliosis screening. J Bone Joint Surg Am 66:1381–1387
Erkula G, Sponseller PD, Kiter AE (2003) Rib deformity in scoliosis. Eur Spine J 12:281–287
Geissele AE, Ogilvie JW, Cohen M, Bradford DS (1994) Thoracoplasty for the treatment of rib prominence in thoracic scoliosis. Spine 19:1636–1642
Haher TR, Gorup JM, Shin TM, Homel P, Merola AA, Grogan DP, Pugh L, Lowe TG, Murray M (1999) Results of the scoliosis research society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine 24:1435–1440
Halm H, Niemeyer T, Link T, Liljenqvist U (2000) Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J 9:191–197
Harvey CJ Jr, Betz RR, Clements DH, Huss GK, Clancy M (1993) Are there indications for partial rib resection in patients with adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation? Spine 18:1593–1598
Helenius I, Remes V, Yrjonen T, Ylikoski M, Schlenzka D, Helenius M, Poussa M (2003) Harrington and Cotrel-Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Joint Surg Am 85-A:2303–2309
King HA, Moe JH, Bradford DS, Winter RB (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 65:1302–1313
Liljenqvist UR, Halm HF, Link TM (1997) Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine 22:2239–2245
Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H (2002) Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J 11:336–343
Lonstein JE, Bradford DS, Winter RB (1995) Moe’s textbook of scoliosis and other spinal deformitiesed. W.B. Saunders Company, Philadelphia
Manning CW, Prime FJ, Zorab PA (1973) Partial costectomy as a cosmetic operation in scoliosis. J Bone Joint Surg Br 55:521–527
Steel HH (1983) Rib resection and spine fusion in correction of convex deformity in scoliosis. J Bone Joint Surg Am 65:920–925
Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 20:1399–1405
Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine 26:2049–2057
Thulbourne T, Gillespie R (1976) The rib hump in idiopathic scoliosis. Measurement, analysis and response to treatment. J Bone Joint Surg Br 58:64–71
Willers U, Transfeldt EE, Hedlund R (1996) The segmental effect of Cotrel-Dubousset instrumentation on vertebral rotation, rib hump and the thoracic cage in idiopathic scoliosis. Eur Spine J 5:387–393
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Min, K., Waelchli, B. & Hahn, F. Primary thoracoplasty and pedicle screw instrumentation in thoracic idiopathic scoliosis. Eur Spine J 14, 777–782 (2005). https://doi.org/10.1007/s00586-005-0977-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-005-0977-4