Abstract
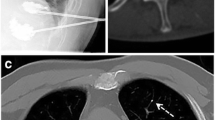
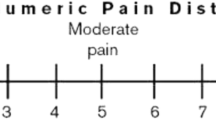
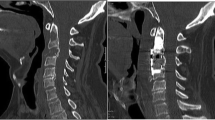
The results of percutaneous vertebroplasty with polymethylmethacrylate (PMMA) of vertebral metastases were evaluated by a retrospective review of a consecutive series of 21 patients, with special reference to functional outcome. Patients complained of vertebral pain in all cases. Walking was impossible for 13 patients. Ten patients presented neurological deficit. Treatment included percutaneous vertebroplasty in all patients, radiotherapy in 15 patients and neural decompression surgery in 3 patients. Mean duration of hospitalization was 14.1 days (range 2–60 days) and the mean follow-up was 5.6 months (range 1–18 months). Preprocedural pain, measured by the visual analog scale (VAS), was 9.1, decreasing to 3.2 after the procedure and 2.8 at the last follow-up visit. Morphinics were discontinued in 7 of 14 patients following discharge from hospital. Ten out of 13 (77%) patients recovered walking capacity. Neurological status improved in three out of five patients. No further vertebral compression occurred in the vertebrae treated. Overall, 81% of the patients in this study were satisfied or very satisfied with the procedure. One patient (5%) had transitory radicular neuritis after the procedure. No major complications were observed. In conclusion, percutaneous vertebroplasty with PMMA proved to be safe and beneficial, providing significant and early improvement in the functional status of patients with spinal metastasis.
Similar content being viewed by others
References
Alvarez L, Perez-Higueras A, Rossi RE, Calvo E (2001) Vertebroplasty in osteoporotic fractures: clinical and radiological results after 5 years. Eur Spine J 10 [Suppl 1]:8
Alvarez L, Pérez-Higueras A (2002) Vertebroplasty: indications and technique (in Spanish). Rev Ortop Traumatol 46:175–182
Argenson C, Cordonnier D, Enkaoua E, Laredo JD, Onimus M, Resbeut M, Saillant G, Viens P, Vital JM (1997) Place de la chirugie dans le traitement des métastases du rachis. Rev Chir Orthop 83 [Suppl III]:109–174
Barr JD, Barr MS, Lemley TJ, McCann RM (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25:923–928
Bünger C, Laursen M, Hansen ES, Neumann P, Christensen FB, Hoy K, Helming P (1999) A new algorithm for the surgical treatment of spinal metastases. Curr Opin Orthop 10:101–105
Chataigner H, Onimus M (2000) Surgery in spinal metastasis without spinal cord compression: indications and strategy related to the risk of recurrence. Eur Spine J 9:523–527
Cortet B, Cotten A, Boutry N, Dewatre F, Flipo RM, Duquesnoy B, Chastanet P, Decalmbre B (1997). Percutaneous vertebroplasty in patients with multiple metastases or multiple myeloma. Rev Rhum Engl Ed 64:177–183
Cotten A, Dewatre F, Cortet B, Assaker R, Leblond D, Duquesnoy B, Chastanet P, Clarisse J (1996) Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methylmethacrylate at clinical follow-up. Radiology 200:525–530
Deramond H, Depriester C, Galibert P, Le Gars D (1998) Percutaneous vertebroplasty with polymethylmethacrylate. Technique, indications and results. Radiol Clin North Am 36:533–546
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ (1969) The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 7:179–192
Gilbert HA, Kagan AR, Nussbaum H, Rao AR, Satzman J, Chan P, Allen Brent, Forsythe A (1977) Evaluation of radiation therapy for bone metastases: pain relief and quality of life. Am J Roentgenol 129:1095–1096
Hammerberg KW (1992) Surgical treatment of metastatic spine disease. Spine 17:1148–1153
Kaemmerlen P, Thiesse P, Bouvard H, Biron P, Mornex F, Jonas P (1989) Percutaneous vertebroplasty in the treatment of metastases. Technique and results. J Radiol 70:557–562
Martin JB, Sugiu JK, San Millan D, Piotin M, Murphy K, Rüfenacht B, Muster M, Rüfenacht DA (1999) Vertebroplasty: clinical experience and follow-up results. Bone 25:11S–15S
Murray JA, Bruels MC, Lindberg RD (1974) Irradiation of poly-methyl-methacrylate: in vitro gamma radiation effect. J Bone Joint Surg Am 56:311–312
Onimus M, Schraub S, Bertin D, Bosset JF, Guidet M (1986) Surgical treatment of vertebral metastases. Spine 11:883–891
Pasca-Moussellard H, Broc G, Pointillart V, Siméon F, Vital JM, Sénégas J (1998) Complications of vertebral metastasis surgery. Eur Spine J 7:438–444
Prié L, Lagarde P, Palussière J, El Ayoubi S, Dilhuydy JM, Durand M, Vital JM, Kantor G (1997) Radiothérapie des métastases vertébrales du cancer du sein. A propos d'une série de 108 patientes. Cancer Radiother 1:234–239
Resbeut M, Alzieu C, Hannounn-Levi JM, Noirclerc M, Cowen D (1997) Place de la chirurgie dans le traitement des métastases du rachis. Radiothérapie des métastases vertébrales. Rev Chir Orthop 83 [Suppl III]:127–130
Sundaresan N, Sachev VP, Holland JF, Moore F, Sung M, Paciucci PA, Wu LT, Kelligher K, Hough L (1995) Surgical treatment of spinal cord compression from epidural metastasis. J Clin Oncol 13:2330–2335
Tokuhashi Y, Matsuzaki H, Toriyama S, Kawano H, Ohsaka S (1990) Scoring system for the operative evaluation of metastatic spine tumor prognosis. Spine 15:1110–1113
Weigel B, Maghsudi M. Neumann C, Kretschmer R, Müller FJ, Nerlich M (1999). Surgical management of symptomatic spinal metastases. Spine 24:2240–2246
Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E (1996). Spinal metastases: indications for and result of percutaneous injection of acrylic surgical cement. Radiology 199:241–247
Acknowledgements
The authors thank JJ Granizo, MD (clinical epidemiologist), for performing the statistical analysis and L Gulliksen for his assistance in correcting the text.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alvarez, L., Pérez-Higueras, A., Quiñones, D. et al. Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life. Eur Spine J 12, 356–360 (2003). https://doi.org/10.1007/s00586-003-0525-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-003-0525-z