Abstract
Purpose
Several technical aspects of the Fick method limit its use intraoperatively. A data-driven modification of the Fick method may enable its use in intraoperative settings.
Methods
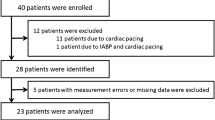
This two-center retrospective observational study included 57 (28 and 29 in each center) patients who underwent off-pump coronary artery bypass graft (OPCAB) surgery. Intraoperative recordings of physiological data were obtained and divided into training and test datasets. The Fick equation was used to calculate cardiac output (CO-Fick) using ventilator-determined variables, intraoperative hemoglobin level, and SvO2, with continuous thermodilution cardiac output (CCO) used as a reference. A modification CO-Fick was derived and validated: CO-Fick-AD, which adjusts the denominator of the original equation.
Results
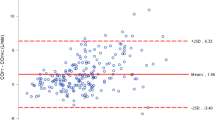
Increased deviation between CO-Fick and CCO was observed when oxygen extraction was low. The root mean square error of CO-Fick was decreased from 6.07 L/min to 0.70 L/min after the modification. CO-Fick-AD showed a mean bias of 0.17 (95% CI 0.00–0.34) L/min, with a 36.4% (95% CI 30.6–44.4%) error. The concordance rates of CO-Fick-AD ranged from 73.3 to 87.1% depending on the time interval and exclusion zone.
Conclusions
The original Fick method is not reliable when oxygen extraction is low, but a modification using data-driven approach could enable continuous estimation of cardiac output during the dynamic intraoperative period with minimal bias. However, further improvements in precision and trending ability are needed.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon a reasonable request.
References
Meng L, Wang Y, Zhang L, McDonagh DL. Heterogeneity and variability in pressure autoregulation of organ blood flow: lessons learned over 100+ years. Crit Care Med. 2019;47:436–48.
Meng L. Heterogeneous impact of hypotension on organ perfusion and outcomes: a narrative review. Br J Anaesth. 2021;127:845–61.
Argueta EE, Paniagua D. Thermodilution cardiac output: a concept over 250 years in the making. Cardiol Rev. 2019;27:138–44.
Drummond KE, Murphy E. Minimally invasive cardiac output monitors. Contin Educ Anaesth Crit Care Pain. 2012;12:5–10.
Nadeau S, Noble WH. Limitations of cardiac output measurements by thermodilution. Can Anaesth Soc J. 1986;33:780–4.
Bootsma IT, Boerma EC, Scheeren TWL, de Lange F. The contemporary pulmonary artery catheter. Part 2: measurements, limitations, and clinical applications. J Clin Monit Comput. 2022;36:17–31.
Medin DL, Brown DT, Wesley R, Cunnion RE, Ognibene FP. Validation of continuous thermodilution cardiac output in critically ill patients with analysis of systematic errors. J Crit Care. 1998;13:184–9.
Sun Q, Rogiers P, Pauwels D, Vincent JL. Comparison of continuous thermodilution and bolus cardiac output measurements in septic shock. Intensive Care Med. 2002;28:1276–80.
Aranada M, Mihm Frederick G, Garrett S, Mihm Megan N, Pearl RG. Continuous cardiac output catheters: delay in in vitro response time after controlled flow changes. Anesthesiology. 1998;89:1592–5.
Lazor MA, Pierce ET, Stanley GD, Cass JL, Halpern EF, Bode RH Jr. Evaluation of the accuracy and response time of STAT-mode continuous cardiac output. J Cardiothorac Vasc Anesth. 1997;11:432–6.
Siegel LC, Hennessy MM, Pearl RG. Delayed time response of the continuous cardiac output pulmonary artery catheter. Anesth Analg. 1996;83:1173–7.
Seely RD, Nerlich WE, Gregg DE. A comparison of cardiac output determined by the fick procedure and a direct method using the rotameter. Circulation. 1950;1:1261–6.
Visscher MB, Johnson JA. The fick principle: analysis of potential errors in its conventional application. J Appl Physiol. 1985;1953(5):635–8.
Light RB. Intrapulmonary oxygen consumption in experimental pneumococcal pneumonia. J Appl Physiol. 1985;1988(64):2490–5.
Lin SY, Chang FC, Lin JR, Chou AH, Tsai YF, Liao CC, Tsai HI, Chen CY. Increased FIO2 influences SvO2 interpretation and accuracy of Fick-based cardiac output assessment in cardiac surgery patients: a prospective randomized study. Medicine (Baltimore). 2021;100: e27020.
Lee HC, Jung CW. Vital Recorder-a free research tool for automatic recording of high-resolution time-synchronised physiological data from multiple anaesthesia devices. Sci Rep. 2018;8:1527.
Truijen J, Westerhof BE, Kim YS, Stok WJ, de Mol BA, Preckel B, Hollmann MW, van Lieshout JJ. The effect of haemodynamic and peripheral vascular variability on cardiac output monitoring: thermodilution and non-invasive pulse contour cardiac output during cardiothoracic surgery. Anaesthesia. 2018;73:1489–99.
Montenij LJ, Buhre WF, Jansen JR, Kruitwagen CL, de Waal EE. Methodology of method comparison studies evaluating the validity of cardiac output monitors: a stepwise approach and checklist. Br J Anaesth. 2016;116:750–8.
Carrasco JL, King TS, Chinchilli VM. The concordance correlation coefficient for repeated measures estimated by variance components. J Biopharm Stat. 2009;19:90–105.
Zou GY. Confidence interval estimation for the Bland-Altman limits of agreement with multiple observations per individual. Stat Methods Med Res. 2013;22:630–42.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91.
Critchley LA, Lee A, Ho AMH. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Kouz K, Michard F, Bergholz A, Vokuhl C, Briesenick L, Hoppe P, Flick M, Schön G, Saugel B. Agreement between continuous and intermittent pulmonary artery thermodilution for cardiac output measurement in perioperative and intensive care medicine: a systematic review and meta-analysis. Crit Care. 2021;25:125.
Peyton PJ, Chong SW. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology. 2010;113:1220–35.
Saugel B, Hoppe P, Nicklas JY, Kouz K, Körner A, Hempel JC, Vos JJ, Schön G, Scheeren TWL. Continuous noninvasive pulse wave analysis using finger cuff technologies for arterial blood pressure and cardiac output monitoring in perioperative and intensive care medicine: a systematic review and meta-analysis. Br J Anaesth. 2020;125:25–37.
Kusaka Y, Ohchi F, Minami T. Evaluation of the fourth-generation FloTrac/Vigileo system in comparison with the intermittent bolus thermodilution method in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2019;33:953–60.
Maeda T, Hamaguchi E, Kubo N, Shimokawa A, Kanazawa H, Ohnishi Y. The accuracy and trending ability of cardiac index measured by the fourth-generation FloTrac/Vigileo system™ and the Fick method in cardiac surgery patients. J Clin Monit Comput. 2019;33:767–76.
de Lange F, Bootsma IT, Boerma EC. Letter to the editor in response to “Agreement between continuous and intermittent pulmonary artery thermodilution for cardiac output measurement in perioperative and intensive care medicine: a systematic review and meta-analysis.” Crit Care. 2021;25:215.
Nakanishi N, Yoshioka T, Okano Y, Nishimura T. Continuous Fick cardiac output measurement during exercise by monitoring of mixed venous oxygen saturation and oxygen uptake. Chest. 1993;104:419–26.
Hoeper MM, Maier R, Tongers J, Niedermeyer J, Hohlfeld JM, Hamm M, Fabel H. Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med. 1999;160:535–41.
Liao R, Li J, Liu J. Volatile induction/maintenance of anaesthesia with sevoflurane increases jugular venous oxygen saturation and lumbar cerebrospinal fluid pressure in patients undergoing craniotomy. Eur J Anaesthesiol. 2010;27:369–76.
Jeong H, Jeong S, Lim Hoi J, Lee J, Yoo KY. Cerebral oxygen saturation measured by near-infrared spectroscopy and jugular venous bulb oxygen saturation during arthroscopic shoulder surgery in beach chair position under sevoflurane-nitrous oxide or propofol-remifentanil anesthesia. Anesthesiology. 2012;116:1047–56.
Barker SJ, Shander A, Ramsay MA. Continuous noninvasive hemoglobin monitoring: a measured response to a critical review. Anesth Analg. 2016;122:565–72.
Ritchie-McLean S, Shankar R. Calculating oxygen consumption during low-flow anaesthesia. Anaesthesia. 2017;72:789.
Acknowledgements
Sincere appreciation to Dr. Sangil Park and Prof. Jin-Tae Kim for their precious guidance and invaluable advice.
Funding
This research was supported by a research fund of Chungnam National University and a research fund of Chungnam National University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Oh, C., Lee, HC., Lee, S. et al. Continuous cardiac output estimation using a new modified Fick method during off-pump coronary artery bypass graft surgery: a retrospective observational study. J Anesth 38, 1–9 (2024). https://doi.org/10.1007/s00540-023-03260-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03260-x