Abstract
Purpose
Several studies indicate that assisted reproductive technology (ART) including in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) pregnancies carries increased risk of complications including postpartum hemorrhage (PPH). However, the association between IVF/ICSI and the bleeding risk particularly in cesarean delivery has not been systematically assessed. The aim of this study was to evaluate bleeding risk during and after cesarean delivery in parturients who conceived using IVF or ICSI.
Methods
This is a retrospective observational study analyzing data from 310 parturients who underwent cesarean delivery: 155 who had conceived using IVF or ICSI (IVF/ICSI group) and 155 age and year of delivery matched controls who had conceived spontaneously (control group). The primary outcome measure was the amount of blood lost during and within 24 h after cesarean delivery. Secondary outcome measure was the incidence of severe PPH. With 132 parturients in each group, we had 90% power to detect a 200 mL difference in the bleeding amount, at a 0.05 two-sided significance level.
Results
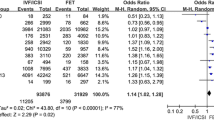
The amount of bleeding in the IVF/ICSI group was 1234 ± 669 mL, which was 124 mL (11.2%) greater than that in the control group (95% CI − 34 to 282; p = 0.12). The incidence of severe PPH in the IVF/ICSI group and in the control group was 23.9% and 16.8%, respectively (p = 0.16), and the unadjusted odds ratio was 1.6 (95% CI, 0.9–2.7; p = 0.12). No significant independent effect of IVF/ICSI on the bleeding amount and the incidence of severe PPH was observed in multivariable regression analyses (p = 0.22, p = 0.16).
Conclusion
In this study, IVF and ICSI were not associated with increasing risk of bleeding in cesarean delivery.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author MA.
References
Chambers GM, Dyer S, Zegers-Hochschild F, de Mouzon J, Ishihara O, Banker M, Mansour R, Kupka MS, Adamson GD. International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology, 2014. Hum Reprod. 2021;36:2921–34. https://doi.org/10.1093/humrep/deab198.
Qin J, Liu X, Sheng W, Wang H, Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta analysis of cohort studies. Fertil Steril. 2016;105:73–85. https://doi.org/10.1016/j.fertnstert.2015.09.007.
Nyfløt LT, Sandven I, Oldereid NB, Stray-Pedersen B, Vangen S. Assisted reproductive technology and severe postpartum haemorrhage: a case-control study. BJOG. 2017;124:1198–205. https://doi.org/10.1111/1471-0528.14471.
Vannuccini S, Ferrata C, Perelli F, Pinzauti S, Severi FM, Reis FM, Petraglia F, Di Tommaso M. Peripartum and postpartum outcomes in uncomplicated term pregnancy following ART: a retrospective cohort study from two Italian obstetric units. Hum Reprod Open. 2018;2018:hoy012. https://doi.org/10.1093/hropen/hoy012.
Slavov S, Ingilizova G, Yaneva G. Analysis of delivery in singleton pregnancies achieved by in vitro fertilization. Open Access Maced J Med Sci. 2021;9:885–9. https://doi.org/10.3889/oamjms.2021.6705.
Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anesth Analg. 2010;110:1368–73. https://doi.org/10.1213/ANE.0b013e3181d74898.
Chang CC, Wang IT, Chen YH, Lin HC. Anesthetic management as a risk factor for postpartum hemorrhage after cesarean deliveries. Am J Obstet Gynecol. 2011;205(462):e1-7. https://doi.org/10.1016/j.ajog.2011.06.068.
Sei K, Masui K, Sasa H, Furuya K. Size of uterine leiomyoma is a predictor for massive haemorrhage during caesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2018;223:60–3. https://doi.org/10.1016/j.ejogrb.2018.02.014.
Bienstock JL, Eke AC, Hueppchen NA. Postpartum Hemorrhage. N Engl J Med. 2021;384:1635–45. https://doi.org/10.1056/NEJMra1513247.
Vlahos NF, Theodoridis TD, Partsinevelos GA. Myomas and adenomyosis: impact on reproductive outcome. Biomed Res Int. 2017;2017:5926470. https://doi.org/10.1155/2017/5926470.
Grabarz A, Ghesquière L, Debarge V, Ramdane N, Delporte V, Bodart S, Deruelle P, Subtil D, Garabedian C. Cesarean section complications according to degree of emergency during labour. Eur J Obstet Gynecol Reprod Biol. 2021;256:320–5. https://doi.org/10.1016/j.ejogrb.2020.11.047.
Healy DL, Breheny S, Halliday J, Jaques A, Rushford D, Garrett C, Talbot JM, Baker HW. Prevalence and risk factors for obstetric haemorrhage in 6730 singleton births after assisted reproductive technology in Victoria Australia. Hum Reprod. 2010;25:265–74. https://doi.org/10.1093/humrep/dep376.
Noguchi S, Murakoshi T, Konno H, Matsushita M, Matsumoto M. Embryo transfer is a risk factor for severe postpartum hemorrhage and blood transfusion requirement. J Matern Fetal Neonatal Med. 2017;32:879–82. https://doi.org/10.1080/14767058.2017.1394288.
Nyfløt LT, Sandven I, Stray-Pedersen B, Silje P, Al-Zirqi I, Rosenberg M, Jacobsen AF, Vangen S. Risk factors for severe postpartum hemorrhage: a case-control study. BMC Pregnancy Childbirth. 2017;17:17. https://doi.org/10.1186/s12884-016-1217-0.
Neary C, Naheed S, McLernon DJ, Black M. Predicting risk of postpartum haemorrhage: a systematic review. BJOG. 2021;128:46–53. https://doi.org/10.1111/1471-0528.16379.
Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjaerven R, Vatten LJ. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Hum Reprod. 2006;21:2353–8. https://doi.org/10.1093/humrep/del153.
Nakamura Y, Yaguchi C, Itoh H, Sakamoto R, Kimura T, Furuta N, Uchida T, Tamura N, Suzuki K, Sumimoto K, Matsuda Y, Matsuura T, Nishimura M, Kanayama N. Morphologic characteristics of the placental basal plate in in vitro fertilization pregnancies: a possible association with the amount of bleeding in delivery. Hum Pathol. 2015;46:1171–9. https://doi.org/10.1016/j.humpath.2015.04.007.
Takahashi H, Tanaka H, Osuga Y, Miura K, Saito S, Sato S, Sugawara J, Ide S, Koh I, Yamauchi K, Okuyama A, Okuno K, Kuwata T, Fujieda S, Ikeda T. Retained products of conception (RPOC) following delivery without placenta previa: Which patients with RPOC show postpartum hemorrhage? Placenta. 2022;124:12–7. https://doi.org/10.1016/j.placenta.2022.05.004.
Fujita K, Ushida T, Imai K, Nakano-Kobayashi T, Iitani Y, Seiko M, Yoshida S, Yamashita M, Kajiyama H, Kotani T. Manual removal of the placenta and postpartum hemorrhage: a multicenter retrospective study. J Obstet Gyenaecol Res. 2021;47:3867–74. https://doi.org/10.1111/jog.15004.
Committee on Obstetric Practice. Quantitative blood loss in obstetric hemorrhage: ACOG COMMITTEE OPINION, Number 794. Obstet Gynecol. 2019;134:e150–6. https://doi.org/10.1097/AOG.0000000000003564.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Aizawa, M., Ishihara, S. & Yokoyama, T. Singleton pregnancy using in vitro fertilization or intracytoplasmic sperm injection does not increase risk of bleeding in cesarean delivery: a retrospective cohort study. J Anesth 37, 769–774 (2023). https://doi.org/10.1007/s00540-023-03234-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03234-z