Abstract
Purpose
Nurses routinely assess respiration of hospitalized children; however, respiratory rate measurements are technically difficult due to rapid and small chest wall movements. The aim of this study is to reveal the respiratory status of small children undergoing minor surgery with load cells placed under the bed legs, and to test the hypothesis that respiratory rate (primary variable) is slower immediately after arrival to the ward and recovers in 2 h.
Methods
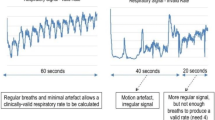
Continuous recordings of the load cell signals were performed and stable respiratory waves within the 10 discriminative perioperative timepoints were used for respiratory rate measurements. Apnea frequencies were calculated at pre and postoperative nights and 2 h immediately after returning to the ward after surgery.
Results
Continuous recordings of the load cell signals were successfully performed in 18 children (13 to 119 months). Respiratory waves were appraisable for more than 70% of nighttime period and 40% of immediate postoperative period. There were no statistically significant differences of respiratory rate in any timepoint comparisons (p = 0.448), thereby not supporting the study hypothesis. Respiratory rates changed more than 5 breaths per minute postoperatively in 5 out of 18 children (28%) while doses of fentanyl alone did not explain the changes. Apnea frequencies significantly decreased 2 h immediately after returning to the ward and during the operative night compared to the preoperative night.
Conclusion
Respiratory signal extracted from load cell sensors under the bed legs successfully revealed various postoperative respiratory pattern change in small children undergoing minor surgery.
Clinical Trail Registration: UMIN (University Hospital Information Network) Clinical Registry: UMIN000045579 (https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000052039).









Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mamie C, Habre W, Delhumeau C, Argiroffo CB, Morabia A. Incidence and risk factors of perioperative respiratory adverse events in children undergoing elective surgery. Paediatr Anaesth. 2004;14:218–24.
Tait AR, Malviya S, Voepel-Lewis T, Munro HM, Siewert M, Pandit UA. Risk factors for perioperative adverse respiratory events in children with upper respiratory tract infections. Anesthesiology. 2001;95:299–306.
Von Ungern-Sternberg BS, Boda K, Chambers NA, Rebmann C, Johnson C, Sly PD, Habre W. Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study. Lancet. 2010;376:773–83.
Wudineh DM, Berhe YW, Chekol WB, Adane H, Workie MM. Perioperative respiratory adverse events among pediatric surgical patients in university hospitals in northwest Ethiopia. A prospective observational study. Front Pediatr. 2022;10:1–9.
Chung F, Wong J, Mestek ML, Niebel KH, Lichtenthal P. Characterization of respiratory compromise and the potential clinical utility of capnography in the post-anesthesia care unit: a blinded observational trial. J Clin Monit Comput. 2020;34:541–51.
Ginsburg AS, Lenahan JL, Izadnegahdar R, Ansermino JM. A systematic review of tools to measure respiratory rate in order to identify childhood pneumonia. Am J Respir Crit Care Med. 2018;197:1116–27.
Roback K, Nelson N, Johansson A, Hass U, Strömberg T. A new fiberoptical respiratory rate monitor for the neonatal intensive care unit. Pediatr Pulmonol. 2005;39:120–6.
Bonafide CP, Brady PW, Keren R, Conway PH, Marsolo K, Daymont C. Development of heart and respiratory rate percentile curves for hospitalized children. Pediatrics. 2013;131:1150–7.
Christensen RE, Haydar B, Voepel-Lewis TD. Pediatric cardiopulmonary arrest in the postanesthesia care unit, rare but preventable: analysis of data from wake up safe, the pediatric anesthesia quality improvement initiative. Anesth Analg. 2017;124:1231–6.
Al-Khalidi FQ, Saatchi R, Burke D, Elphick H, Tan S. Respiration rate monitoring methods: a review. Pediatr Pulmonol. 2011;46:523–9.
Patino M, Kalin M, Griffin A, Minhajuddin A, Ding L, Williams T, Ishman S, Mahmoud M, Kurth CD, Szmuk P. Comparison of postoperative respiratory monitoring by acoustic and transthoracic impedance technologies in pediatric patients at risk of respiratory depression. Anesth Analg. 2017;124:1937–42.
Brown KA, Aoude AA, Galiana HL, Kearney RE. Automated respiratory inductive plethysmography to evaluate breathing in infants at risk for postoperative apnea. Can J Anesth. 2008;55:739–47.
Isono S, Nozaki-Taguchi N, Hasegawa M, Kato S, Todoroki S, Masuda S, Iida N, Nishimura T, Noto M, Sato Y. Contact-free unconstraint respiratory measurements with load cells under the bed in awake healthy volunteers: breath-by-breath comparison with pneumotachography. J Appl Physiol. 2019;126:1432–41.
Schaefer MS, Eikermann M. Contact-free respiratory monitoring using bed wheel sensors: a valid respiratory monitoring technique with significant potential impact on public health. J Appl Physiol. 2019;126:1430–1.
Hasegawa M, Nozaki-Taguchi N, Shono K, Mizuno Y, Takai H, Sato Y, Isono S. Effects of opioids on respiration assessed by a contact-free unconstraint respiratory monitor with load cells under the bed in patients with advanced cancer. J Appl Physiol. 2021;130:1743–53.
Lee WK, Yoon H, Han C, Joo KM, Park KS. Physiological signal monitoring bed for infants based on load-cell sensors. Sensors (Switzerland). 2016;16:409.
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012; 8(5):597–619.
Pattinson KTS. Opioids and the control of respiration. Br J Anaesth. 2008;100:747–58.
Mellen NM, Janczewski WA, Bocchiaro CM, Feldman JL. Opioid-induced quantal slowing reveals dual networks for respiratory rhythm generation. Neuron. 2003;37:821–6.
Zhang Z, Xu F, Zhang C, Liang X. Activation of opioid μ receptors in caudal medullary raphe region inhibits the ventilatory response to hypercapnia in anesthetized rats. Anesthesiology. 2007;107:288–97.
Sarton E, Dahan A, Teppema L, Van den Elsen M, Olofsen E, Berkenbosch A, Van Kleef J. Acute pain and central nervous system arousal do not restore impaired hypoxic ventilatory response during sevoflurane sedation. Anesthesiology. 1996;85:295–303.
Borgbjerg FM, Nielsen K, Franks J. Experimental pain stimulates respiration and attenuates morphine-induced respiratory depression: A controlled study in human volunteers. Pain. 1996;64:123–8.
Nishino T, Hiraga K, Fujisato M, Mizuguchi T, Honda Y. Breathing patterns during postoperative analgesia in patients after lower abdominal operations. Anesthesiology. 1988;69:967–72.
Cozowicz C, Memtsoudis SG. Perioperative management of the patient with obstructive sleep apnea: a narrative review. Anesth Analg. 2021;132:1231–43.
Bauchat JR, Weiniger CF, Sultan P, Habib AS, Ando K, Kowalczyk JJ, Kato R, George RB, Palmer CM, Carvalho B. Society for obstetric anesthesia and perinatology consensus statement: monitoring recommendations for prevention and detection of respiratory depression associated with administration of neuraxial morphine for cesarean delivery analgesia. Anesth Analg. 2019;129:458–74.
Combes X, Cerf C, Bouleau D, Duvaldestin P, Dhonneur G. The effects of residual pain on oxygenation and breathing pattern during morphine analgesia. Anesth Analg. 2000;90:156–60.
Cavalcante AN, Sprung J, Schroeder DR, Weingarten TN. Multimodal analgesic therapy with gabapentin and its association with postoperative respiratory depression. Anesth Analg. 2017;125:141–6.
Ray DC, Drummond GB. Continuous intravenous morphine for pain relief after abdominal surgery. Ann R Coll Surg Engl. 1988;70:317–21.
Fechtner L, El AM, Sattar A, Moore M, Strohl KP. Fentanyl effects on breath generation in C57BL/6J and A/J mouse strains. Respir Physiol Neurobiol. 2015;215:20–9.
Hayashida M, Nagashima M, Satoh Y, Katoh R, Tagami M, Ide S, Kasai S, Nishizawa D, Ogai Y, Hasegawa J, Komatsu H, Sora I, Fukuda K, Koga H, Hanaoka K, Ikeda K. Analgesic requirements after major abdominal surgery are associated with OPRM1 gene polymorphism genotype and haplotype. Pharmacogenomics. 2008;9:1605–16.
Wang D, Yee BJ, Grunstein RR, Chung F. Chronic opioid use and central sleep apnea, where are we now and where to go? A state of the art review. Anesth Analg. 2021;132:1244–53.
Chung F, Liao P, Yegneswaran B, Shapiro CM, Kang W. Postoperative changes in sleep-disordered breathing and sleep architecture in patients with obstructive sleep apnea. Anesthesiology. 2014;120:287–98.
Jordan AS, O’Donoghue FJ, Cori JM, Trinder J. Physiology of arousal in obstructive sleep apnea and potential impacts for sedative treatment. Am J Respir Crit Care Med. 2017;196:814–21.
Nozaki-Taguchi N, Nishino T. Depression of sighing in the first three postoperative days with epidural morphine analgesia. J Anesth. 1994;8:415–9.
Brown K, Bates JHT. Post sigh apnoea represents the majority of central apnoea in infants at risk for postoperative apnoea. Pediatr Anesth. 2000;10:696.
Zhang Z, Xu F, Zhang C, Liang X. Activation of opioid μ-receptors in medullary raphe depresses sighs. Am J Physiol - Regul Integr Comp Physiol. 2009;296:1528–37.
Bell HJ, Pankuch G. Augmented breaths ('sighs’) are suppressed by morphine in a dose-dependent fashion via naloxone-sensitive pathways in adult rats. Respir Physiol Neurobiol. 2013;185:296–303.
Kallioinen N, Hill A, Christofidis MJ, Horswill MS, Watson MO. Quantitative systematic review: sources of inaccuracy in manually measured adult respiratory rate data. J Adv Nurs. 2021;77:98–124.
Cardona-Morrell M, Prgomet M, Lake R, Nicholson M, Harrison R, Long J, Westbrook J, Braithwaite J, Hillman K. Vital signs monitoring and nurse-patient interaction: a qualitative observational study of hospital practice. Int J Nurs Stud. 2015;56:9–16.
McGain F, Cretikos MA, Jones D, van Dyk S, Buist MD, Opdam H, Pellegrino V, Robertson MS, Bellomo R. Documentation of clinical review and vital signs after major surgery. Med J Aust. 2008;189:380–3.
Chen J, Hillman K, Bellomo R, Flabouris A, Finfer S, Cretikos M. The impact of introducing medical emergency team system on the documentations of vital signs. Resuscitation. 2009;80:35–43.
Shah SA, Fleming S, Thompson M, Tarassenko L. Respiratory rate estimation during triage of children in hospitals. J Med Eng Technol. 2015;39:514–24.
Sefton G, Lane S, Killen R, Black S, Lyon M, Ampah P, Sproule C, Loren-Gosling D, Richards C, Spinty J, Holloway C, Davies C, Wilson A, Chean CS, Carter B, Carro ED. Accuracy and efficiency of recording pediatric early warning scores using an electronic physiological surveillance system compared with traditional paper-based documentation. CIN - Comput Informatics Nurs. 2017;35:228–36.
Acknowledgements
Sara Shimizu M.D. (Shimizu Orthopedic Plastic Surgery Clinic, Tokyo, Japan) greatly helped to improve this manuscript.
Funding
This study was supported by JSPS KAKENHI Grant number 19K18262 (the primary investigator; Dr. Hateruma). This work was performed at Chiba University Hospital, Chiba, Japan. Textual similarities: Similarity Index 5% by iThenticate (May 10, 2022).
Author information
Authors and Affiliations
Contributions
Study design: YH, YS, KT, NN, SI. Data collection: YH, SK, KS. Data analysis: YH, SI. Statistical analysis and advice: YH, NN, SI, YS. Writing up the draft of the manuscript: YH, NN, SK, KT, KS, YS, SI. Approval of the final version: YH, NN, SK, KT, KS, YS, SI.
Corresponding author
Ethics declarations
Conflict of interest
This study used data obtained during a collaborative research between Chiba University and MinebeaMitsumi Inc.. Shiroh Isono received scholarship donations from MinebeaMitsumi Inc. as a head of Department of Anesthesiology, Chiba University. Shiroh Isono is one of the inventors of the vital sign monitoring system used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hateruma, Y., Nozaki-Taguchi, N., Son, K. et al. Assessments of perioperative respiratory pattern with non-contact vital sign monitor in children undergoing minor surgery: a prospective observational study. J Anesth 37, 714–725 (2023). https://doi.org/10.1007/s00540-023-03223-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03223-2