Abstract
Purpose
The main aim of the current trial was to explore our hypothesis that cooling head wraps lower the core temperature more effectively than ice packs on the head during forced-air warming after pediatric cardiac surgeries.
Methods
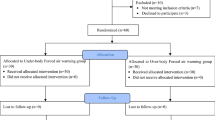
This study was a single-center Randomized Controlled Trial. Participants were children with a weight ≤ 10 kg and hyperthermia during forced-air warming after cardiac surgeries. When the core temperature reached 37.5 °C, ice packs on the head (group C) or a cooling head wrap (group H) were used as cooling devices to decrease the core temperature. The primary outcome was the core temperature. The secondary outcomes were the foot surface temperature and heart rate. We measured all outcomes every 30 min for 240 min after the patient developed hyperthermia. We conducted two-way ANOVA as a pre-planned analysis and also the Bonferroni test as a post hoc analysis.
Results
Twenty patients were randomly assigned to groups C and H. The series of core temperatures in group H were significantly lower than those in group C (p < 0.0001), and post hoc analysis showed that there was no significant difference in core temperatures at T0 between the two groups and statistically significant differences in all core temperatures at T30-240 between the two groups. There was no difference between the two groups’ surface temperatures and heart rates.
Conclusions
Compared to ice packs on the head, head cooling wraps more effectively suppress core temperature elevation during forced-air warming after pediatric cardiac surgery.




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Savard GK, Cooper KE, Veale WL, Malkinson TJ. Peripheral blood flow during rewarming from mild hypothermia in humans. J Appl Physiol. 1985;1985(58):4–13.
Inoue Y, Ichinose-Kuwahara T, Nakamura S, Ueda H, Yasumatsu H, Kondo N, Araki T. Cutaneous vasodilation response to a linear increase in air temperature from 28 degrees C to 40 degrees C in prepubertal boys and young men. J Physiol Anthropol. 2009;28:137–44.
Zhang R, Chen X, Xiao Y. The effects of a forced-air warming system plus electric blanket for elderly patients undergoing transurethral resection of the prostate: a randomized controlled trial. Medicine (Baltimore). 2018;97:e13119.
Tharakan JA, Sukulal K. Post cardiac surgery junctional ectopic tachycardia: a ‘Hit and Run’ tachyarrhythmia as yet unchecked. Ann Pediatr Cardiol. 2014;7:25–8.
Li J, Schulze-Neick I, Lincoln C, Shore D, Scallan M, Bush A, Redington AN, Penny DJ. Oxygen consumption after cardiopulmonary bypass surgery in children: determinants and implications. J Thorac Cardiovasc Surg. 2000;119:525–33.
Triffterer L, Marhofer P, Sulyok I, Keplinger M, Mair S, Steinberger M, Klug W, Kimberger O. Forced-air warming during pediatric surgery: a randomized comparison of a compressible with a noncompressible warming system. Anesth Analg. 2016;122:219–25.
Tibby SM, Hatherill M, Murdoch IA. Capillary refill and core-peripheral temperature gap as indicators of haemodynamic status in paediatric intensive care patients. Arch Dis Child. 1999;80:163–6.
Balaji S, Sullivan I, Deanfield J, James I. Moderate hypothermia in the management of resistant automatic tachycardias in children. Br Heart J. 1991;66:221–4.
Lemyre B, Chau V. Hypothermia for newborns with hypoxic-ischemic encephalopathy. Paediatr Child Health. 2018;23:285–91.
Sarkar S, Barks JD, Bhagat I, Donn SM. Effects of therapeutic hypothermia on multiorgan dysfunction in asphyxiated newborns: whole-body cooling versus selective head cooling. J Perinatol. 2009;29:558–63.
Walker HK, Hall WD, Hurst JW, editors. Clinical methods: the history, physical, and laboratory examinations. 3rd ed. Boston: Butterworths; 1990.
Kimura S, Butt W. Core-peripheral temperature gradient and skin temperature as predictors of major adverse events among postoperative pediatric cardiac patients. J Cardiothorac Vasc Anesth. 2022;36:690–8.
Gupta AK, Singh VK, Varma A. Approach to postoperative fever in pediatric cardiac patients. Ann Pediatr Cardiol. 2012;5(1):61–8.
Koehn J, Kollmar R, Cimpianu CL, Kallmünzer B, Moeller S, Schwab S, Hilz MJ. Head and neck cooling decreases tympanic and skin temperature, but significantly increases blood pressure. Stroke. 2012;43:2142–8.
Kussman BD, Wypij D, DiNardo JA, Newburger JW, Mayer JE Jr, del Nido PJ, Bacha EA, Pigula F, McGrath E, Laussen PC. Cerebral oximetry during infant cardiac surgery: evaluation and relationship to early postoperative outcome. Anesh Analg. 2009;108:1122–31.
Dalrymple-Hay MJ, Deakin CD, Knight H, Edwards JC, Keeton B, Salmon AP, Monro JL. Induced hypothermia as salvage treatment for refractory cardiac failure following paediatric cardiac surgery. Eur J Cardiothorac Surg. 1999;15:515–8.
Sarkar S, Barks JD, Bhagat I, Dechert R, Donn SM. Pulmonary dysfunction and therapeutic hypothermia in asphyxiated newborns: whole body versus selective head cooling. Am J Perinatol. 2009;26:265–70.
Davies P, Maconochie I. The relationship between body temperature, heart rate and respiratory rate in children. Emerg Med J. 2009;26:641–3.
Kirschen GW, Singer DD, Thode HC Jr, Singer AJ. Relationship between body temperature and heart rate in adults and children: a local and national study. Am J Emerg Med. 2020;38:929–33.
Kabbani MS, Al Taweel H, Kabbani N, Al Ghamdi S. Critical arrhythmia in postoperative cardiac children: recognition and management. Avicenna J Med. 2017;7:88–95.
Ross J Jr, Miura T, Kambayashi M, Eising GP, Ryu KH. Adrenergic control of the force-frequency relation. Circulation. 1995;92:2327–32.
Elstad M, Liu X, Thoresen M. Heart rate response to therapeutic hypothermia in infants with hypoxic-ischaemic encephalopathy. Resuscitation. 2016;106:53–7.
Hilz MJ, Stemper B, Sauer P, Haertl U, Singer W, Axelrod FB. Cold face test demonstrates parasympathetic cardiac dysfunction in familial dysautonomia. Am J Physiol. 1999;276:R1833–9.
Khurana RK, Watabiki S, Hebel JR, Toro R, Nelson E. Cold face test in the assessment of trigeminal-brainstem-vagal function in humans. Ann Neurol. 1980;7:144–9.
Lauri T, Leskinen M, Timisjärvi J, Hirvonen L. Cardiac function in hypothermia. Arctic Med Res. 1991;50:63–6.
van Veelen MJ, Brodmann MM. Hypothermia in trauma. Int J Environ Res Public Health. 2021;18:8719.
Guvakov DV, Cheung AT, Weiss SJ, Kalinin NB, Fedorenko NO, Shunkin AV, Lomivorotov VN, Karaskov AM. Effectiveness of forced air warming after pediatric cardiac surgery employing hypothermic circulatory arrest without cardiopulmonary bypass. J Clin Anesth. 2000;12:519–24.
Topjian A, Hutchins L, DiLiberto MA, Abend NS, Ichord R, Helfaer M, Berg RA, Nadkarni V. Induction and maintenance of therapeutic hypothermia after pediatric cardiac arrest: efficacy of a surface cooling protocol. Pediatr Crit Care Med. 2011;12:e127–135.
Gibbison B, Villalobos Lizardi JC, Avilés Martínez KI, Fudulu DP, Medina Andrade MA, Pérez-Gaxiola G, Schadenberg AW, Stoica SC, Lightman SL, Angelini GD, Reeves BC. Prophylactic corticosteroids for paediatric heart surgery with cardiopulmonary bypass. Cochrane Database Syst Rev. 2020;10:CD013101.
Fromy B, Josset-Lamaugarny A, Aimond G, Pagnon-Minot A, Marics I, Tattersall GJ, Moqrich A, Sigaudo-Roussel D. Disruption of TRPV3 impairs heat-evoked vasodilation and thermoregulation: a critical role of CGRP. J Invest Dermatol. 2018;138:688–96.
Bräuer A, English MJ, Steinmetz N, Lorenz N, Perl T, Weyland W, Quintel M. Efficacy of forced-air warming systems with full body blankets. Can J Anaesth. 2007;54:34–41.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
WS: This author served as the global chief investigator for this study, designed the study, analyzed and interpreted the data, and drafted the manuscript. TC: This author designed the study, helped with experiments, analyzed and interpreted the data, revised the work critically, and proofread the manuscript draft. YN: This author designed the work, helped with the experiments, interpreted the data, and revised the work critically. TO: This author designed the study, helped with clinical management, interpreted the data, and revised the study critically. YI: This author designed the study, helped with clinical management, interpreted the data, and revised the study critically. TN: This author designed the study, helped with clinical management, interpreted the data, and revised the study critically. HA: This author designed the study, helped with clinical management, interpreted the data, and revised the study critically. NE: This author designed the study, helped with clinical management, interpreted the data, and revised the study critically. JO: This author designed the study, helped with clinical management, interpreted the data, and revised the study critically. MY: This author designed the study, acquired the work, analyzed and interpreted the data, and revised the study critically. WS, TC, YN, TO, YI, TN, HA, NE, JO, and MY drafted the study, approved the final version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work was appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Ethical approval
The study was approved by the ethics committee of the Hokkaido Medical Center for Child Health and Rehabilitation (Trial ID:42-4). The trial was registered in the jRCT Clinical Trial Registry (ID: jRCT1012210039, URL: https://rctportal.niph.go.jp/en/detail?trial_id=jRCT1012210039, principal investigator’s name: Wataru Sakai, registration day: October 13, 2021) and performed in accordance with the Declaration of Helsinki after approval from the ethics committee.
Consent to participate
Written consent was obtained from the parents of the participating patients.
Consent for publication
Written consent was obtained from the parents of the participating patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Sakai, W., Chaki, T., Nawa, Y. et al. Head cooling wrap could suppress the elevation of core temperature after cardiac surgery during forced-air warming in a pediatric intensive care unit: a randomized clinical trial. J Anesth 37, 596–603 (2023). https://doi.org/10.1007/s00540-023-03210-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03210-7