Abstract
Purpose
This study aimed to identify the incidence and risk factors of early post-operative cognitive dysfunction (POCD) in middle-aged patients undergoing cardiac surgery.
Methods
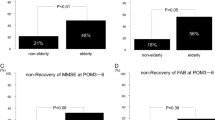
Data were examined retrospectively from 71 patients aged 46–64 years who underwent elective cardiac surgery. Magnetic resonance imaging (MRI) and MR angiography were obtained preoperatively to assess prior cerebral infarctions, carotid artery stenosis, and intracranial arterial stenosis. Patients also completed six neuropsychological tests of memory, attention, and executive function before and after surgery. Mild cognitive impairment (MCI) was defined as performance 1.5 standard deviations (SD) below the population means on any neurocognitive battery, whereas POCD was defined as a decrease of 1 SD population means on at least two in the test battery. Patient characteristics were analyzed using univariate analysis, and independent predictors were analyzed using multivariate logistic regression analysis.
Results
After surgery, 25 patients (35%) were assessed with POCD. Patients with POCD had significantly higher rates of preoperative MCI and cerebral infarcts on MRI. Multivariate logistic regression analysis identified preoperative MCI and cerebral infarctions detected by MRI as a predictor of POCD.
Conclusion
More than one-third of middle-aged patients undergoing cardiac surgery developed POCD. Our findings suggested preoperative MCI and infarcts detected by MRI were risk factors for POCD in these middle-aged patients.
Similar content being viewed by others
Data Availability
The data that support the fndings of this report are available from the corresponding author, N.H., upon reasonable request.
References
Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, Gravenstein JS. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108(1):18–30.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344(6):395–402.
Newman MF, Grocott HP, Mathew JP, White WD, Landolfo K, Reves JG, Laskowitz DT, Mark DB, Blumenthal JA. Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke. 2001;32(12):2874–81.
Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS, ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110(3):548–55.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303–8.
Lopez OL, Kuller LH, Becker JT, Dulberg C, Sweet RA, Gach HM, Dekosky ST. Incidence of dementia in mild cognitive impairment in the cardiovascular health study cognition study. Arch Neurol. 2007;64(3):416–20.
Petersen RC, Roberts RO, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, Smith GE, Jack CR. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66(12):1447–55.
Lu Y, Liu C, Yu D, Fawkes S, Ma J, Zhang M, Li C. Prevalence of mild cognitive impairment in community-dwelling Chinese populations aged over 55 years: a meta-analysis and systematic review. BMC Geriatr. 2021;21(1):10.
González HM, Tarraf W, Schneiderman N, Fornage M, Vásquez PM, Zeng D, Youngblood M, Gallo LC, Daviglus ML, Lipton RB, Kaplan R, Ramos AR, Lamar M, Thomas S, Chai A, DeCarli C. Prevalence and correlates of mild cognitive impairment among diverse Hispanics/Latinos: study of latinos-Investigation of neurocognitive aging results. Alzheimers Dement. 2019;15(12):1507–15.
Szcześniak D, Rymaszewska J, Zimny A, Sąsiadek M, Połtyn-Zaradna K, Smith EE, Zatońska K, Zatoński T, Rangarajan S, Yusuf S, Szuba A. Cerebral small vessel disease and other influential factors of cognitive impairment in the middle-aged: a long-term observational cohort PURE-MIND study in Poland. GeroScience. 2021;43(1):279–95.
Rosengart TK, Sweet J, Finnin EB, Wolfe P, Cashy J, Hahn E, Marymont J, Sanborn T. Neurocognitive functioning in patients undergoing coronary artery bypass graft surgery or percutaneous coronary intervention: evidence of impairment before intervention compared with normal controls. Ann Thorac Surg. 2005;80(4):1327–35.
Maekawa K, Goto T, Baba T, Yoshitake A, Katahira K, Yamamoto T. Impaired cognition preceding cardiac surgery is related to cerebral ischemic lesions. J Anesth. 2011;25(3):330–6.
Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59(5):1289–95.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Carrillo MC, Thies B, Phelps CH. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the national institute on aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT, ISPOCD group. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand. 2001;45(3):275–89.
Lewis MS, Maruff P, Silbert BS, Evered LA, Scott DA. The sensitivity and specificity of three common statistical rules for the classification of post-operative cognitive dysfunction following coronary artery bypass graft surgery. Acta Anaesthesiol Scand. 2006;50(1):50–7.
Heiserman JE, Drayer BP, Keller PJ, Fram EK. Intracranial vascular stenosis and occlusion: Evaluation with three-dimensional time-of-flight MR angiography. Radiology. 1992;185(3):667–73.
Atlas SW. MR angiography in neurologic disease. Radiology. 1994;193(1):1–16.
Masaryk TJ, Lewin JS, Laub G. Magnetic resonance angiography. In: Stark DD, Bradley WG, editors. Magnetic resonance imaging. 2nd ed. St Louis: Mosby Year Book; 1992. p. 299–313.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Needham MJ, Webb CE, Bryden DC, (2017) Postoperative cognitive dysfunction and dementia: what we need to know and do. Br J Anaesth 119 (suppl_1) i115-i125
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Rudolph JL, Schreiber KA, Culley DJ, McGlinchey RE, Crosby G, Levitsky S, Marcantonio ER. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54(6):663–77.
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, Rabbitt P,Jolles J, Larsen K, Hanning CD, Langeron O, Johnson T, Lauven PM, Kristensen PA, Biedler A, van Beem H, Fraidakis O, Silverstein JH, Beneken JE, Gravenstein JS. (1998) Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet. Mar 351 (9106) 857–61.
Johnson T, Monk T, Rasmussen LS, Abildstrom H, Houx P, Korttila K, Kuipers HM, Hanning CD, Siersma VD, Kristensen D, Canet J, Ibañaz MT, Moller JT. Postoperative cognitive dysfunction in middle-aged patients. Anesthesiology. 2002;96(6):1351–7.
Culley DJ, Flaherty D, Fahey MC, Rudolph JL, Javedan H, Huang CC, Wright J, Bader AM, Hyman BT, Blacker D, Crosby G. Poor performance on a preoperative cognitive screening test predicts postoperative complications in older orthopedic surgical patients. Anesthesiology. 2017;127(5):765–74.
Silbert B, Evered L, Scott DA, McMahon S, Choong P, Ames D, Maruff P, Jamrozik K. Preexisting cognitive impairment is associated with postoperative cognitive dysfunction after hip joint replacement surgery. Anesthesiology. 2015;122(6):1224–34.
Zietlow K, McDonald SR, Sloane R, Browndyke J, Lagoo-Deenadayalan S, Heflin MT. Preoperative cognitive impairment as a predictor of postoperative outcomes in a collaborative care model. J Am Geriatr Soc. 2018;66(3):584–9.
Evered LA, Silbert BS, Scott DA, Maruff P, Ames D. Prevalence of dementia 7.5 years after coronary artery bypass graft surgery. Anesthesiology. 2016;125(1):62–71.
Vidal JS, Sigurdsson S, Jonsdottir MK, Eiriksdottir G, Thorgeirsson G, Kjartansson O, Garcia ME, van Buchem MA, Harris TB, Gudnason V, Launer LJ. Coronary artery calcium, brain function and structure: the AGES-Reykjavik study. Stroke. 2010;41(5):891–7.
Sabayan B, van Buchem MA, Sigurdsson S, Zhang Q, Harris TB, Gudnason V, Arai AE, Launer LJ. Cardiac hemodynamics are linked with structural and functional features of brain aging: the age, gene/environment susceptibility (AGES)-Reykjavik study. J Am Heart Assoc. 2015;4(1): e001294.
Ito A, Goto T, Maekawa K, Baba T, Mishima Y, Ushijima K. Postoperative neurological complications and risk factors for pre-existing silent brain infarction in elderly patients undergoing coronary artery bypass grafting. J Anesth. 2012;26(3):405–11.
DeCarli C, Massaro J, Harvey D, Hald J, Tullberg M, Au R, Beiser A, D’Agostino R, Wolf PA. Measures of brain morphology and infarction in the framingham heart study: establishing what is normal. Neurobiol Aging. 2005;26(4):491–510.
Smith EE, O’Donnell M, Dagenais G, Lear SA, Wielgosz A, Sharma M, Poirier P, Stotts G, Black SE, Strother S, Noseworthy MD, Benavente O, Modi J, Goyal M, Batool S, Sanchez K, Hill V, McCreary CR, Frayne R, Islam S, DeJesus J, Rangarajan S, Teo K, Yusuf S. Early cerebral small vessel disease and brain volume cognition and gait. Ann Neurol. 2015;77(2):251–61.
Tini G, Scagliola R, Monacelli F, Malfa GL, Porto I, Brunelli C, Rosa GM. Alzheimer’s disease and cardiovascular disease: a particular association. Cardiol Res Pract. 2020;2020:2617970.
Kuźma E, Airdrie J, Littlejohns TJ, Lourida I, Thompson-Coon J, Lang IA, Scrobotovici M, Thacker EL, Fitzpatrick A, Kuller LH, Lopez OL, Longstreth WT Jr, Ukoumunne OC, Llewellyn DJ. Coronary artery bypass graft surgery and dementia risk in the cardiovascular health study. Alzheimer Dis Assoc Disord. 2017;31(2):120–7.
Dokkedal U, Hansen TG, Rasmussen LS, Mengel-From J, Christensen K. Cognitive functioning after surgery in middle-aged and elderly Danish twins. Anesthesiology. 2016;124(2):312–21.
Bratzke LC, Koscik RL, Schenning KJ, et al. Cognitive decline in the middle-aged after surgery and anaesthesia: results from the wisconsin registry for Alzheimer’s prevention cohort. Anaesthesia. 2018;73(5):549–55.
Acknowledgements
The authors would like to thank Dr. Tatsuo Yamamoto for the valuable comments and suggestions.
Author information
Authors and Affiliations
Contributions
TO and KM contributed to the study conception and design. TO, KM, and YM conducted the study, data collection, and analysis. The first draft of the manuscript was written by TO and it was revised by KM and NH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Oyoshi, T., Maekawa, K., Mitsuta, Y. et al. Predictors of early postoperative cognitive dysfunction in middle-aged patients undergoing cardiac surgery: retrospective observational study. J Anesth 37, 357–363 (2023). https://doi.org/10.1007/s00540-023-03164-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03164-w