Abstract
Purpose
This study aimed to elucidate the effects of neuraxial analgesia on labor in women classified based on the Robson classification system.
Methods
We retrospectively reviewed the clinical data of singleton cephalic nulliparous deliveries in labor at term between January 2018 and December 2021 and compared obstetrical outcomes between deliveries with and without neuraxial analgesia in women of Robson group 1 (spontaneous labor) and group 2a (induced labor). Statistical analyses were performed using the Wilcoxon ranked-sum test, Fisher’s exact test, and logistic regression model. Statistical significance was set at p < 0.05.
Results
We identified 2726 deliveries during the period, of which 387 deliveries (215 with analgesia and 172 without analgesia) were in Robson group 1 and 502 deliveries (258 with analgesia and 244 without analgesia) in Robson 2a. In Robson group 1 pregnancies, the cesarean section (CS) rate was higher in those who received analgesia (15%) than in those who did not (3%) (p = 0.0001). Multivariate analysis revealed that labor with analgesia was a significant risk factor for CS (p < 0.0001). Similarly, in Robson group 2a pregnancies, we observed a higher CS rate in those with analgesia than in those without analgesia (18 vs. 11%, p = 0.042).
Conclusion
A higher CS rate was observed in deliveries with analgesia than in those without analgesia both in the Robson group 1 and group 2a pregnancies.


Similar content being viewed by others

References
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin no. 209: obstetric analgesia and anesthesia. Obstet Gynecol. 2019;133:e208–25.
Anim-Somuah M, Smyth RMD, Cyna AM, Cuthbert A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev. 2018;5:CD00031.
Kurakazu M, Umehara N, Nagata C, Yamashita Y, Sato M, Sago H. Delivery mode and maternal and neonatal outcomes of combined spinal–epidural analgesia compared with no analgesia in spontaneous labor: a single-center observational study in Japan. J Obstet Gynaecol Res. 2020;46:425–33.
Naito Y, Ida M, Yamamoto R, Tachibana K, Kinouchi K. The effect of labor epidural analgesia on labor, delivery, and neonatal outcomes: a propensity score-matched analysis in a single Japanese institute. JA Clin Rep. 2019;5:40.
World Health Organization. WHO statement on caesarean section rates. World Health Organization; 2015. https://www.who.int/publications/i/item/WHO-RHR-15.02. Accessed 8 Apr 2022.
World Health Organization. Robson classification implementation manual. World Health Organization; 2017. Available from https://www.who.int/publications/i/item/9789241513197. Accessed 8 April 2022.
Brennan DJ, Robson MS, Murphy M, O’Herlihy C. Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. Am J Obstet Gynecol. 2009;201:308.e1-308.e8.
Betrán AP, Vindevoghel N, Souza JP, Gülmezoglu AM, Torloni MR. A systematic review of the Robson classification for caesarean section: what works, doesn’t work and how to improve it. PLoS ONE. 2014;9: e97769.
Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N. United States state-level variation in the use of neuraxial analgesia during labor for pregnant women. JAMA Netw Open. 2018;1: e186567.
Blondel B, Coulm B, Bonnet C, Goffinet F, Le Ray C, National Coordination Group of the National Perinatal Surveys. Trends in perinatal health in metropolitan France from 1995 to 2016: results from the French national perinatal surveys. J Gynecol Obstet Hum Reprod. 2017;46:701–13.
Public Health Agency of Canada. Care during labour and birth. In: Family centred maturnity and newborn care: national guidelines. Ottawa (ON): PHAC; 2018.
Lavand’homme P, Roelants F. Patient-controlled intravenous analgesia as an alternative to epidural analgesia during labor: questioning the use of the short-acting opioid remifentanil. Survey in the French part of Belgium (Wallonia and Brussels). Acta Anaesthesiol Belg. 2009;60:75–82.
Japan Association of Obstetricians and Gynecologists. Surveillance on delivery (in Japanese). Tokyo: Japan Association of Obstetricians and Gynecologists; 2017.
Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM. Using a simplified Bishop score to predict vaginal delivery. Obstet Gynecol. 2011;117:805–11.
Japan Society of Obstetrics and Gynecology (JSOG), Japan Association of Obstetricians and Gynecologists (JAOG). Guidelines for obstetrical practice in Japan. 2017 ed. Tokyo: Kyorin-Sha; 2017.
Japan Society of Obstetrics and Gynecology (JSOG), Japan Association of Obstetricians and Gynecologists (JAOG). Guidelines for obstetrical practice in Japan. 2020 ed. Tokyo: Kyorin-Sha; 2020.
Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804.
Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand Suppl. 1965;16:55–69.
American College of Obstetricians and Gynecologists (College), Society for Maternal-Fetal Medicine, Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210:179–93.
Hasegawa J, Farina A, Turchi G, Hasegawa Y, Zanello M, Baroncini S. Effects of epidural analgesia on labor length, instrumental delivery, and neonatal short-term outcome. J Anesth. 2013;27:43–7.
Nguyen U-SDT, Rothman KJ, Demissie S, Jackson DJ, Lang JM, Ecker JL. Epidural analgesia and risks of Cesarean and operative vaginal deliveries in nulliparous and multiparous women. Matern Child Health J. 2010;14:705–12.
Eriksen LM, Nohr EA, Kjaergaard H. Mode of delivery after epidural analgesia in a cohort of low-risk nulliparas. Birth. 2011;38:317–26.
Hung TH, Hsieh TT, Liu HP. Differential effects of epidural analgesia on modes of delivery and perinatal outcomes between nulliparous and multiparous women: a retrospective cohort study. PLoS ONE. 2015;10:1–11.
Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS ONE. 2016;11: e0148343.
Ishikawa K, Ikeda T, Miyazaki R. Cesarean delivery and perinatal mortality rates in Japan, 2007–2011. J Matern Fetal Neonatal Med. 2014;27:994–9.
Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing Cesarean delivery rate. Obstet Gynecol. 2011;118:29–38.
Song BL, Leong WL, Zeng Y, Siddiqui FJ, Assam PN, Lim Y, Chan ESY, Sia AT. Early versus late initiation of epidural analgesia for labour. Cochrane Database Syst Rev. 2014;17:CD0007238.
Fischer C, Blanié P, Jaouën E, Vayssière C, Kaloul I, Coltat JC. Ropivacaine, 0.1%, plus sufentanil, 0.5 microg/ml, versus bupivacaine, 0.1%, plus sufentanil, 0.5 microg/ml, using patient-controlled epidural analgesia for labor: a double-blind comparison. Anesthesiology. 2000;92:1588–93.
Lee BB, Ngan Kee WD, Ng FF, Lau TK, Wong ELY. Epidural infusions of ropivacaine and bupivacaine for labor analgesia: a randomized, double-blind study of obstetric outcome. Anesth Analg. 2004;98:1145–52.
Capogna G, Camorcia M, Stirparo S, Farcomeni A. Programmed intermittent epidural bolus versus continuous epidural infusion for labor analgesia: the effects on maternal motor function and labor outcome. A randomized double-blind study in nulliparous women. Anesth Analg. 2011;113:826–31.
Song Y, Du W, Zhou S, Zhou Y, Yu Y, Xu Z, Liu Z. Effect of dural puncture epidural technique combined with programmed intermittent epidural bolus on labor analgesia onset and maintenance: a randomized controlled trial. Anesth Analg. 2021;132:971–8.
Caughey AB, Sharshiner R, Cheng YW. Fetal malposition: impact and management. Clin Obstet Gynecol. 2015;58:241–5.
Lieberman E, Davidson K, Lee-Parritz A, Shearer E. Changes in fetal position during labor and their association with epidural analgesia. Obstet Gynecol. 2005;105:974–82.
Chestnut DH, Wong CA, Tsen LC, Kee WDN, Beilin Y, Mhyre JM, Bateman BT, Nathan N. Epidural and spinal analgesia: anaesthesia for labour and vaginal delivery. In: Wong CA, editor. Chestnut’s obstet anesth. 6th ed. Philadelphia: Mosby/Elsevier; 2019. p. 475–524.
Rahm VANR, Hallgren AH, Högberg HH, Hurtig IH, Odlind VO. Plasma oxytocin levels in women during labor with or without epidural analgesia: a prospective study. Acta Obstet Gynecol Scand. 2002;81:1033–9.
Behrens O, Goeschen K, Luck HJ, Fuchs AR. Effects of lumbar epidural analgesia on prostaglandin F2α release and oxytocin secretion during labor. Prostaglandins. 1993;45:285–96.
Kotaska AJ, Klein MC, Liston RM. Epidural analgesia associated with low-dose oxytocin augmentation increases cesarean births: a critical look at the external validity of randomized trials. Am J Obstet Gynecol. 2006;194:809–14.
American College of Obstetricians and Gynecologists. ACOG practice bulletin no 107: induction of labor. Obstet Gynecol. 2009;114:386–97.
National Institute for Health and Care Excellence (NICE). Surveillance report Induction of labour; 2017. London: National Institute for Health and Care Excellence. UK; 2008 NICE Guideline cg70. p. 2017.
Leduc D, Biringer A, Lee L, Dy J, Clinical practice obstetrics committee, special contributors. Induction of labour. J Obstet Gynaecol Can. 2013;35:840–57.
Zhao B, Qian X, Wang Q, Ou X, Lin B, Song X. The effects of ropivacaine 0.0625% and levobupivacaine 0.0625% on uterine and abdominal muscle electromyographic activity during the second stage of labor. Minerva Anestesiol. 2019;85:854–61.
Reitman E, Conell-Price J, Evansmith J, Olson L, Drosinos S, Jasper N, Randolph P, Smiley RM, Shafer S, Flood P. β2-adrenergic receptor genotype and other variables that contribute to labor pain and progress. Anesthesiology. 2011;114:927–39.
Terkawi AS, Jackson WM, Thiet MP, Hansoti S, Tabassum R, Flood P. Oxytocin and catechol-O-methyltransferase receptor genotype predict the length of the first stage of labor. Am J Obstet Gynecol. 2012;207:184.e1-184.e8.
Greenberg MB, Cheng YW, Hopkins LM, Stotland NE, Bryant AS, Caughey AB. Are there ethnic differences in the length of labor? Am J Obstet Gynecol. 2006;195:743–8.
Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, Hill K, Thom EA, El-Sayed YY, Perez-Delboy A, Rouse DJ, Saade GR, Boggess KA, Chauhan SP, Iams JD, Chien EK, Casey BM, Gibbs RS, Srinivas SK, Swamy GK, Simhan HN, Macones GA, Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513–23.
Wuitchik M, Bakal D, Lipshitz J. The clinical significance of pain and cognitive activity in latent labor. Obstet Gynecol. 1989;73:35–42.
Acknowledgements
We would like to thank Yoko Kawanishi, Kosuke Hiramatsu, Mahiru Kawano, Aiko Kakigano, and Toshihiro Kimura for their assistance and clinical support at Osaka University Hospital.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
The study was approved by the ethics committee of Osaka University Hospital, Japan (registration number: 21517).
Informed consent
Informed consent was obtained from all patients using an opt-out approach on the hospital website.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
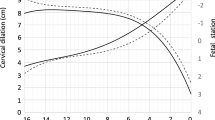
540_2022_3125_MOESM1_ESM.tif
Figure S1: Schematic diagram of the Robson classification. The shaded area indicates groups 1 and 2a. CS, cesarean section. Supplementary file1 (TIF 127 kb)
About this article
Cite this article
Yagi, T., Kinose, Y., Bun, M. et al. Obstetrical outcomes of labor with and without analgesia in Robson classification groups 1 and 2a: a single-center retrospective study. J Anesth 37, 39–48 (2023). https://doi.org/10.1007/s00540-022-03125-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-022-03125-9