Abstract
Background
Cardiac surgery in frail patients has been reported to be associated with increased mortality and morbidity but may improve functional status of frail patients. Few studies have investigated the impact of cardiac surgery on the trajectory of postoperative frailty. We hypothesized that cardiac surgery in frail patients would improve frailty postoperatively.
Method
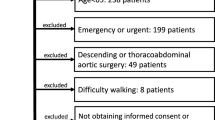
This study included 71 patients over 65 years old who were scheduled for cardiac surgery via sternotomy or thoracotomy. Frailty was prospectively evaluated using the Kihon Checklist (KCL) at 1 and 3 months postoperatively. Patients were divided into three groups based on the preoperative KCL score: nonfrail, prefrail, and frail. The interaction between the degree of preoperative frailty and the trajectory of postoperative KCL scores was assessed.
Results
The KCL score changed significantly over time (P < 0.001), and the KCL score trajectory differed significantly according to the degree of preoperative frailty (P for interaction = 0.003). In the frail group, the KCL score was significantly lower 3 months postoperatively than preoperatively (median 8, interquartile range [5, 9] versus median 9, interquartile range (9, 13), P = 0.029).
Conclusion
The trajectory of postoperative KCL scores differed significantly depending on the degree of preoperative frailty. At 3 months after cardiac surgery, the KCL score of frail patients was significantly improved, while that in nonfrail patients was significantly deteriorated.


Similar content being viewed by others
Data availability
The deidentified participant data will be shared on a request basis. Please directly contact the corresponding author to request data sharing.
References
Sepehri A, Beggs T, Hassan A, Rigatto C, Shaw-Daigle C, Tangri N, Arora RC. The impact of frailty on outcomes after cardiac surgery: a systematic review. J Thorac Cardiovasc Surg. 2014;148:3110–7.
Kim DH, Afilalo J, Shi SM, Popma JJ, Khabbaz KR, Laham RJ, Grodstein F, Guibone K, Lux E, Lipsitz LA. Evaluation of changes in functional status in the year after aortic valve replacement. JAMA Intern Med. 2019;179:383–91.
Afilalo J, Lauck S, Kim DH, Lefèvre T, Piazza N, Lachapelle K, Martucci G, Lamy A, Labinaz M, Peterson MD, Arora RC, Noiseux N, Rassi A, Palacios IF, Généreux P, Lindman BR, Asgar AW, Kim CA, Trnkus A, Morais JA, Langlois Y, Rudski LG, Morin JF, Popma JJ, Webb JG, Perrault LP. Frailty in older adults undergoing aortic valve replacement: The FRAILTY-AVR study. J Am Coll Cardiol. 2017;70:689–700.
Kotajarvi BR, Schafer MJ, Atkinson EJ, Traynor MM, Bruce CJ, Greason KL, Suri RM, Miller JD, LeBrasseur NK. The impact of frailty on patient-centered outcomes following aortic valve replacement. J Gerontol A Biol Sci Med Sci. 2017;72:917–21.
Arnold SV, Reynolds MR, Wang K, Magnuson EA, Baron SJ, Chinnakondepalli KM, Reardon MJ, Tadros PN, Zorn GL, Maini B, Mumtaz MA, Brown JM, Kipperman RM, Adams DH, Popma JJ, Cohen DJ. Health status after transcatheter or surgical aortic valve replacement in patients with severe aortic stenosis at increased surgical risk: results from the corevalve US pivotal trial. JACC Cardiovasc Interv. 2015;8:1207–17.
Miguelena-Hycka J, Lopez-Menendez J, Prada PC, Rodriguez-Roda J, Martin M, Vigil-Escalera C, Hernandez-Vaquero D, Miguelena JM, Silva J, Gonzalez-Colaço M. Influence of preoperative frailty on health-related quality of life after cardiac surgery. Ann Thorac Surg. 2019;108:23–9.
Fukutomi E, Okumiya K, Wada T, Sakamoto R, Ishimoto Y, Kimura Y, Chen WL, Imai H, Kasahara Y, Fujisawa M, Otsuka K, Matsubayashi K. Relationships between each category of 25-item frailty risk assessment (Kihon Checklist) and newly certified older adults under long-term care insurance: A 24-month follow-up study in a rural community in Japan. Geriatr Gerontol Int. 2015;15:864–71.
Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015;15:518–9.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56.
Satake S, Senda K, Hong YJ, Miura H, Endo H, Sakurai T, Kondo I, Toba K. Validity of the Kihon Checklist for assessing frailty status. Geriatr Gerontol Int. 2016;16:709–15.
JCS Joint Working Group. Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012). Circ J. 2014;78:2022–93.
Izumi C, Eishi K, Ashihara K, Arita T, Otsuji Y, Kunihara T, Komiya T, Shibata T, Seo Y, Daimon M, Takanashi S, Tanaka H, Nakatani S, Ninami H, Nishi H, Hayashida K, Yaku H, Yamaguchi J, Yamamoto K, Watanabe H, Abe Y, Amaki M, Amano M, Obase K, Tabata M, Miura T, Miyake M, Murata M, Watanabe N, Akasaka T, Okita Y, Kimura T, Sawa Y, Yoshida K. JCS/JSCS/JATS/JSVS 2020 Guidelines on the management of valvular heart disease. Circ J. 2020;84:2037–119.
Horne D, Kehler DS, Kaoukis G, Hiebert B, Garcia E, Chapman S, Duhamel TA, Arora RC. Impact of physical activity on depression after cardiac surgery. Can J Cardiol. 2013;29:1649–56.
Pandey A, Kitzman D, Reeves G. Frailty is intertwined with heart failure: mechanisms, prevalence, prognosis, assessment, and management. JACC Heart Fail. 2019;7:1001–11.
Sündermann SH, Dademasch A, Seifert B, Rodriguez Cetina Biefer H, Emmert MY, Walther T, Jacobs S, Mohr FW, Falk V, Starck CT. Frailty is a predictor of short- and mid-term mortality after elective cardiac surgery independently of age. Interact Cardiovasc Thorac Surg. 2014;18:580–5.
Becher RD, Murphy TE, Gahbauer EA, Leo-Summers L, Stabenau HF, Gill TM. Factors associated with functional recovery among older survivors of major surgery. Ann Surg. 2020;272:92–8.
Tully PJ. Psychological depression and cardiac surgery: a comprehensive review. J Extra Corpor Technol. 2012;44:224–32.
Iga J, Uchiyama M, Ohmori T, Ogasawara K, Ozaki N, Kanba S, Saito T, Sugiyama N, Suzuki M, Tomita M, Nakamura T, Nomura S, Furihata R, Watanabe K. Treatment guidelines of the japanese society of mood disorders II. Depression (DSM-5) / Major Depressive Disorder. https://www.secretariat.ne.jp/jsmd/iinkai/katsudou/data/20190724.pdf (2016). Accessed 27, June 2021.
Morone NE, Weiner DK, Belnap BH, Karp JF, Mazumdar S, Houck PR, He F, Rollman BL. The impact of pain and depression on recovery after coronary artery bypass grafting. Psychosom Med. 2010;72:620–5.
Arrowsmith JE, Grocott HP, Reves JG, Newman MF. Central nervous system complications of cardiac surgery. Br J Anaesth. 2000;84:378–93.
Terrando N, Eriksson LI, Ryu JK, Yang T, Monaco C, Feldmann M, Jonsson Fagerlund M, Charo IF, Akassoglou K, Maze M. Resolving postoperative neuroinflammation and cognitive decline. Ann Neurol. 2011;70:986–95.
Hall RI, Smith MS, Rocker G. The systemic inflammatory response to cardiopulmonary bypass: pathophysiological, therapeutic, and pharmacological considerations. Anesth Analg. 1997;85:766–82.
van Dijk D, Keizer AM, Diephuis JC, Durand C, Vos LJ, Hijman R. Neurocognitive dysfunction after coronary artery bypass surgery: a systematic review. J Thorac Cardiovasc Surg. 2000;120:632–9.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
IRB information: This study protocol was approved by the Ethics Committee of the National Cerebral and Cardiovascular Center (registration number: M29-100).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Shimakura, K., Minami, K., Yoshitani, K. et al. Cardiac surgery improves the postoperative frailty score of frail patients. J Anesth 36, 186–193 (2022). https://doi.org/10.1007/s00540-021-03025-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-03025-4