Abstract
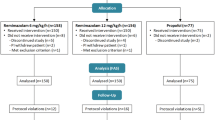
A new ultra-short-acting benzodiazepine intravenous anesthetic agent, remimazolam, was launched in Japan in 2020. Anesthesia during awake craniotomy is reportedly being performed safely using remimazolam; however, studies on its efficacy in awake craniotomy have not been conducted. We aimed to compare the efficacy of remimazolam and propofol in awake craniotomy. In this retrospective study, patients who underwent awake craniotomy (n = 36) at our hospital between December 2019 and January 2021 were divided into two groups: the propofol group (P group: n = 21) and the remimazolam group (R group: n = 15). There was no significant difference in the recovery time between the two groups (p = 0.18). The number of patients experiencing nausea was higher in the R group than in the P group (p = 0.02); however, regression analysis revealed that the use of remimazolam contributed to increased intraoperative nausea (odds ratio = 14.4, p = 0.04). No significant differences were observed in the frequency of vomiting and other intraoperative complications between the two groups. In conclusion, remimazolam has the potential for use as an alternative drug in anesthetic management during awake craniotomy.
Similar content being viewed by others
Change history
24 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00540-023-03232-1
References
Lobo FA, Wagemakers M, Absalom AR. Anaesthesia for awake craniotomy. Br J Anaesth. 2016;116:740–4. https://doi.org/10.1093/bja/aew113.
Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anaesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34:543–53. https://doi.org/10.1007/s00540-020-02788-6.
Sato T, Kato Y, Yamamoto M, Nishiwaki K. Novel anesthetic agent remimazolam as an alternative for the asleep-awake-asleep technique of awake craniotomy. JA Clin Rep. 2020;6:92. https://doi.org/10.1186/s40981-020-00398-5.
Sato T, Okumura T, Nishiwaki K. Preanesthesia scalp blocks reduce intraoperative pain and hypertension in the asleep-awake-asleep method of awake craniotomy: a retrospective study. J Clin Anesth. 2020;66: 109946. https://doi.org/10.1016/j.jclinane.2020.109946.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
Goettel N, Bharadwaj S, Venkatraghavan L, Mehta J, Bernstein M, Mannien PH. Dexmedetomidine vs propofol-remifentanil conscious sedation for awake craniotomy: a prospective randomized controlled trial. Br J Anaesth. 2016;116:811–21. https://doi.org/10.1093/bja/aew024.
Sneyd JR, Gambus PL, Rigby-Jones AE. Current status of perioperative hypnotics, role of benzodiazepines, and the case for remimazolam: a narrative review. Br J Anaesth. 2021;127:41–55. https://doi.org/10.1016/j.bja.2021.03.028.
Yamamoto T, Kurabe M, Kamiya Y. Re-sleeping after reversal of remimazolam by flumazenil. J Anesth. 2021;35:322. https://doi.org/10.1007/s00540-021-02915-x.
Kamata K, Morioka N, Maruyama T, Komayama N, Nitta M, Muragaki Y, Kawamata T, Ozaki M. The effect of single low-dose dexamethasone on vomiting during awake craniotomy. J Anesth. 2016;30(6):941–8. https://doi.org/10.1007/s00540-016-2243-9.
Piccioni F, Fanzio M. Management of anesthesia in awake craniotomy. Minerva Anestesiol. 2008;74(7–8):393–408.
Vasileiou I, Xanthos T, Koudouna E, Perrea D, Klonaris C, Katsargyris A, Papadimitriou L. Propofol: a review of its non-anaesthetic effects. Eur J Pharmacol. 2009;605:1–8. https://doi.org/10.1016/j.ejphar.2009.01.007.
Acknowledgements
The authors would like to thank Editage (https://www.editage.jp) for the English language review.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sato, T., Nishiwaki, K. Comparison of remimazolam and propofol in anesthetic management for awake craniotomy: a retrospective study. J Anesth 36, 152–155 (2022). https://doi.org/10.1007/s00540-021-03021-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-03021-8