Abstract
Purpose
Recently, a new handheld ultrasound-based device, called Accuro, has been commercialized with a real-time automated interpretation of lumbar ultrasound images. We hypothesized that the handheld ultrasound device would improve the efficacy and safety of combined spinal-epidural anesthesia (CSEA) for cesarean delivery in obese parturients.
Methods
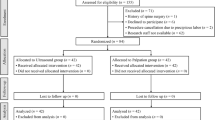
Eighty parturients with a body mass index > 30 kg∙m−2 scheduled for elective cesarean delivery were randomly allocated equally (palpation group and ultrasound group). The primary outcome was the first insertion success rate. Secondary outcomes were the time taken to identify the needle puncture site, duration of CSEA procedure, the total time, the rate of parturients who require needle redirections, the number of skin punctures, changes in the intended interspace, and the incidence of complications.
Results
Compared to the palpation group, the first insertion success rate was significantly higher (72.5% vs. 40.0%; P = 0.003), and time taken to identify the needle puncture site was less (30 [26–36] vs. 39 [32–49] seconds; P = 0.001) in the ultrasound group. The rate of parturients who required needle redirections (40.0% vs. 72.5%; P = 0.003) and the incidence of paresthesia were both lower (7.5% vs. 45.0%; P < 0.001). The other outcomes had no significant difference between groups. The mean difference between the epidural depth measured by the handheld ultrasound and needle depth was − 0.29 cm [95% limit of agreement, − 0.52 to − 0.05].
Conclusions
Our study suggests using the Accuro ultrasound device can enhance the efficacy and safety of CSEA in obese parturients when executed by experienced anesthesiologists, and its automated estimation of epidural depth is accurate.



Similar content being viewed by others
Change history
10 June 2021
Figure 3 was published incorrectly in PDF and corrected in this version.
References
Taylor CR, Dominguez JE, Habib AS. Obesity and obstetric anesthesia: current insights. Local Reg Anesth. 2019;12:111–24.
Wang Q, Yin C, Wang TL. Ultrasound facilitates identification of combined spinal-epidural puncture in obese parturients. Chin Med J. 2012;125(21):3840–3.
Schlotterbeck H, Schaeffer R, Dow WA, Touret Y, Bailey S, Diemunsch P. Ultrasonographic control of the puncture level for lumbar neuraxial block in obstetric anaesthesia. Br J Anaesth. 2008;100:230–4.
Whitty R, Moore M, Macarthur A. Identification of the lumbar interspinous spaces: palpation versus ultrasound. Anesth Analg. 2008;106:538–40.
Tanaka K, Irikoma S, Kokubo S. Identification of the lumbar interspinous spaces by palpation and verified by X-rays. Braz J Anesthesiol. 2013;63:245–8.
Lee A. Ultrasound in obstetric anesthesia. Semin Perinatol. 2014;38:349–58.
Li M, Ni X, Xu Z, Shen F, Song Y, Li Q, Liu Z. Ultrasound-assisted technology versus the conventional landmark location method in spinal anesthesia for cesarean delivery in obese parturients. Anesth Analg. 2019;129(1):155–61.
Park SK, Bae J, Yoo S, Kim WH, Lim YJ, Bahk JH, Kim JT. Ultrasound-assisted versus landmark-guided spinal anesthesia in patients with abnormal apinal anatomy: a randomized controlled trial. Anesth Analg. 2020;130(3):787–95.
Whitty RJ, Maxwell CV, Carvalho JC. Complications of neuraxial anesthesia in an extreme morbidly obese patient for cesarean section. Int J Obstet Anesth. 2007;16:139–44.
Shaikh F, Brzezinski J, Alexander S, Arzola C, Carvalho JCA, Beyene J, Sung L. Ultrasound imaging for lumbar punctures and epidural catheterisations: systematic review and meta-analysis. BMJ. 2013;346:f1720.
Perlas A, Chaparro LE, Chin KJ. Lumbar neuraxial ultrasound for spinal and epidural anesthesia: a systematic review and meta-analysis. Reg Anesth Pain Med. 2016;41:251–60.
Margarido CB, Arzola C, Balki M, Carvalho JCA. Anesthesiologists’ learning curves for ultrasound assessment of the lumbar spine. Can J Anaesth. 2009;57(2):120–6.
Singla P, Dixon AJ, Sheeran JL, Scalzo D, Mauldin FW Jr, Tiouririne M. Feasibility of spinal snesthesia placement using automated interpretation of lumbar ultrasound images: a prospective randomized controlled trial. J Anesth Clin Res. 2019;10(2):878.
Tiouririne M, Dixon AJ, Mauldin FW Jr, Scalzo D, Krishnaraj A. Imaging performance of a handheld ultrasound system with real-time computer-aided detection of lumbar spine anatomy: a feasibility study. Invest Radiol. 2017;52(8):447–55.
Seligman KM, Weiniger CF, Carvalho B. The Accuracy of a handheld ultrasound device for neuraxial depth and landmark assessment: a prospective cohort trial. Anesth Analg. 2018;126(6):1995–8.
Carvalho B, Seligman KM, Weiniger CF. The comparative accuracy of a handheld and console ultrasound device for neuraxial depth and landmark assessment. Int J Obstet Anesth. 2019;39:68–73.
Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011;115:94–101.
Tubinis MD, Lester SA, Schlitz CN, Morgan CJ, Sakawi Y, Powell MF. Utility of ultrasonography in identification of midline and epidural placement in severely obese parturients. Minerva Anestesiol. 2019;85(10):1089–96.
Sahin T, Balaban O, Sahin L, Solak M, Toker K. A randomized controlled trial of preinsertion ultrasound guidance for spinal anaesthesia in pregnancy: outcomes among obese and lean parturients. J Anesth. 2013;28(3):413–9.
Dancel R, Schnobrich D, Puri N, Franco-Sadud R, Cho J, Grikis L, Lucas BP, El-Barbary M, Soni NJ. Recommendations on the use of ultrasound guidance for adult lumbar puncture—a position statement of the society of hospital medicine. J Hosp Med. 2019;14(10):591–601.
Gambling DR. Lumbar ultrasound: useful gadget or time-consuming gimmick? Int J Obstet Anesth. 2011;20:318–20.
Margarido CB, Mikhael R, Arzola C, Balki M, Carvalho JC. The intercristal line determined by palpation is not a reliable anatomical landmark for neuraxial anesthesia. Can J Anaesth. 2011;58:262–6.
Tawfik MM, Atallah MM, Elkharboutly WS, Allakkany NS, Abdelkhalek M. Does preprocedural ultrasound increase the first-pass success rate of epidural catheterization before cesarean delivery? A randomized controlled trial. Anesth Analg. 2017;124(3):851–6.
Ghisi D, Tomasi M, Giannone S, Luppi A, Aurini L, Toccaceli L, Benazzo A, Bonarelli S. A randomized comparison between Accuro and palpation-guided spinal anesthesia for obese patients undergoing orthopedic surgery. Reg Anesth Pain Med. 2019;25:100538.
Acknowledgements
The authors thank the patients who participated in the study and all authors who contributed to the study.
Funding
This work was supported in part by the National Natural Science Foundation of China (81771188), Shanghai Municipal Commission of Health and Family Planning (201740072), Science and Technology Commission of Shanghai Municipality and Rivanna Medical provided the handheld ultrasound device for the study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by ML and SZ. The first draft of the manuscript was written by XN, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ni, X., Li, Mz., Zhou, Sq. et al. Accuro ultrasound-based system with computer-aided image interpretation compared to traditional palpation technique for neuraxial anesthesia placement in obese parturients undergoing cesarean delivery: a randomized controlled trial. J Anesth 35, 475–482 (2021). https://doi.org/10.1007/s00540-021-02922-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02922-y