Abstract
Purpose
To evaluate changes in cerebral regional oxygen saturation (rSO2) after spinal anesthesia and compare the changes in rSO2 and systemic oxygenation between dexmedetomidine sedation and propofol sedation.
Methods
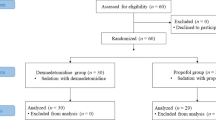
Thirty-six patients scheduled to undergo transurethral surgery under spinal anesthesia were randomly assigned to the dexmedetomidine (n = 18) and propofol groups (n = 18). We used near-infrared spectroscopy sensors to measure rSO2, and obtained data from each side were averaged. After oxygen insufflation, baseline measurements of mean arterial blood pressure (MAP), heart rate, rSO2, pulse oximetry saturation (SpO2), bispectral index, and body temperature were made. After spinal anesthesia, we measured these parameters every 5 min. Twenty minutes after spinal injection, dexmedetomidine or propofol administration was started. We measured each parameter at 10, 25, and 40 min after the administration of dexmedetomidine or propofol.
Results
The baseline rSO2 in the dexmedetomidine group was 71.3 ± 7.3%, and that in the propofol group was 71.8 ± 5.6%. After spinal anesthesia, rSO2 in both groups decreased significantly (dexmedetomidine group: 65.4 ± 6.9%; propofol group: 64.3 ± 7.4%). After administering sedatives, rSO2 was equivalent after spinal anesthesia. rSO2 was comparable between the two groups. MAP and SpO2 were significantly higher in the dexmedetomidine group than in the propofol group.
Conclusion
Spinal anesthesia decreased rSO2; however, the decline was not severe. Dexmedetomidine and propofol did not compromise cerebral oxygenation under spinal anesthesia. Nevertheless, MAP and SpO2 were more stable in dexmedetomidine sedation than in propofol sedation. Dexmedetomidine may be suitable for spinal anesthesia.




Similar content being viewed by others
References
Minville V, Asehnoune K, Salau S, Bourdet B, Tissot B, Lubrano V, Fourcade O. The effects of spinal anesthesia on cerebral blood flow in the very elderly. Anesth Analg. 2009;108:1291–4.
Ishiyama T, Kashimoto S, Oguchi T, Yamaguchi T, Okuyama K, Kumazawa T. Epidural ropivacaine anesthesia decreases the bispectral index during the awake phase and sevoflurane general anesthesia. Anesth Analg. 2005;100:728–32.
Kurup V, Ramani R, Atanassoff PG. Sedation after spinal anesthesia in elderly patients: a preliminary observational study with the PSA-4000. Can J Anaesth. 2004;51:562–5.
Ishiyama T, Dohi S, Iida H, Watanabe Y, Shimonaka H. Mechanisms of dexmedetomidine-induced cerebrovascular effects in canine in vivo experiments. Anesth Analg. 1995;81:1208–15.
Shibuya K, Ishiyama T, Ichikawa M, Sato H, Okuyama K, Sessler DI, Matsukawa T. The direct effects of propofol on pial microvessels in rabbits. J Neurosurg Anesthesiol. 2009;21:40–6.
Pater PM, Drummond JC. Cerebral physiology and the effects of anesthetic drugs. In: Miller RD, editor. Miller’s anesthesia. 7th ed. Philadelphia: Churchill Livingstone; 2010. p. 305–39.
Venn RM, Grounds RM. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth. 2001;87:684–90.
Heil LBB, Santos CL, Santos RS, Samary CS, Cavalcanti VCM, Araújo MMPM, Poggio H, Maia Lde A, Trevenzoli IH, Pelosi P, Fernandes FC, Villela NR, Silva PL, Rocco PRM. The effects of short-term propofol and dexmedetomidine on lung mechanics, histology, and biological markers in experimental obesity. Anesth Analg. 2016;122:1015–23.
Orihashi K, Sueda T, Okada K, Imai K. Near-infrared spectroscopy for monitoring cerebral ischemia during selective cerebral perfusion. Eur J Cardiothorac Surg. 2004;26:907–11.
Rhondali O, Andre C, Pouyau A, Mahr A, Juhel S, De Queiroz M, Rhzioual-Berrada K, Mathews S, Chassard D. Sevoflurane anesthesia and brain perfusion. Paediatr Anaesth. 2015;25:180–5.
Rigamonti A, Scandroglio M, Minicucci F, Magrin S, Carozzo A, Casati A. A clinical evaluation of near-infrared cerebral oximetry in the awake patient to monitor cerebral perfusion during carotid endarterectomy. J Clin Anesth. 2005;17:426–30.
Fassiadis N, Zayed H, Rashid H, Green DW. Invos Cerebral Oximeter compared with the transcranial Doppler for monitoring adequacy of cerebral perfusion in patients undergoing carotid endarterectomy. Int Angiol. 2006;25:401–6.
Nishikawa K, Hagiwara R, Nakamura K, Ishizeki J, Kubo K, Saito S, Goto F. The effects of the extent of spinal block on the BIS score and regional cerebral oxygen saturation in elderly patients: a prospective, randomized, and double-blinded study. J Clin Monit Comput. 2007;21:109–14.
Fassoulaki A, Paraskeva A, Tsaroucha A. Cesarean delivery under spinal anesthesia is associated with decreases in cerebral oxygen saturation as assessed by NIRS: an observational study. Curr Med Res Opin. 2014;30:331–7.
Hoppenstein D, Zohar E, Ramaty E, Shabat S, Fredman B. The effects of general vs spinal anesthesia on frontal cerebral oxygen saturation in geriatric patients undergoing emergency surgical fixation of the neck of femur. J Clin Anesth. 2005;17:431–8.
Lairez O, Ferré F, Portet N, Marty P, Delmas C, Cognet T, Kurrek M, Carrié D, Fourcade O, Minville V. Cardiovascular effects of low-dose spinal anaesthesia as a function of age: an observational study using echocardiography. Anaesth Crit Care Pain Med. 2015;34:271–6.
Kurz A, Sessler DI, Narzt E, Lenhardt R, Lackner F. Morphometric influences on intraoperative core temperature changes. Anesth Analg. 1995;80:562–7.
Ebert TJ, Morgan BJ, Barney JA, Denahan T, Smith JJ. Effects of aging on baroreflex regulation of sympathetic activity in humans. Am J Physiol. 1992;263:H798–803.
Prielipp RC, Wall MH, Tobin JR, Groban L, Cannon MA, Fahey FH, Gage HD, Stump DA, James RL, Bennett J, Butterworth J. Dexmedetomidine-induced sedation in volunteers decreases regional and global cerebral blood flow. Anesth Analg. 2002;95:1052–9.
Zornow MH, Fleischer JE, Scheller MS, Nakakimura K, Drummond JC. Dexmedetomidine, an alpha 2-adrenergic agonist, decreases cerebral blood flow in the isoflurane-anesthetized dog. Anesth Analg. 1990;70:624–30.
Ludbrook GL, Upton RN, Grant C, Gray EC. Cerebral effects of propofol following bolus administration in sheep. Anaesth Intensive Care. 1996;24:26–31.
Drummond JC, Dao AV, Roth DM, Cheng CR, Atwater BI, Minokadeh A, Pasco LC, Patel PM. Effect of dexmedetomidine on cerebral blood flow velocity, cerebral metabolic rate, and carbon dioxide response in normal humans. Anesthesiology. 2008;108:225–32.
Laaksonen L, Kallioinen M, Langsjo J, Laitio T, Scheinin A, Scheinin J, Kaisti K, Maksimow A, Kallionpaa RE, Rajala V, Johansson J, Kantonen O, Nyman M, Siren S, Valli K, Revonsuo A, Solin O, Vahlberg T, Alkire M, Scheinin H. Comparative effects of dexmedetomidine, propofol, sevoflurane, and S-ketamine on regional cerebral glucose metabolism in humans: a positron emission tomography study. Br J Anaesth. 2018;121:281–90.
Matsuoka T, Ishiyama T, Shintani N, Kotoda M, Mitsui K, Matsukawa T. Changes of cerebral regional oxygen saturation during pneumoperitoneum and Trendelenburg position under propofol anesthesia: a prospective observational study. BMC Anesthesiol. 2019;19:72.
Mayer B, Pohl M, Hummler HD, Schmid MB. Cerebral oxygenation and desaturations in preterm infants - a longitudinal data analysis. J Neonatal Perinatal Med. 2017;10:267–73.
Hunter CL, Oei JL, Lui K, Schindler T. Cerebral oxygenation as measured by near-infrared spectroscopy in neonatal intensive care: correlation with arterial oxygenation. Acta Paediatr. 2017;106:1073–8.
Chang YF, Chao A, Shih PY, Hsu YC, Lee CT, Tien YW, Yeh YC, Chen LW, Research NCoMM. Comparison of dexmedetomidine versus propofol on hemodynamics in surgical critically ill patients. J Surg Res. 2018;228:194–200.
Wu Y, Zhang Y, Hu X, Qian C, Zhou Y, Xie J. A comparison of propofol vs. dexmedetomidine for sedation, haemodynamic control and satisfaction, during esophagogastroduodenoscopy under conscious sedation. J Clin Pharm Ther. 2015;40:419–25.
Colin PJ, Hannivoort LN, Eleveld DJ, Reyntjens KMEM, Absalom AR, Vereecke HEM, Struys MMRF. Dexmedetomidine pharmacodynamics in healthy volunteers: 2. Haemodynamic profile. Br J Anaesth. 2017;119:211–20.
Wong ESW, Man RYK, Vanhoutte PM, Ng KFJ. Dexmedetomidine induces both relaxations and contractions, via different α2-adrenoceptor subtypes, in the isolated mesenteric artery and aorta of the rat. J Pharmacol Exp Ther. 2010;335:659–64.
Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93:382–94.
Yokoe C, Hanamoto H, Boku A, Sugimura M, Morimoto Y, Kudo C, Niwa H. The effect of nitrous oxide inhalation on the hypotensive response to propofol: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:166–73.
Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS. A comparison of dexmedetomidine versus propofol during drug-induced sleep endoscopy in sleep apnea patients. Laryngoscope. 2016;126:763–7.
Eastwood PR, Platt PR, Shepherd K, Maddison K, Hillman DR. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology. 2005;103:470–7.
Schramm P, Tzanova I, Hagen F, Berres M, Closhen D, Pestel G, Engelhard K. Cerebral oxygen saturation and cardiac output during anaesthesia in sitting position for neurosurgical procedures: a prospective observational study. Br J Anaesth. 2016;117:482–8.
Yamakage M, Kamada Y, Toriyabe M, Honma Y, Namiki A. Changes in respiratory pattern and arterial blood gases during sedation with propofol or midazolam in spinal anesthesia. J Clin Anesth. 1999;11:375–9.
Kashiwagi M, Osaka Y, Onimaru H, Takeda J. Optical imaging of propofol-induced central respiratory depression in medulla-spinal cord preparations from newborn rats. Clin Exp Pharmacol Physiol. 2011;38:186–91.
Ishiyama T, Kotoda M, Asano N, Ikemoto K, Shintani N, Matsuoka T, Matsukawa T. Effects of hyperventilation on cerebral oxygen saturation estimated using near-infrared spectroscopy: a randomised comparison between propofol and sevoflurane anaesthesia. Eur J Anaesthesiol. 2016;33:929–35.
Keyl C, Trenk D, Laule S, Schuppe C, Staier K, Wiesenack C, Albiez G. Predicted and measured plasma propofol concentration and bispectral index during deep sedation in patients with impaired left ventricular function. J Cardiothorac Vasc Anesth. 2009;23:182–7.
Zhong T, Guo QL, Pang YD, Peng LF, Li CL. Comparative evaluation of the cerebral state index and the bispectral index during target-controlled infusion of propofol. Br J Anaesth. 2005;95:798–802.
Xi C, Sun S, Pan C, Ji F, Cui X, Li T. Different effects of propofol and dexmedetomidine sedation on electroencephalogram patterns: wakefulness, moderate sedation, deep sedation and recovery. PLoS ONE. 2018;13:e0199120.
Chakrabarti D, Surve RM, Bs D, Masapu D. Intraoperative aberrant bispectral index values due to facial nerve monitoring. J Clin Anesth. 2017;37:61–2.
Acknowledgments
We would like to thank Editage (http://www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
All authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kumakura, Y., Ishiyama, T., Matsuoka, T. et al. Effects of spinal anesthesia and sedation with dexmedetomidine or propofol on cerebral regional oxygen saturation and systemic oxygenation a period after spinal injection. J Anesth 34, 806–813 (2020). https://doi.org/10.1007/s00540-020-02816-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02816-5