Abstract
Purpose
We evaluated the efficacy of hemostatic therapy based on point-of-care (POC) testing in patients undergoing cardiac surgery.
Methods
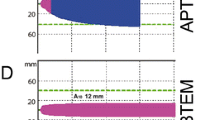
This was a single-institution, prospective, randomized, double-blinded study. In step 1, 90 patients scheduled for elective cardiac surgery underwent complete blood count and fibrinogen measurements at baseline, after cardiopulmonary bypass (CPB) initiation (CPB start), just after CPB end, and in the intensive care unit (ICU). In step 2, 72 patients scheduled for elective cardiac surgery underwent conventional laboratory coagulation tests (control group) or POC coagulation tests (POC group). Transfusions were prepared using the fibrinogen and platelet values at mainly “CPB start” for the control group, and using the ROTEM values at mainly “CPB end” for the POC group. Consequently, the step 2 patients were divided into high- and low-risk subgroups based on the EuroSCORE II by logistic regression analysis; transfusion data and bleeding volumes were compared between the control and POC groups within the high- and low-risk subgroups.
Results
In step 1, all blood components were significantly decreased at CPB start compared with baseline, and platelet and fibrinogen levels remained almost constant from CPB start to end. In step 2, the transfusion rates and perioperative bleeding volumes did not significantly differ between the control and POC groups. Subgroup analysis suggested that only the high-risk subgroup significantly differed regarding perioperative red blood cell transfusion and total bleeding volume in the ICU.
Conclusions
POC testing is beneficial for cardiac surgery patients with a EuroSCORE II of ≥1.83%.


Similar content being viewed by others
References
Ichikawa J, Kodaka M, Kitahara T, Sato N, Nishiyama K, Nakano K, Komori M. The use of thromboelastometry and tranexamic acid reduces blood loss and transfusion requirements in cardiac surgery under cardiopulmonary bypass (in Japanese). Masui. 2015;64:131–8.
Görlinger K, Dirkmann D, Hanke AA, Kamler M, Kottenberg E, Thielmann M, Jakob H, Peters J. First-line therapy with coagulation factor concentrates combined with point-of-care coagulation testing is associated with decreased allogeneic blood transfusion in cardiovascular surgery: a retrospective, single-center cohort study. Anesthesiology. 2011;115:1179–91.
Ichikawa J, Marubuchi T, Nishiyama K, Kodaka M, Görlinger K, Ozaki M, Komori M. Introduction of thromboelastometry-guided administration of fresh-frozen plasma is associated with decreased allogeneic blood transfusions and post-operative blood loss in cardiopulmonary-bypass surgery. Blood Transfus. 2017;23:1–9.
Kawashima S, Suzuki Y, Sato T, Kikura M, Katoh T, Sato S. Four-group classification based on fibrinogen level and fibrin polymerization associated with postoperative bleeding in cardiac surgery. Clin Appl Thromb Hemost. 2016;22:648–55.
Aoki K, Sugimoto A, Nagasawa A, Saito M, Ohzeki H. Optimization of thromboelastography-guided platelet transfusion in cardiovascular surgery. Gen Thorac Cardiovasc Surg. 2012;60:411–6.
Shore-Lesserson L, Manspeizer HE, DePerio M, Francis S, Vela-Cantos F, Ergin MA. Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth Analg. 1999;88:312–9.
Nuttall GA, Oliver WC, Santrach PJ, Bryant S, Dearani JA, Schaff HV, Ereth MH. Efficacy of a simple intraoperative transfusion algorithm for nonerythrocyte component utilization after cardiopulmonary bypass. Anesthesiology. 2001;94:773–81.
Wang J, Ma HP, Zheng H. Blood loss after cardiopulmonary bypass, standard vs titrated protamine: a meta-analysis. Neth J Med. 2013;71:123–7.
Radulovic V, Laffin A, Hansson KM, Backlund E, Baghaei F, Jeppsson A. Heparin and protamine titration does not improve haemostasis after cardiac surgery: a prospective randomized study. PLoS ONE. 2015;10:e0130271.
Nakayama Y, Nakajima Y, Tanaka KA, Sessler DI, Maeda S, Iida J, Ogawa S, Mizobe T. Thromboelastometry-guided intraoperative haemostatic management reduces bleeding and red cell transfusion after paediatric cardiac surgery. Br J Anaesth. 2015;114:91–102.
Weber CF, Görlinger K, Meininger D, Herrmann E, Bingold T, Moritz A, Cohn LH, Zacharowski K. Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012;117:531–47.
Eagle KA, Guyton RA, Davidoff R, Ewy GA, Fonger J, Gardner TJ, Gott JP, Herrmann HC, Marlow RA, Nugent W, O’Connor GT, Orszulak TA, Rieselbach RE, Winters WL, Yusuf S, Gibbons RJ, Alpert JS, Garson A Jr, Gregoratos G, Russell RO, Ryan TJ, Smith SC Jr. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation. 1999;100:1464–80.
https://autoassign.mujinwari.biz/. Accessed 28 Dec 2016
Japanese Red Cross Society: [Blood Programme]. Available at: https://www.jrc.or.jp/mr/blood_product/about/red_blood_cell/. Accessed 28 June 2018 (in Japanese)
Solomon C, Pichlmaier U, Schoechl H, Hagl C, Raymondos K, Scheinichen D, Koppert W, Rahe-Meyer N. Recovery of fibrinogen after administration of fibrinogen concentrate to patients with severe bleeding after cardiopulmonary bypass surgery. Br J Anaesth. 2010;104:555–62.
Sato T, Kawashima S, Suzuki Y, Kikura M, Takatoku K, Heima D, Nishio H, Aoki T, Nishizawa J, Katoh T, Sato S. [Thromboelastometry (ROTEMTM), fibrinogen concentration and platelet counts during cardiopulmonary bypass predict perioperative requirements for blood transfusion in cardiac surgery] (in Japanese with English abstract). Cardiovas Anesth. 2015;19:49–544.
G*Power: statistical power analyses for Windows and Mac. Available at: https://gpower.hhu.de/. Accessed 28 June 2018
Owings JT, Pollock ME, Gosselin RC, Ireland K, Jahr JS, Larkin EC. Anticoagulation of children undergoing cardiopulmonary bypass is overestimated by current monitoring techniques. Arch Surg. 2000;135:1042–7.
Girdauskas E, Kempfert J, Kuntze T, Borger MA, Enders J, Fassl J, Falk V, Mohr FW. Thromboelastometrically guided transfusion protocol during aortic surgery with circulatory arrest: a prospective, randomized trial. J Thorac Cardiovasc Surg. 2010;140:1117–24.
Lodewyks C, Heinrichs J, Grocott HP, Karkouti K, Romund G, Arora RC, Tangri N, Rabbani R, Abou-Setta A, Zarychanski R. Point-of-care viscoelastic hemostatic testing in cardiac surgery patients: a systematic review and meta-analysis. Can J Anaesth. 2018;65:1333–477.
Serraino GF, Murphy GJ. Routine use of viscoelastic blood tests for diagnosis and treatment of coagulopathic bleeding in cardiac surgery: updated systematic review and meta-analysis. Br J Anaesth. 2017;118:823–33.
Wikkelsø A, Wetterslev J, Møller AM, Afshari A. Thromboelastography (TEG) or rotational thromboelastometry (ROTEM) to monitor haemostatic treatment in bleeding patients: a systematic review with meta-analysis and trial sequential analysis. Anaesthesia. 2017;72:519–31.
Meco M, Montisci A, Giustiniano E, Greco M, Pappalardo F, Mammana L, Panisi P, Roscitano C, Cirri S, Donatelli F, Albano G. Point-of-care viscoelastic hemostatic testing in cardiac surgery patients: a systematic review and meta-analysis. Can J Anaesth. 2018;65:1333–477.
Murkin JM, Falter F, Granton J, Young B, Burt C, Chu M. High-dose tranexamic acid is associated with nonischemic clinical seizures in cardiac surgical patients. Anesth Analg. 2010;110:350–3.
Karkouti K, Callum J, Wijeysundera DN, Rao V, Crowther M, Grocott HP, Pinto R, Scales DC, TACS Investigators. Point-of-care hemostatic testing in cardiac surgery: a stepped-wedge clustered randomized controlled trial. Circulation. 2016;134:1152–62.
Acknowledgements
The research was supported by JSPS KAKEN#26462374. We thank Kelly Zammit, BVSc, from Liwen Bianji, Edanz Editing China (https://www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
MK participated in patient recruitment, data collection, and writing the first draft of the paper. JI participated in study design and data analysis. KA participated in patient recruitment and data collection. MK provided final approval of the version to be published.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kodaka, M., Ichikawa, J., Ando, K. et al. Thromboelastometry and a hemostasis management system are most beneficial for guiding hemostatic therapy in cardiac surgery patients with a EuroSCORE II of ≥1.83%: a randomized controlled two-step trial. J Anesth 34, 666–674 (2020). https://doi.org/10.1007/s00540-020-02810-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02810-x