Abstract
Purpose
Retinopathy of prematurity (ROP) is an ocular disorder that primarily occurs in premature infants and is the most common cause of vision impairment. This study examined the effect of desflurane on angiogenesis in a mouse model of oxygen-induced retinopathy (OIR).
Methods
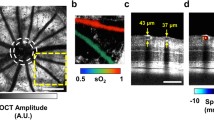
Mice were randomly allocated to the control (C), ROP control (Rc), or ROP with desflurane exposure (Rd) group. To induce ROP, 7-day-old mice were exposed to 75% oxygen in a chamber for 5 days [postnatal days (P) 7–12], and thereafter returned to room air. Age-matched mice exposed to room air formed the C group. The Rd group was exposed to 8% desflurane for 2 h on P12, P13, and P14 with 40% oxygen. To observe changes in angiogenesis of the retina, mice were sacrificed at P16.
Results
The ratio of avascular area/total retinal area was not changed significantly in the Rd group, compared to the Rc group. The expression of endothelial growth factor A (VEGF-A) and hypoxia inducible factor-1α (HIF-1α) in the Rd group and Rc group was not significantly different.
Conclusions
Desflurane does not have a significant influence on retinal angiogenesis via HIF-1α and VEGF-A expression in the OIR mouse model. However, these findings are not directly applicable to premature infants, and it is thus necessary to perform further studies to determine the effect of desflurane on angiogenesis.



Similar content being viewed by others
References
Campbell K. Intensive oxygen therapy as a possible cause of retrolental fibroplasia; a clinical approach. Med J Aust. 1951;2:48–50.
Hwang JH, Lee EH, Kim EA. Retinopathy of prematurity among very-low-birth-weight infants in Korea: incidence, treatment, and risk factors. J Korean Med Sci. 2015;30:S88–94.
Heidary G, Vanderveen D, Smith LE. Retinopathy of prematurity: current concepts in molecular pathogenesis. Semin Ophthalmol. 2009;24:77–81.
Sapieha P, Joyal JS, Rivera JC, Kermorvant-Duchemin E, Sennlaub F, Hardy P, Lachapelle P, Chemtob S. Retinopathy of prematurity: understanding ischemic retinal vasculopathies at an extreme of life. J Clin Invest. 2010;120:3022–32.
Zin A, Gole GA. Retinopathy of prematurity-incidence today. Clin Perinatol. 2013;40:185–200.
Vartanian RJ, Besirli CG, Barks JD, Andrews CA, Musch DC. Trends in the screening and treatment of retinopathy of prematurity. Pediatrics. 2017;139:e20161978.
Kim HY, Baek SH, Baik SW, Bae SS, Ha JM, Kim M, Byeon GJ, Kim HJ, Ri HS, Kim SH. The effect of sevoflurane on retinal angiogenesis in a mouse model of oxygen-induced retinopathy. J Anesth. 2018;32:204–10.
Zhao J, Hao J, Fei X, Wang X, Hou Y, Deng C. Isoflurane inhibits occludin expression via up-regulation of hypoxia-inducible factor 1 alpha. Brain Res. 2014;1562:1–10.
Sun Y, Li QF, Zhang Y, Hu R, Jiang H. Isoflurane preconditioning increases survival of rat skin random-pattern flaps by induction of HIF-1alpha expression. Cell Physiol Biochem. 2013;31:579–91.
Li QF, Wang XR, Yang YW, Su DS. Up-regulation of hypoxia inducible factor 1alpha by isoflurane in Hep3B cells. Anesthesiology. 2006;105:1211–9.
Hermann A, Mack HG, Oberhammer H. Conformations and structures of desflurane and isoflurane. J Fluorine Chem. 2000;101:223–31.
Smith LE, Wesolowski E, McLellan A, Kostyk SK, D'Amato R, Sullivan R, D'Amore PA. Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci. 1994;35:101–11.
Radhakrishnan N, Pillai GS, Kiran KR, Lekshmypriya A. Retinopathy of prematurity—an overview. Kerala J Ophthalmol. 2017;29:154–9.
Scott A, Fruttiger M. Oxygen-induced retinopathy: a model for vascular pathology in the retina. Eye. 2010;24:416–21.
Zhao H, Iwasaki M, Yang J, Savage S, Ma D. Hypoxia-inducible factor-1: a possible link between inhalational anesthetics and tumor progression? Acta Anaesthesiol Taiwan. 2014;52:70–6.
Wiesmann C, Fuh G, Christinger HW, Eigenbrot C, Wells JA, Vos AM. Crystal structure at 1.7 A resolution of VEGF in complex with domain 2 of the Flt-1 receptor. Cell. 1997;91:695–704.
Rundhaug JE. Matrix metalloproteinases and angiogenesis. J Cell Mol Med. 2005;9:267–85.
Bussolino F, Mantovani A, Persico G. Molecular mechanisms of blood vessel formation. Trends Biochem Sci. 1997;22:251–6.
Afuwape AO, Kiriakidis S, Paleolog EM. The role of the angiogenic molecule VEGF in the pathogenesis of rheumatoid arthritis. Histol Histopathol. 2002;17:961–72.
Sale SM, Read JA, Stoddart PA, Wolf AR. Prospective comparison of sevoflurane and desflurane in formerly premature infants undergoing inguinal herniotomy. Br J Anaesth. 2006;96:774–8.
Giles EK, Lawrence AJ, Duncan JR. Exploring the modulation of hypoxia-inducible factor (HIF)-1alpha by volatile anesthetics as a possible mechanism underlying volatile anesthetic-induced CNS injury. Neurochem Res. 2014;39:1640–7.
Datta K, Li J, Bhattacharya R, Gasparian L, Wang E, Mukhopadhyay D. Protein kinase C zeta transactivates hypoxia-inducible factor alpha by promoting its association with p300 in renal cancer. Cancer Res. 2004;64:456–62.
Mellidis K, Ordodi V, Galatou E, Sandesc D, Bubenek S, Duicu O, Muntean D, Lazou A. Activation of prosurvival signaling pathways during the memory phase of volatile anesthetic preconditioning in human myocardium: a pilot study. Mol Cell Biochem. 2014;388:195–201.
Toma O, Weber NC, Wolter JI, Obal D, Preckel B, Schlack W. Desflurane preconditioning induces time-dependent activation of protein kinase C epsilon and extracellular signal-regulated kinase 1 and 2 in the rat heart in vivo. Anesthesiology. 2004;101:1372–80.
Iwasaki M, Zhao H, Jaffer T, Unwith S, Benzonana L, Lian Q, Sakamoto A, Ma D. Volatile anaesthetics enhance the metastasis related cellular signalling including CXCR2 of ovarian cancer cells. Oncotarget. 2016;7:26042–56.
Müller-Edenborn B, Roth-Z'graggen B, Bartnicka K, Borgeat A, Hoos A, Borsig L, Beck-Schimmer B. Volatile anesthetics reduce invasion of colorectal cancer cells through down-regulation of matrix metalloproteinase-9. Anesthesiology. 2012;117:293–301.
Kodama M, Satoh Y, Otsubo Y, Araki Y, Yonamine R, Masui K, Kazama T. Neonatal desflurane exposure induces more robust neuroapoptosis than do isoflurane and sevoflurane and impairs working memory. Anesthesiology. 2011;115:979–91.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ri, HS., Bae, S.S., Ha, J.M. et al. The effect of desflurane on retinal angiogenesis in a mouse model of oxygen-induced retinopathy. J Anesth 34, 352–357 (2020). https://doi.org/10.1007/s00540-020-02752-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02752-4