Abstract
Purpose
Hydrogen gas (H2) inhalation improved the survival rate of hemorrhagic shock. However, its mechanisms are unknown. We hypothesized that H2 protected the endothelial glycocalyx during hemorrhagic shock and prolonged survival time.
Methods
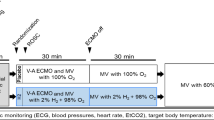
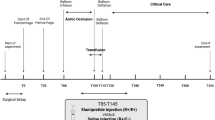
83 Sprague–Dawley rats were anesthetized with isoflurane. The animals were randomly assigned to 5 groups: room air with no shock, 1.2% H2 with no shock, room air with shock (Control-S), 1.2% H2 with shock (H21.2%-S), and 3.0% H2 with shock (H23.0%-S). Shock groups were bled to a mean arterial pressure of 30–35 mmHg and held for 60 min, then resuscitated with normal saline at fourfold the amount of the shed blood volume.
Results
The syndecan-1 level was significantly lower in the H21.2%-S [8.3 ± 6.6 ng/ml; P = 0.01; 95% confidence interval (CI), 3.2–35.8] than in the Control-S (27.9 ± 17.0 ng/ml). The endothelial glycocalyx was significantly thicker in the H21.2%-S (0.15 ± 0.02 µm; P = 0.007; 95% CI, 0.02–0.2) than in the Control-S (0.06 ± 0.02 µm). The survival time was longer in the H21.2%-S (327 ± 67 min, P = 0.0160) than in the Control-S (246 ± 69 min). The hemoglobin level was significantly lower in the H21.2%-S (9.4 ± 0.5 g/dl; P = 0.0034; 95% CI, 0.6–2.9) than in the Control-S (11.1 ± 0.8 g/dl). However, the H23.0%-S was not significant.
Conclusions
Inhalation of 1.2% H2 gas protected the endothelial glycocalyx and prolonged survival time during hemorrhagic shock. Therapeutic efficacy might vary depending on the concentration.




Similar content being viewed by others
References
Kawashima Y, Irita K, Morita K, Tuzaki K, Sawa T. Preoperative hemorrhagic shock and intraoperative bleeding: two main causes of surgical deaths in Japan. J Jpn Soc Blood Trans. 2005;51(1):23–31.
Kozar RA, Peng Z, Zhang R, Holcomb JB, Pati S, Park P, Ko TC, Paredes A. Plasma restoration of endothelial glycocalyx in a rodent model of hemorrhagic shock. Anesth Analg. 2011;112(6):1289–95.
Chappell D, Westphal M, Jacob M. The impact of the glycocalyx on microcirculatory oxygen distribution in critical illness. Curr Opin Anaesthesiol. 2009;22(2):155–62.
Okada H, Takemura G, Suzuki K, Oda K, Takada C, Hotta Y, Miyazaki N, Tsujimoto A, Muraki I, Ando Y, Zaikokuji R, Matsumoto A, Kitagaki H, Tamaoki Y, Usui T, Doi T, Yoshida T, Yoshida S, Ushikoshi H, Toyoda I, Ogura S. Three-dimensional ultrastructure of capillary endothelial glycocalyx under normal and experimental endotoxemic conditions. Crit Care. 2017;21(1):261.
Rubio-Gayosso I, Platts SH, Duling BR. Reactive oxygen species mediate modification of glycocalyx during ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol. 2006;290(6):H2247–H2256256.
Iba T, Levy JH. Derangement of the endothelial glycocalyx in sepsis. J Thromb Haemost. 2019;17(2):283–94.
Diebel ME, Martin JV, Liberati DM, Diebel LN. The temporal response and mechanism of action of tranexamic acid in endothelial glycocalyx degradation. J Trauma Acute Care Surg. 2018;84(1):75–80.
Kazuma S, Tokinaga Y, Kimizuka M, Azumaguchi R, Hamada K, Yamakage M. Sevoflurane promotes regeneration of the endothelial glycocalyx by upregulating sialyltransferase. J Surg Res. 2019;241:40–7.
Ohsawa I, Ishikawa M, Takahashi K, Watanabe M, Nishimaki K, Yamagata K, Katsura K, Katayama Y, Asoh S, Ohta S. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med. 2007;13(6):688–94.
Ichihara M, Sobue S, Ito M, Ito M, Hirayama M, Ohno K. Beneficial biological effects and the underlying mechanisms of molecular hydrogen—comprehensive review of 321 original articles. Med Gas Res. 2015;5:12.
Xie K, Liu L, Yu Y, Wang G. Hydrogen gas presents a promising therapeutic strategy for sepsis. Biomed Res Int. 2014;2014:807635.
Yu Y, Yang Y, Bian Y, Li Y, Liu L, Zhang H, Xie K, Wang G, Yu Y. Hydrogen gas protects against intestinal injury in wild type but not NRF2 knockout mice with severe sepsis by regulating HO-1 and HMGB1 release. Shock. 2017;48(3):364–70.
Yonamine R, Satoh Y, Kodama M, Araki Y, Kazama T. Coadministration of hydrogen gas as part of the carrier gas mixture suppresses neuronal apoptosis and subsequent behavioral deficits caused by neonatal exposure to sevoflurane in mice. Anesthesiology. 2013;118(1):105–13.
Shinbo T, Kokubo K, Sato Y, Hagiri S, Hataishi R, Hirose M, Kobayashi H. Breathing nitric oxide plus hydrogen gas reduces ischemia-reperfusion injury and nitrotyrosine production in murine heart. Am J Physiol Heart Circ Physiol. 2013;305(4):H542–H550550.
Hayashida K, Sano M, Kamimura N, Yokota T, Suzuki M, Ohta S, Fukuda K, Hori S. Hydrogen inhalation during normoxic resuscitation improves neurological outcome in a rat model of cardiac arrest independently of targeted temperature management. Circulation. 2014;130(24):2173–80.
Hayashida K, Sano M, Ohsawa I, Shinmura K, Tamaki K, Kimura K, Endo J, Katayama T, Kawamura A, Kohsaka S, Makino S, Ohta S, Ogawa S, Fukuda K. Inhalation of hydrogen gas reduces infarct size in the rat model of myocardial ischemia-reperfusion injury. Biochem Biophys Res Commun. 2008;373(1):30–5.
Matsuoka T, Suzuki M, Sano M, Hayashida K, Tamura T, Homma K, Fukuda K, Sasaki J. Hydrogen gas inhalation inhibits progression to the “irreversible” stage of shock after severe hemorrhage in rats. J Trauma Acute Care Surg. 2017;83(3):469–75.
Kataoka H, Ushiyama A, Akimoto Y, Matsubara S, Kawakami H, Iijima T. Structural behavior of the endothelial glycocalyx is associated with pathophysiologic status in septic mice: an integrated approach to analyzing the behavior and function of the glycocalyx using both electron and fluorescence intravital microscopy. Anesth Analg. 2017;125(3):874–83.
Kobayashi K, Mimuro S, Sato T, Kobayashi A, Kawashima S, Makino H, Doi M, Katoh T, Nakajima Y. Dexmedetomidine preserves the endothelial glycocalyx and improves survival in a rat heatstroke model. J Anesth. 2018;32(6):880–5.
van den Berg BM, Vink H, Spaan JA. The endothelial glycocalyx protects against myocardial edema. Circ Res. 2003;92(6):592–4.
Rehm M, Bruegger D, Christ F, Conzen P, Thiel M, Jacob M, Chappell D, Stoeckelhuber M, Welsch U, Reichart B, Peter K, Becker BF. Shedding of the endothelial glycocalyx in patients undergoing major vascular surgery with global and regional ischemia. Circulation. 2007;116(17):1896–906.
Becker BF, Chappell D, Bruegger D, Annecke T, Jacob M. Therapeutic strategies targeting the endothelial glycocalyx: acute deficits, but great potential. Cardiovasc Res. 2010;87(2):300–10.
Tamura T, Hayashida K, Sano M, Onuki S, Suzuki M. Efficacy of inhaled HYDROGEN on neurological outcome following BRAIN ischemia during post-cardiac arrest care (HYBRID II trial): study protocol for a randomized controlled trial. Trials. 2017;18(1):488.
Kohama K, Yamashita H, Aoyama-Ishikawa M, Takahashi T, Billiar TR, Nishimura T, Kotani J, Nakao A. Hydrogen inhalation protects against acute lung injury induced by hemorrhagic shock and resuscitation. Surgery. 2015;158(2):399–407.
Du Z, Liu J, Jia H, Xu W, Zhao X. Three hydrogen-rich solutions protect against intestinal injury in uncontrolled hemorrhagic shock. Int J Clin Exp Med. 2015;8(5):7620–6.
Du Z, Jia H, Liu J, Zhao X, Xu W. Effects of three hydrogen-rich liquids on hemorrhagic shock in rats. J Surg Res. 2015;193(1):377–82.
Aguirre JA, Lucchinetti E, Clanachan AS, Plane F, Zaugg M. Unraveling interactions between anesthetics and the endothelium: update and novel insights. Anesth Analg. 2016;122(2):330–48.
Iba T. Glycocalyx regulates the intravascular hemostasis. Juntendo Med J. 2016;62(4):330–5.
Osuka A, Kusuki H, Yoneda K, Matsuura H, Matsumoto H, Ogura H, Ueyama M. Glycocalyx shedding is enhanced by age and correlates with increased fluid requirement in patients with major burns. Shock. 2018;50(1):60–5.
Iuchi K, Imoto A, Kamimura N, Nishimaki K, Ichimiya H, Yokota T, Ohta S. Molecular hydrogen regulates gene expression by modifying the free radical chain reaction-dependent generation of oxidized phospholipid mediators. Sci Rep. 2016;6:18971.
Chappell D, Hofmann-Kiefer K, Jacob M, Rehm M, Briegel J, Welsch U, Conzen P, Becker BF. TNF-alpha induced shedding of the endothelial glycocalyx is prevented by hydrocortisone and antithrombin. Basic Res Cardiol. 2009;104(1):78–89.
van Bommel J, Siegemund M, Henny ChP, Ince C. Heart, kidney, and intestine have different tolerances for anemia. Transl Res. 2008;151(2):110–7.
Bihorac A, Delano MJ, Schold JD, Lopez MC, Nathens AB, Maier RV, Layon AJ, Baker HV, Moldawer LL. Incidence, clinical predictors, genomics, and outcome of acute kidney injury among trauma patients. Ann Surg. 2010;252(1):158–65.
Chelazzi C, Villa G, Mancinelli P, De Gaudio AR, Adembri C. Glycocalyx and sepsis-induced alterations in vascular permeability. Crit Care. 2015;19:26.
Kurita T, Morita K, Fukuda K, Uraoka M, Takata K, Sanjo Y, Sato S. Influence of hemorrhagic shock and subsequent fluid resuscitation on the electroencephalographic effect of isoflurane in a swine model. Anesthesiology. 2005;103(6):1189–94.
Nakajima Y, Moriwaki G, Ikeda K, Fujise Y. The effects of sevoflurane on recovery of brain energy metabolism after cerebral ischemia in the rat: a comparison with isoflurane and halothane. Anesth Analg. 1997;85(3):593–9.
Acknowledgements
The authors thank I. Ohta, Y. Kumakiri, and Y. Tokunaga (Hamamatsu University School of Medicine) for their technical assistance with the electron microscopy. We thank T. Ojima (Hamamatsu University School of Medicine) for his statistical assistance. We thank Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript. This work was supported by JSPS KAKENHI (Grant Numbers JP19K09371 and JP18K08885).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TS, SM, and KK. The first draft of the manuscript was written by TS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sato, T., Mimuro, S., Katoh, T. et al. 1.2% Hydrogen gas inhalation protects the endothelial glycocalyx during hemorrhagic shock: a prospective laboratory study in rats. J Anesth 34, 268–275 (2020). https://doi.org/10.1007/s00540-020-02737-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02737-3