Abstract
Purpose
Rocuronium Bromide Intravenous Solution® (Maruishi Pharmaceutical Co., Ltd, Osaka, Japan) is a newly developed generic drug and we have noticed that compared with conventional rocuronium formulations [e.g. Esmeron (Eslax), MSD Co. Ltd., Tokyo, Japan], rocuronium Maruishi appeared to cause less pain or withdrawal movement. The aim of this study was to assess the hypothesis that the injection of rocuronium Maruishi causes less body movement than rocuronium MSD does, during rapid-sequence induction of anesthesia.
Methods
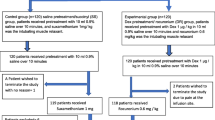
Sixty patients were allocated randomly to one of two groups. In one group, rocuronium MSD was used and in the other group, rocuronium Maruishi was used. After induction of general anesthesia, a test drug (containing rocuronium) 0.9 mg/kg was injected. Patient’s withdrawal movement was graded with the scale. Primary outcome measure was the incidence of moderate or severe movement after the injection of rocuronium. Secondary outcome measure was the degree of movement between the groups.
Results
Moderate or severe withdrawal movement was observed after the injection of rocuronium MSD in 11 of 30 patients (37%) and after the injection of rocuronium Maruishi in 3 of 30 patients (10%). There was a significant difference in the incidence between the groups (P = 0.013, 95% CI for difference 26–28%). The degree of movement was also significantly greater for rocuronium MSD than for rocuronium Maruishi (P = 0.015).
Conclusion
Compared with rocuronium MSD, rocuronium Maruishi is more suitable than conventional rocuronium formulations, for rapid-sequence induction of anesthesia.
Similar content being viewed by others
References
Stept WJ, Safar P. Rapid induction-intubation for prevention of gastric-content aspiration. Anesth Analg. 1970;49:633–6.
Sajayan A, Wicker J, Ungureanu N, Mendonca C, Kimani PK. Current practice of rapid sequence induction of anaesthesia in the UK—a national survey. Br J Anaesth. 2016;117(Suppl 1):i69–i74.
Mazurek AJ, Rae B, Hann S, Kim I, Castro B, Cote CJ. Rocuronium versus succinylcholine: are they equally effective during rapid-sequence induction of anesthesia? Anesth Analg. 1998;87:1259–62.
Chiarella AB, Jolly DT, Huston CM, Clanachan AS. Comparison of four strategies to reduce the pain associated with intravenous administration of rocuronium. Br J Anaesth. 2003;90:377–9.
Kwak HJ, Kim JY, Kim YB, Min SK, Moon BK, Kim JY. Pharmacological prevention of rocuronium-induced injection pain or withdrawal movements: a meta-analysis. J Anesth. 2013;27:742–9.
Shevchenko Y, Jocson JC, McRae VA, Stayer SA, Schwartz RE, Rehman M, Choudhry DK. The use of lidocaine for preventing the withdrawal associated with the injection of rocuronium in children and adolescents. Anesth Analg. 1999;88:746–8.
Ahmad N, Choy CY, Aris EA, Balan S. Preventing the withdrawal response associated with rocuronium injection: a comparison of fentanyl with lidocaine. Anesth Analg. 2005;100:987–90.
Morton HJ, Wylie WD. Anaesthetic deaths due to regurgitation or vomiting. Anaesthesia. 1951;6:190–205.
Sellick BA. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet. 1961;2:404–6.
Asai T. Airway management in patients undergoing emergency Cesarean section. J Anesth. 2015;29:927–33.
Memiş D, Turan A, Karamanlioğlu B, Süt N, Pamukçu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol, and fentanyl. Anesth Analg. 2002;94:1517–20.
Asai T, Eguchi T, Shingu K. Masseter spasm during induction of anaesthesia using propofol and fentanyl. Eur J Anaesthesiol. 1998;15:614.
Hogue CW Jr, Bowdle TA, O'Leary C, Duncalf D, Miguel R, Pitts M, Streisand J, Kirvassilis G, Jamerson B, McNeal S, Batenhorst R. A multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgery. Anesth Analg. 1996;83:279–85.
Ciftci T, Erbatur S, Ak M. Comparison of the effects of dexmedetomidine and remifentanil on potential extreme haemodynamic and respiratory response following mask ventilation and laryngoscopy in patients with mandibular fractures. Eur Rev Med Pharmacol Sci. 2015;19:4427–33.
Bennett JA, Abrams JT, Van Riper DF, Horrow JC. Difficult or impossible ventilation after sufentanil-induced anesthesia is caused primarily by vocal cord closure. Anesthesiology. 1997;87:1070–4.
Khan FA, Ullah H. Pharmacological agents for preventing morbidity associated with the haemodynamic response to tracheal intubation. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD004087.pub2.
Tuncali B, Karci A, Tuncali BE, Mavioglu O, Olguner CG, Ayhan S, Elar Z. Dilution of rocuronium to 0.5 mg/mL with 0.9% NaCl eliminates the pain during intravenous injection in awake patients. Anesth Analg. 2004;99:740–3.
Klement W, Arndt JO. Pain on i.v. injection of some anaesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br J Anaesth. 1991;66:189–95.
Ti LK, Dhara SS. Vecuronium, like rocuronium, causes pain on injection. Br J Anaesth. 1998;81:487.
Keisuke J, Yutaka I, Erika K, Masamichi K, Kuniharu M, Yoshiro Y. A new rocuronium formulation not causing vascular pain in a flexor reflex model od anesthetized rats. J Anesth. 2018;32:806–12.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Tachikawa, M., Asai, T. & Okuda, Y. Rocuronium Bromide Intravenous Solution Maruishi® is more suitable than ESLAX Intravenous® during rapid-sequence induction of anesthesia. J Anesth 33, 600–603 (2019). https://doi.org/10.1007/s00540-019-02673-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02673-x