Abstract
Purpose
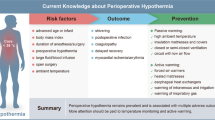
Inadvertent hypothermia is a relatively common intraoperative complication. Few studies have investigated predictors of body temperature change or the effect of the blanket type used with a forced-air warming device during the intraoperative period. We investigated the predictive factors of intraoperative body temperature change in scheduled abdominal surgery.
Methods
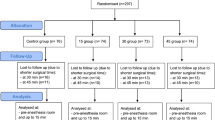
We retrospectively reviewed the data from 2574 consecutive adult patients who underwent scheduled abdominal surgery in the supine position. Temperature data were collected from anesthesia records. Multiple regression analysis was performed at 60, 120, and 180 min after the surgical incision to identify the factors influencing body temperature change. We conducted nonlinear regression analysis using the equation ΔT = α (e−γt—1) + βt, where ΔT represented the change in intraoperative core temperature (°C), t represented the surgical duration (minutes), and α, β, and γ were constants.
Results
The intraoperative core temperature change was explained by the equation ΔT = 0.59 (e− 0.018t − 1) + 0.0043t. Younger age, higher body mass index (BMI), male sex, laparoscopic surgery, and use of an underbody blanket were associated with increased core temperature at 1 or 2 h after surgical incision. Male sex and an underbody blanket remained strong predictive variables even 3 h after surgical incision, whereas BMI had little explanatory power at this timepoint. The difference in the heating effect of an underbody versus an overbody blanket was 0.0012 °C per minute.
Conclusions
The blanket type of the forced-air warmer, age, sex, laparoscopic surgery, and BMI are predictors of intraoperative core temperature change.

Similar content being viewed by others
References
Greif R, Laciny S, Rajek A, Doufas AG, Sessler DI. Blood pressure response to thermoregulatory vasoconstriction during isoflurane and desflurane anesthesia. Acta Anaesthesiol Scand. 2003;47:847–52.
Royse CF, Liew DF, Wright CE, Royse AG, Angus JA. Persistent depression of contractility and vasodilation with propofol but not with sevoflurane or desflurane in rabbits. Anesthesiology. 2008;108:87–93.
Chen A, Ashburn MA. Cardiac effects of opioid therapy. Pain Med. 2015;16(Suppl 1):27–31.
Sessler DI, McGuire J, Moayeri A, Hynson J. Isoflurane-induced vasodilation minimally increases cutaneous heat loss. Anesthesiology. 1991;74:226–32.
Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109:318–38.
Frank SM, Fleisher LA, Breslow MJ, Higgins MS, Olson KF, Kelly S, Beattie C. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA. 1997;277:1127–34.
Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108:71–7.
Schmied H, Kurz A, Sessler DI, Kozek S, Reiter A. Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty. Lancet. 1996;347:289–92.
Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–15.
Zhou J, Poloyac SM. The effect of therapeutic hypothermia on drug metabolism and response. Cellular mechanisms to organ function. Expert Opin Drug Metab Toxicol. 2011;7:803–16.
Sun Z, Honar H, Sessler DI, Dalton JE, Yang D, Panjasawatwong K, Deroee AF, Salmasi V, Saager L, Kurz A. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. Anesthesiology. 2015;122:276–85.
Han SB, Gwak MS, Choi SJ, Ko JS, Kim GS, Son HJ, Shin JC. Risk factors for inadvertent hypothermia during adult living-donor liver transplantation. Transpl Proc. 2014; 46: 705–8.
Kasai T, Hirose M, Yaegashi K, Matsukawa T, Takamata A, Tanaka Y. Preoperative risk factors of intraoperative hypothermia in major surgery under general anesthesia. Anesth Analg. 2002;95:1381–3. table of contents.
Yang L, Huang CY, Zhou ZB, Wen ZS, Zhang GR, Liu KX, Huang WQ. Risk factors for hypothermia in patients under general anesthesia: is there a drawback of laminar airflow operating rooms? A prospective cohort study. Int J Surg. 2015;21:14–7.
Sessler DI. Temperature regulation and monitoring. In: Miller RD, editor. Miller’s anesthesia. Eighth edition. Philadelphia: Elsevier Health Sciences; 2015. p. 1627.
Bräuer A, English MJ, Lorenz N, Steinmetz N, Perl T, Braun U, Weyland W. Comparison of forced-air warming systems with lower body blankets using a copper manikin of the human body. Acta Anaesthesiol Scand. 2003;47:58–64.
Hardy JD, Du Bois EF. Differences between men and women in their response to heat and cold. Proc Natl Acad Sci U S A. 1940;26:389–98.
Bal NC, Maurya SK, Sopariwala DH, Sahoo SK, Gupta SC, Shaikh SA, Pant M, Rowland LA, Bombardier E, Goonasekera SA, Tupling AR, Molkentin JD, Periasamy M. Sarcolipin is a newly identified regulator of muscle-based thermogenesis in mammals. Nat Med. 2012;18:1575–9.
Erdling A, Johansson A. Core temperature–the intraoperative difference between esophageal versus nasopharyngeal temperatures and the impact of prewarming, age, and weight: a randomized clinical trial. AANA J. 2015;83:99–105.
Kurz A, Plattner O, Sessler DI, Huemer G, Redl G, Lackner F. The threshold for thermoregulatory vasoconstriction during nitrous oxide/isoflurane anesthesia is lower in elderly than in young patients. Anesthesiology. 1993;79:465–9.
Nguyen NT, Fleming NW, Singh A, Lee SJ, Goldman CD, Wolfe BM. Evaluation of core temperature during laparoscopic and open gastric bypass. Obes Surg. 2001;11:570–5.
Stewart BT, Stitz RW, Tuch MM, Lumley JW. Hypothermia in open and laparoscopic colorectal surgery. Dis Colon Rectum. 1999;42:1292–5.
Song C, Tang B, Campbell PA, Cuschieri A. Thermal spread and heat absorbance differences between open and laparoscopic surgeries during energized dissections by electrosurgical instruments. Surg Endosc. 2009;23:2480–7.
Umenai T, Nakajima Y, Sessler DI, Taniguchi S, Yaku H, Mizobe T. Perioperative amino acid infusion improves recovery and shortens the duration of hospitalization after off-pump coronary artery bypass grafting. Anesth Analg. 2006;103:1386–93.
Inoue S, Shinjo T, Kawaguchi M, Nakajima Y, Furuya H. Amino acid infusions started after development of intraoperative core hypothermia do not affect rewarming but reduce the incidence of postoperative shivering during major abdominal surgery: a randomized trial. J Anesth. 2011;25:850–4.
Morris RH, Wilkey BR. The effects of ambient temperature on patient temperature during surgery not involving body cavities. Anesthesiology. 1970;32:102–7.
Morris RH. Operating room temperature and the anesthetized, paralyzed patient. Arch Surg. 1971;102:95–7.
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz Group, for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Miyazaki, R., Hoka, S. What is the predictor of the intraoperative body temperature in abdominal surgery?. J Anesth 33, 67–73 (2019). https://doi.org/10.1007/s00540-018-2585-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-018-2585-6