Abstract
Purpose
The aim of this study was to examine the relationship between FFP (fresh frozen plasma)/pRBC (packed red blood cell) transfusion ratio and outcomes in patients undergoing cardiovascular surgery.
Methods
This is a single center retrospective cohort study performed in a cardiovascular center. Patients undergoing cardiovascular surgery between January 2012 and October 2016 with or without massive transfusion (n = 1453). Patients’ outcomes were compared based on FFP/pRBC transfusion ratio (FFP/pRBC > 1 or FFP/pRBC ≤ 1).
Results
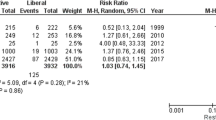
In hospital mortality and rate of stroke and myocardial infarction was significantly higher in patients with less than 1 of FFP/pRBC transfusion ratio only in patients with massive transfusion (3.0 vs 8.8%, p = 0.001; 0.7 vs 6.4%, p < 0.001; 1.0 vs 3.2%, p = 0.047, respectively).
Conclusions
Higher FFP/RBC ratio was associated with reduced risk of death, stroke and myocardial infarction only in patients with cardiovascular surgery receiving massive transfusion. Clinicians should be aware that judicious FFP replacement plays a critical role in the successful management of massive transfusion in cardiac surgery.

Similar content being viewed by others
References
Karkouti K, O’Farrell R, Yau TM, Beattie WS, Reducing Bleeding in Cardiac Surgery Research G. Prediction of massive blood transfusion in cardiac surgery. Can J Anaesth. 2006;53:781–94.
Karkouti K, Wijeysundera DN, Yau TM, Beattie WS, Abdelnaem E, McCluskey SA, Ghannam M, Yeo E, Djaiani G, Karski J. The independent association of massive blood loss with mortality in cardiac surgery. Transfusion. 2004;44:1453–62.
Holcomb JB, del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, Alarcon LH, Bai Y, Brasel KJ, Bulger EM, Cotton BA. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148:127–36.
Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, Sebesta J, Jenkins D, Wade CE, Holcomb JB. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma Acute Care Surg. 2007;63:805–13.
Delaney M, Stark PC, Suh M, Triulzi DJ, Hess JR, Steiner ME, Stowell CP, Sloan SR. Massive transfusion in cardiac surgery: the impact of blood component ratios on clinical outcomes and survival. Anesth Analg. 2017;124:1777–82.
Mazzeffi MA, Chriss E, Davis K, Zhan M, Harris A, Rock P, Gammie JS, Tanaka K. Optimal plasma transfusion in patients undergoing cardiac operations with massive transfusion. Ann Thorac Surg. 2017;104:153–60.
Rao SV, Jollis JG, Harrington RA, Granger CB, Newby LK, Armstrong PW, Moliterno DJ, Lindblad L, Pieper K, Topol EJ, Stamler JS. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555–62.
Cook D, Crowther M, Meade M, Rabbat C, Griffith L, Schiff D, Geerts W, Guyatt G. Deep venous thrombosis in medical-surgical critically ill patients: prevalence, incidence, and risk factors. Crit Care Med. 2005;33:1565–71.
Spiess BD, Royston D, Levy JH, Fitch J, Dietrich W, Body S, Murkin J, Nadel A. Platelet transfusions during coronary artery bypass graft surgery are associated with serious adverse outcomes. Transfusion. 2004;44:1143–8.
Abu-Rustum NR, Richard S, Wilton A, Lev G, Sonoda Y, Hensley ML, Gemignani M, Barakat RR, Chi DS. Transfusion utilization during adnexal or peritoneal cancer surgery: effects on symptomatic venous thromboembolism and survival. Gynecol Oncol. 2005;99:320–6.
Okita Y, Miyata H, Motomura N, Takamoto S, Japan Cardiovascular Surgery Database O. A study of brain protection during total arch replacement comparing antegrade cerebral perfusion versus hypothermic circulatory arrest, with or without retrograde cerebral perfusion: analysis based on the Japan Adult Cardiovascular Surgery Database. J Thorac Cardiovasc Surg. 2015;149:S65–73.
Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33:1242–58.
Dente CJ, Shaz BH, Nicholas JM, Harris RS, Wyrzykowski AD, Patel S, Shah A, Vercruysse GA, Feliciano DV, Rozycki GS, Salomone JP. Improvements in early mortality and coagulopathy are sustained better in patients with blunt trauma after institution of a massive transfusion protocol in a civilian level I trauma center. J Trauma Acute Care Surg. 2009;66:1616–24.
Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Filipescu D, Hunt BJ, Komadina R, Nardi G, Neugebauer EA. The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20:100.
Rowell SE, Barbosa RR, Diggs BS, Schreiber MA, Trauma Outcomes Group. Effect of high product ratio massive transfusion on mortality in blunt and penetrating trauma patients. J Trauma Acute Care Surg. 2011;71:S353–7.
Sharpe JP, Weinberg JA, Magnotti LJ, MacLennan PA, Schroeppel TJ, Fabian TC, Croce MA. Accounting for differences in transfusion volume: are all massive transfusions created equal? J Trauma Acute Care Surg. 2012;72:1536–40.
Rowell SE, Barbosa RR, Allison CE, Van PY, Schreiber MA, Trauma Outcomes Group. Gender-based differences in mortality in response to high product ratio massive transfusion. J Trauma Acute Care Surg. 2011;71:S375–9.
Kozar RA, Peng Z, Zhang R, Holcomb JB, Pati S, Park P, Ko TC, Paredes A. Plasma restoration of endothelial glycocalyx in a rodent model of hemorrhagic shock. Anesth Analg. 2011;112:1289–95.
Peng Z, Pati S, Potter D, Brown R, Holcomb JB, Grill R, Wataha K, Park PW, Xue H, Kozar RA. Fresh frozen plasma lessens pulmonary endothelial inflammation and hyperpermeability after hemorrhagic shock and is associated with loss of syndecan 1. Shock. 2013;40:195–202.
Potter DR, Baimukanova G, Keating SM, Deng X, Chu JA, Gibb SL, Peng Z, Muench MO, Fomin ME, Spinella PC, Kozar R. Fresh frozen plasma and spray-dried plasma mitigate pulmonary vascular permeability and inflammation in hemorrhagic shock. J Trauma Acute Care Surg. 2015;78:S7–S17.
Woodcock TE, Woodcock TM. Revised Starling equation and the glycocalyx model of transvascular fluid exchange: an improved paradigm for prescribing intravenous fluid therapy. Br J Anaesth. 2012;108:384–94.
Chelazzi C, Villa G, Mancinelli P, De Gaudio AR, Adembri C. Glycocalyx and sepsis-induced alterations in vascular permeability. Crit Care. 2015;19:26.
Acknowledgements
We thank Jane Charbonneau, DVM, from Edanz Group (http://www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Tsukinaga, A., Maeda, T., Takaki, S. et al. Relationship between fresh frozen plasma to packed red blood cell transfusion ratio and mortality in cardiovascular surgery. J Anesth 32, 539–546 (2018). https://doi.org/10.1007/s00540-018-2508-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-018-2508-6