Abstract
Purpose
This study aims to identify prognostic factors related to short-term and long-term outcomes of patients with hematological malignancy (HM) admitted to the intensive care unit (ICU) in Japan during ICU stay and after discharge from ICU.
Methods
We conducted a retrospective, observational study of 169 patients with HM admitted to the general ICU from January 2009 to December 2016. We examined prognostic factors affecting outcome during ICU stay and at 180 days after ICU discharge using logistic regression analysis.
Results
During ICU stay, 57 patients (33.7%) died. Invasive mechanical ventilation (OR 8.96, 95% CI 3.67–21.9; P < 0.001, the same hereinafter), the Sequential Organ Failure Assessment (SOFA) score within the first 24 h of ICU admission (1.25, 1.11–1.40; P < 0.001), and malignant lymphoma (0.30, 0.11–0.78; P = 0.014) were detected as factors associated with ICU outcome. Of 112 ICU survivors, 46 (41.1%) died within 180 days after ICU discharge. Duration of ICU stay (1.07, 1.01–1.13; P = 0.027) and the SOFA score at ICU discharge (1.24, 1.04–1.48; P = 0.016) were related to poor outcome at 180 days after ICU discharge.
Conclusions
In critically ill patients with HM, the use of invasive mechanical ventilation, a high SOFA score within the first 24 h of ICU admission, and malignant lymphoma as primary HM affected short-term ICU outcome. Increased duration of ICU stay and SOFA score at ICU discharge influenced long-term outcome at 180 days after ICU discharge.
Similar content being viewed by others
Introduction
The mortality of critically ill patients with hematological malignancy (HM) admitted to the intensive care unit (ICU) remains high, ranging from 33.7 to 84.1% [1,2,3], although therapeutic interventions for these patients such as mechanical ventilation, renal replacement therapy, chemotherapy regimens, and hematopoietic stem cell transplantation (HSCT) have significantly improved their outcome in the past decade [4,5,6,7,8,9,10]. These patients frequently require intensive management, since life-threatening events may occur due to the HM itself, the adverse effects of high-dose chemotherapy, and/or infectious diseases. Although considered a specific and definitive therapy for HM, it is well known that HSCT may also lead to severe complications such as sepsis (including septic shock) due to immunosuppression, acute and chronic graft-versus-host disease (GVHD), acute kidney injury, and acute respiratory failure [5, 9].
Previous studies have revealed several poor prognostic factors in these patients, including the use of invasive mechanical ventilation [1, 11], a high Acute Physiology and Chronic Health Evaluation II (APACHE II) score [2, 3], the need for vasopressors [3], sepsis as reason for ICU admission [12], the presence of neutropenia at ICU admission [11], and previous allogeneic HSCT [13]. However, prognostic factors affecting critically ill patients with HM in Japan during ICU stay remain unclear. The prognostic factors and long-term prognosis related to patients who are successfully treated and discharged from ICU are also unknown.
In this study, we retrospectively evaluated prognostic factors related to short-term and long-term outcome during ICU stay and after ICU discharge in critically ill patients with HM admitted to the general ICU in a single-center in Japan.
Methods
This retrospective, observational study was approved by the institutional review board of Kurashiki Central Hospital, which is a private, tertiary care hospital. Of all patients who were admitted to our general ICU, patients diagnosed with hematological disorders and admitted to the ICU for any reason during their hospital stay from January 2009 to December 2016 were included in this study. We excluded patients younger than 18 years, patients with benign hematological disease, and patients undergoing readmission to the ICU during their hospital stay.
Critically ill inpatients are admitted to our ICU if any of the following criteria are present: new-onset disturbed consciousness, respiratory failure requiring invasive or non-invasive mechanical ventilation, circulatory failure requiring supportive management, severe electrolyte, metabolic disturbances and/or exacerbation of fluid balances requiring renal replacement therapy, severe infectious disease with organ dysfunction such as sepsis or septic shock, and the need for intensive postoperative management. The criteria for ICU discharge are the following: the improvement of respiratory failure (the absence of dyspnea and sputum retention, improvement of chest X-ray and/or blood gas findings, and reduced inspiratory oxygen requirements, although not necessarily requiring withdrawal of ventilation), the improvement of circulatory failure (stable blood pressure and heart rate without inotropes and/or vasopressors), withdrawal of continuous renal replacement therapy, the absence of deterioration in physical and/or laboratory findings, as well as taking into consideration the wishes of patients and/or their relatives when terminal disease is present. In our hospital, 300–320 patients are newly diagnosed with HM each year; approximately 50 patients undergo HSCT. Eligibility for HSCT and type of HSCT employed are comprehensively determined by hematologists.
We retrospectively examined the following variables by consulting clinical and ICU records: age, sex, primary HM, reason for ICU admission, status of HM, proportion of patients with previous HSCT, type of transplantation, occurrence of acute and chronic GVHD, the APACHE II score, the Sequential Organ Failure Assessment (SOFA) score within the first 24 h of ICU admission, duration of ICU stay, ICU mortality rate, mortality rate at 180 days after ICU discharge, the SOFA score at ICU discharge in ICU survivors, and cause of death. The results of hematological investigations at ICU admission and the proportion of applied therapeutic interventions during ICU stay (including invasive mechanical ventilation, renal replacement therapy, and the use of inotropes and/or vasopressors) were also analyzed. Inotropes and vasopressors use was defined as the use of dobutamine, noradrenalin, adrenalin, and vasopressin at any dose. Neutropenia at ICU admission was defined as a neutrophil count of less than 1000/µl.
We evaluated differences of these variables between survivors and non-survivors during ICU stay and at 180 days after ICU discharge by using the χ 2 test or Fisher’s exact test and Mann–Whitney U test, and all results were expressed as the median and interquartile range, numbers and percentages, or as range. We conducted logistic regression analysis to determine prognostic factors during ICU stay and at 180 days after ICU discharge. Odds ratios (ORs) and 95% confidence intervals (CIs) were also calculated.
Using logistic regression analysis, the explanatory variables where the P value was less than 0.15 by univariate analyses were directly and simultaneously entered into the model. For reliable analysis, the number of explanatory variables was determined by a tenth of the smaller number in either survivors or non-survivors. We allowed several explanatory variables that correlated clinically and strongly with each other to not overlap when entering data into the model. Multicollinearity was checked using the variance inflation factor, with a value above 10 is regarded as indicating large multicollinearity. Finally, the model was assessed for accuracy by calculating the area under the receiver operating characteristic curve (AUC).
Assuming the presence of at least five explanatory variables for logistic regression analysis regarding prognostic factors during ICU stay, and an ICU mortality rate of 30% in patients with HM [1], we estimated a sample size of 167 patients to be included in this study.
All tests were two-sided, and differences of P < 0.05 were considered statistically significant. Statistical analyses were performed by using EZR on R Commander software, Version 1.24 (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R, Version 3.0.3 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
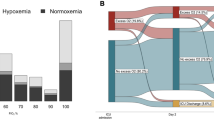
A total of 7048 patients were admitted to the ICU from January 2009 to December 2016, with an overall mortality rate of 6.4%. Of these, there were 215 patients diagnosed with hematological disorders who were admitted to the ICU during their hospital stay. Two patients younger than 18 years, 22 patients with benign hematological disease, and 22 patients undergoing readmission to the ICU during their hospital stay were excluded. Thus, a total of 169 patients were enrolled in this study. Demographic characteristics are shown in Table 1. Fifty-six patients (33.1%) suffered from malignant lymphoma as primary HM, and 75 patients (44.4%) had developed respiratory failure as reason for ICU admission. The median of the APACHE II scores and the SOFA scores within the first 24 h of ICU admission was 24 and 9 points, respectively. The number of patients who required invasive mechanical ventilation, vasopressors, and renal replacement therapy was 86 (50.9%), 101 (59.8%), and 33 (19.5%), respectively. The median duration of ICU stay was 6 days (interquartile range 3–12 days).
Table 1 also shows the results of univariate analyses comparing survivors and non-survivors in the ICU. Fifty-seven (33.7%) patients died during their ICU stay. The proportion of survivors with malignant lymphoma was higher than that of non-survivors (41.1 vs. 17.5%). Respiratory failure was the most common indication for ICU admission in both groups, and the proportion of patients with respiratory failure was higher in non-survivors than in survivors (59.6 vs. 36.6%). Both the APACHE II scores and the SOFA scores within the first 24 h of ICU admission in non-survivors were significantly higher when compared to survivors (median 27 vs. 22.5 points; P < 0.001, 11 vs. 8 points; P < 0.001, respectively). Regarding treatment, the proportion of allogeneic HSCT did not differ between ICU survivors and non-survivors. Invasive mechanical ventilation and vasopressors were used more frequently in non-survivors (84.2 vs. 33.9%; P < 0.001, 77.2 vs. 50.9%; P < 0.001, respectively).
Using logistic regression analysis, we selected the use of invasive mechanical ventilation, the SOFA score within the first 24 h of ICU admission, malignant lymphoma as primary HM, allogeneic HSCT, and age as the explanatory variables for ICU outcome. We removed the APACHE II score from the logistic regression analysis because it is already known to be a prognostic factor related to poor ICU outcome in several reports [2, 3, 7], while the relationship between a SOFA score within the first 24 h of ICU admission and ICU outcome remains unknown. In addition, APACHE II scores correlate clinically and strongly with SOFA scores and age, despite no correlations between SOFA scores and age. Serum total bilirubin levels and platelet count at ICU admission and the use of vasopressors were also excluded because of a strong relationship with these to the SOFA score.
The factors related to poor ICU outcome were the use of invasive mechanical ventilation (OR 8.96, 95% CI 3.67–21.9; P < 0.001) and the SOFA score within the first 24 h of ICU admission (OR 1.25, 95% CI 1.11–1.40; P < 0.001) (Table 2). Malignant lymphoma was found to be predictive of good outcome (OR 0.30, 95% CI 0.11–0.78; P = 0.014). Allogeneic HSCT (OR 1.29, 95% CI 0.51–3.30; P = 0.594) and age (OR 1.01, 95% CI 0.98–1.04; P = 0.434) were not detected as prognostic factors of ICU. The variance inflation factors for the use of invasive mechanical ventilation, the SOFA score within the first 24 h of ICU admission, malignant lymphoma, allogeneic HSCT, and age were 1.04, 1.02, 1.12, 1.27, and 1.22, respectively. The AUC was 0.85 (95% CI 0.79–0.91) when the five variables were employed in the model.
In patients with malignant lymphoma, the proportion of respiratory failure as reason for ICU admission (18 of 56 patients, 32.1%) was significantly smaller than those with other HMs (57 of 113 patients, 50.4%) (P = 0.032), whereas invasive mechanical ventilation was instituted similarly (24 of 56, and 62 of 113 patients, respectively) (42.9 vs. 54.9%; P = 0.191). Any type of HSCT was performed less frequently in patients with malignant lymphoma (14 of 56 patients, 25.0%) than those with other HMs (49 of 113 patients, 43.4%) (P = 0.028).
There were 112 patients who were successfully discharged from ICU. Of these, 46 patients died within 180 days after ICU discharge, representing a mortality rate of 41.1%. The comparison between survivors and non-survivors at 180 days after ICU discharge is summarized in Table 3. The proportion of sepsis as reason for ICU admission was higher in survivors (36.4 vs. 19.5%). The SOFA scores within the first 24 h of ICU admission were higher in non-survivors than in survivors (median 8.5 vs. 7 points; P = 0.043). The duration of ICU stay was longer (median 7.5 vs. 4 days; P = 0.001), and the SOFA scores at ICU discharge were higher (median 5 vs. 4 points: P = 0.001) in non-survivors than in survivors. Regarding other factors, no significant differences were found between survivors and non-survivors at 180 days after ICU discharge. No differences in the length of invasive mechanical ventilation and continuous renal replacement therapy during ICU were found (median 0 days [range 0–30 days] vs. 0 days [0–35 days]; P = 0.313, and 0 days [0–6 days] vs. 0 days [0–12 days]; P = 0.287, respectively). The numbers of patients who had depended on ventilator at ICU discharge were 3 and 4 (4.5 vs. 8.7%; P = 0.443), and those who had depended on renal replacement therapy were 2 and 6 (3.0 vs. 13.0%; P = 0.062), respectively. Logistic regression analysis revealed that duration of ICU stay (OR 1.07, 95% CI 1.01–1.13; P = 0.027) and a high SOFA score at ICU discharge (OR 1.24, 95% CI 1.04–1.48; P = 0.016) was associated with poor outcome at 180 days after ICU discharge (Table 4). Serum creatinine levels at ICU admission and sepsis as reason for ICU admission were not detected as being prognostic factors of outcome at 180 days after ICU admission. The variance inflation factors for duration of ICU stay, the SOFA score at ICU discharge, creatinine, sepsis were 1.02, 1.19, 1.21, and 1.00, respectively, and the AUC was 0.73 (95% CI 0.63–0.83).
The cause of death between non-survivors who died during ICU stay and within 180 days after ICU discharge was significantly different (P < 0.001) (Table 5). The proportion of non-survivors who had primary HM as the cause of death at 180 days after ICU discharge was higher than those who died during ICU stay (47.8 vs. 5.3%). The cause of death in five patients (10.9%) after ICU discharge was unknown because they had been discharged home or transferred at 180 days after ICU discharge.
Discussion
In this study, the ICU mortality rate in critically ill patients with HM was 33.7%, whereas the mortality rate of all patients admitted to ICU during the same period was 6.4%. We also found that the need for invasive mechanical ventilation and/or a high SOFA score within the first 24 h of ICU admission was associated with poor ICU outcome. Conversely, malignant lymphoma as primary HM was associated with good ICU outcome. There were no relationships found between the history of allogeneic HSCT, age, and ICU outcome. In ICU survivors, the mortality rate at 180 days after ICU discharge was 41.1%. The duration of ICU stay and/or a high SOFA score at ICU discharge was detected as a predictor of outcome at 180 days after ICU discharge.
Our findings could suggest several points. Firstly, ICU outcome in patients with HM remains poor, and the high ICU mortality rates in patients with HM are significantly associated with the need for invasive mechanical ventilation. This may be associated with life-threatening events arising during treatment of HM rather than the primary malignancies themselves, because in our study, the SOFA score was associated with ICU outcome. Indeed, Hill has described that the severity of physiological disturbance could predict short-term outcome in patients with HM [14]. In particular, respiratory failure (resulting from acute respiratory distress syndrome, pneumonia secondary to immunosuppression, invasive aspergillosis, and/or pulmonary hemorrhage) is well known to occur during treatment of HM [15,16,17]. Another possible reason why invasive mechanical ventilation is strongly associated with poor ICU outcome is that, we think, individuals with HM tend to be instituted invasive mechanical ventilation compared to other cancer patients because most of the patients with HM admitted to the ICU are aimed at complete recovery from HM and therefore there are little tendencies for withholding of treatment and/or shifting to palliative care.
Secondly, previous HSCT was not associated with ICU outcome in our study, suggesting that critically ill patients with HM may develop potentially lethal events regardless of whether they have undergone HSCT or not. Although patients who underwent HSCT suffered from several specific complications (including GVHD, engraftment syndrome, bacterial, fungal and/or viral infection, and thrombotic microangiopathy) [18, 19], outcomes in HSCT recipients have improved in the past decade owing to several factors: reduced intensity conditioning regimens, careful selection of recipients (including younger age and fewer comorbidities), and routine use of antibiotics [1, 10]. Pène et al. described that patients admitted to the ICU after 30 or more days of HSCT requiring mechanical ventilation had a poor outcome compared to those admitted within 30 days after HSCT [20]. This could be explained by the fact that several complications secondary to HSCT occur more frequently after 30 or more days of HSCT as opposed to the first 30 days after HSCT [20]. In this study, the proportion of GVHD and time from HSCT to ICU admission did not differ between ICU survivors and non-survivors. This may be one of the reasons why previous HSCT was not associated with ICU outcome. However, our result differs from a report by Azoulay et al. that previous HSCT predicted poor outcome of ICU patients with HM [13]. In their study, the number of enrolled patients was 1011. On the other hand, only 169 patients were enrolled in our study although we could achieve the estimated sample size of 167 patients. The difference of sample size between the two studies might affect our result, because the P value of previous allogeneic HSCT between ICU survivors and non-survivors was 0.082. We believe this may be another reason that previous allogeneic HSCT was not detected as a prognostic factor of ICU outcome.
Thirdly, it is of note that a diagnosis of malignant lymphoma as primary HM was associated with a good ICU outcome. In this study, patients with malignant lymphoma did not suffer from respiratory failure compared to other HMs despite the similar proportion of the use of invasive mechanical ventilation. These findings suggest that patients with malignant lymphoma tend to be instituted invasive mechanical ventilation against clinical conditions, except for respiratory failure. In addition, it is plausible that the lower proportion of previous HSCT in patients with malignant lymphoma compared to other HMs affected the low incidence of respiratory failure [15]. Therefore, considering that critically ill patients with HM have high mortality rates owing to respiratory failure, there may be a possibility that meticulous intensive care support for patients with malignant lymphoma, particularly suffering from clinical conditions separate from respiratory failure such as sepsis, renal failure, heart failure, and neurologic disorders, can result in a successful outcome. Wohlfarth et al. also showed that in patients with diffuse large B-cell lymphoma admitted to the ICU, hemodynamic instability (37.8%) was the most common reason for ICU admission, and that the ICU survival rate of them was 75.7% [21].
Fourthly, for critically ill patients with HM, it is likely that prognosis after discharge from ICU is determined by the level of physiological care needed at ICU discharge. This is because in our study, the duration of ICU stay and/or a high SOFA score at ICU discharge predicted poor outcome at 180 days after ICU discharge as a long-term outcome, although the length of invasive mechanical ventilation and continuous renal replacement therapy during ICU stay, and the proportion of patients who had needed for ventilator and/or renal replacement therapy at ICU discharge were similar between survivors and non-survivors. We presume that hematologists considered the longer patients had experienced ICU admission and the severer patients had had physiological disturbances at ICU discharge, the higher they were at risk for re-exacerbating general conditions requiring ICU readmission if the treatments for underlying or relapsed primary HM were proceeded after ICU discharge. Consequently, many hematologists tended to avoid providing or hesitate to perform additional chemotherapy and/or HSCT after ICU discharge because these patients were in the poor physical status at ICU discharge. As a result, it is reasonable to reveal, in our result, the most common cause of death in patients who had died at 180 days after ICU discharge was primary HM, with differing those who died during ICU stay.
There are several limitations to our study. This was a retrospective study with a relatively small sample size (n = 169), and the sample size that analyzed factors associated with outcome at 180 days after ICU discharge was also smaller than that which analyzed factors during ICU stay (n = 112); the AUC of this model was 0.73. Because there is a chance of a type II error as we described, only factors having strong correlations could be detected as risk factors with logistic regression analysis. In addition, little generalization may be possible since this was a single-center experience. There is a lack of information regarding primary disease status, treatment, clinical course following ICU discharge, and data from patients undergoing readmission to ICU during their hospital stay and who were discharged home or transferred. However, our institution is a tertiary care hospital, where treatments for HM are performed by experienced teams. The results of the present study are largely similar to several other studies looking at prognostic factors in patients with HM admitted to ICU. To the best our knowledge, this is the first report in Japan describing prognostic factors related to short-term outcomes during ICU in critically ill patients with HM, as well as long-term outcomes (defined as at 180 days after ICU discharge in this study) in patients who could be successfully discharged from the ICU.
Conclusions
In critically ill patients with HM admitted to the ICU, the mortality rate during ICU stay and at 180 days after ICU discharge among ICU survivors was 33.7 and 41.1%, respectively. Regarding the short-term outcome of critically ill patients with HM during ICU stay, the use of invasive mechanical ventilation and a high SOFA score within the first 24 h of admission to the ICU was associated with poor ICU outcome. Conversely, malignant lymphoma as primary HM was associated with good ICU outcome. Previous allogeneic HSCT and age were not detected as prognostic factors during ICU stay. As a long-term outcome, increased duration of ICU stay and a high SOFA score at ICU discharge was related to poor outcome at 180 days after ICU discharge in patients discharged from the ICU.
References
Bird GT, Farquhar-Smith P, Wigmore T, Potter M, Gruber PC. Outcomes and prognostic factors in patients with haematological malignancy admitted to a specialist cancer intensive care unit: a 5 yr study. Br J Anaesth. 2012;108:452–9.
Liu J, Cheng Q, Yang Q, Li X, Shen X, Zhang L, Liu Z, Khoshnood K. Prognosis-related factors in intensive care unit (ICU) patients with hematological malignancies: a retrospective cohort analysis in a Chinese population. Hematology. 2015;20:494–503.
Yeo CD, Kim JW, Kim SC, Kim YK, Kim KH, Kim HJ, Lee S, Rhee CK. Prognostic factors in critically ill patients with hematologic malignancies admitted to the intensive care unit. J Crit Care. 2012;27(739):e1–6.
Belenguer-Muncharaz A, Albert-Rodrigo L, Ferrandiz-Selles A, Cebrian-Graullera G. [Ten-year evolution of mechanical ventilation in acute respiratory failure in the hematological patient admitted to the intensive care unit]. Med Intensiva. 2013;37:452–60.
Benz R, Schanz U, Maggiorini M, Seebach JD, Stussi G. Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014;49:62–5.
Darmon M, Vincent F, Canet E, Mokart D, Pene F, Kouatchet A, Mayaux J, Nyunga M, Bruneel F, Rabbat A, Lebert C, Perez P, Renault A, Meert AP, Benoit D, Hamidfar R, Jourdain M, Schlemmer B, Chevret S, Lemiale V, Azoulay E. Acute kidney injury in critically ill patients with haematological malignancies: results of a multicentre cohort study from the Groupe de Recherche en Reanimation Respiratoire en Onco-Hematologie. Nephrol Dial Transplant. 2015;30:2006–13.
Hill QA, Kelly RJ, Patalappa C, Whittle AM, Scally AJ, Hughes A, Ashcroft AJ, Hill A. Survival of patients with hematological malignancy admitted to the intensive care unit: prognostic factors and outcome compared to unselected medical intensive care unit admissions, a parallel group study. Leuk Lymphoma. 2012;53:282–8.
Park MR, Jeon K, Song JU, Lim SY, Park SY, Lee JE, Huh W, Kim K, Kim WS, Jung CW, Suh GY. Outcomes in critically ill patients with hematologic malignancies who received renal replacement therapy for acute kidney injury in an intensive care unit. J Crit Care. 2011;26(107):e1–6.
Sawinski D. The kidney effects of hematopoietic stem cell transplantation. Adv Chronic Kidney Dis. 2014;21:96–105.
Townsend WM, Holroyd A, Pearce R, Mackinnon S, Naik P, Goldstone AH, Linch DC, Peggs KS, Thomson KJ, Singer M, Howell DC, Morris EC. Improved intensive care unit survival for critically ill allogeneic haematopoietic stem cell transplant recipients following reduced intensity conditioning. Br J Haematol. 2013;161:578–86.
Namendys-Silva SA, González-Herrera MO, García-Guillén FJ, Texcocano-Becerra J, Herrera-Gómez A. Outcome of critically ill patients with hematological malignancies. Ann Hematol. 2013;92:699–705.
Horster S, Stemmler HJ, Mandel PC, Muck A, Tischer J, Hausmann A, Parhofer KG, Geiger S. Mortality of patients with hematological malignancy after admission to the intensive care unit. Onkologie. 2012;35:556–61.
Azoulay E, Mokart D, Pène F, Lambert J, Kouatchet A, Mayaux J, Vincent F, Nyunga M, Bruneel F, Laisne LM, Rabbat A, Lebert C, Perez P, Chaize M, Renault A, Meert AP, Benoit D, Hamidfar R, Jourdain M, Darmon M, Schlemmer B, Chevret S, Lemiale V. Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en réanimation onco-hématologique study. J Clin Oncol. 2013;31:2810–8.
Hill QA. Intensify, resuscitate or palliate: decision making in the critically ill patient with haematological malignancy. Blood Rev. 2010;24:17–25.
Azoulay E, Lemiale V, Mokart D, Pene F, Kouatchet A, Perez P, Vincent F, Mayaux J, Benoit D, Bruneel F, Meert AP, Nyunga M, Rabbat A, Darmon M. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40:1106–14.
Choi MH, Jung JI, Chung WD, Kim YJ, Lee SE, Han DH, Ahn MI, Park SH. Acute pulmonary complications in patients with hematologic malignancies. Radiographics. 2014;34:1755–68.
Steinbach WJ, Marr KA, Anaissie EJ, Azie N, Quan SP, Meier-Kriesche HU, Apewokin S, Horn DL. Clinical epidemiology of 960 patients with invasive aspergillosis from the PATH Alliance registry. J Infect. 2012;65:453–64.
Rosenthal J. Hematopoietic cell transplantation-associated thrombotic microangiopathy: a review of pathophysiology, diagnosis, and treatment. J Blood Med. 2016;7:181–6.
Saillard C, Mokart D, Lemiale V, Azoulay E. Mechanical ventilation in cancer patients. Minerva Anestesiol. 2014;80:712–25.
Pène F, Aubron C, Azoulay E, Blot F, Thiéry G, Raynard B, Schlemmer B, Nitenberg G, Buzyn A, Arnaud P, Socié G, Mira JP. Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol. 2006;24:643–9.
Wohlfarth P, Carlström A, Staudinger T, Clauss S, Hermann A, Rabitsch W, Bojic A, Skrabs C, Porpaczy E, Schiefer AI, Valent P, Knöbl P, Agis H, Hauswirth A, Jäger U, Kundi M, Sperr WR, Schellongowski P. Arbeitsgruppe für hämato-onkologische Intensivmedizin der Österreichischen Gesellschaft für Internistische und Allgemeine Intensivmedizin und Notfallmedizin (ÖGIAIN). Incidence of intensive care unit admission, outcome and post intensive care survival in patients with diffuse large B-cell lymphoma. Leuk Lymphoma. 2016;57:1831–8.
Acknowledgements
The authors would like to thank Dr. Yasunori Ueda and Dr. Kazuya Okada, Department of Hematology/Oncology, Kurashiki Central Hospital, for providing their support to conduct this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
About this article
Cite this article
Irie, H., Otake, T., Kawai, K. et al. Prognostic factors in critically ill patients with hematological malignancy admitted to the general intensive care unit: a single-center experience in Japan. J Anesth 31, 736–743 (2017). https://doi.org/10.1007/s00540-017-2390-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2390-7