Abstract
Objectives
When physicians become patients, they may expect special privileges, extra attention from caregivers, and non-routine treatments. Consequently, physician patients may not be treated per routine—which possibly worsens care rather than improving it. We thus tested the primary hypothesis that in-hospital mortality and major complications after non-cardiac surgery are more common in physician patients than in non-physician patients.
Patients and methods
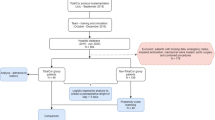
Perioperative data were extracted for patients who had non-cardiac surgery at the Cleveland Clinic between 2005 and 2013. We used propensity score matching to identify comparable groups of physician and non-physician patients. Matched physician and non-physician patients were compared on a composite of in-hospital mortality and major postoperative complications using a generalized equation average relative effects model. Secondly, the matched patients were also compared on reoperation using logistic regression and on duration of hospitalization using Kaplan–Meier analysis with the log-rank test and Cox proportional hazards regression.
Results
Among 21,173 qualifying patients, we matched 522 physician patients to 2448 non-physician controls. There were no significant differences between physician and non-physician patients in the composite of in-hospital mortality and major complications, with an estimated odds ratio across the outcome components (average relative effect) of 1.20 (95% confidence interval 0.77–1.87) for physicians vs. non-physicians, P = 0.41. There was also no difference in the risk of re-operation or duration of hospitalization.
Conclusions
A variety of important outcomes were similar in physician patients and matched non-physician patients after non-cardiac surgery.




Similar content being viewed by others
References
Guzman JA, Sasidhar M, Stoller JK. Caring for VIPs: nine principles. Cleve Clin J Med. 2011;78:90–4.
Groves JE, Dunderdale BA, Stern TA. Celebrity patients, VIPs, and potentates. Prim Care Companion J Clin Psychiatry. 2002;4:215–23.
Weintraub W. “The VIP syndrome”: a clinical study in hospital psychiatry. J Nerv Ment Dis. 1964;138:181–93.
Diekema DS. The preferential treatment of VIPs in the emergency department. Am J Emerg Med. 1996;14:226–9.
Georges E, Anzia J, Dinwiddie S. General effect of VIP patients on delivery of care. Psychiatric Annals. 2012;42:15–9.
Schneck SA. “Doctoring” doctors and their families. JAMA. 1998;280:2039–42.
Cappell MS. The physician-administrator as patient: distinctive aspects of medical care. Perspect Biol Med. 2011;54:232–42.
Stoudemire A, Rhoads JM. When the doctor needs a doctor: special considerations for the physician-patient. Ann Intern Med. 1983;98:654–9.
Marzuk PM. Sounding board: when the patient is a physician. N Engl J Med. 1987;317:1409–11.
D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–81.
Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013;32:2837–49.
Austin PC. A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014;33:1057–69.
Mascha EJ, Imrey PB. Factors affecting power of tests for multiple binary outcomes. Stat Med. 2010;29:2890–904.
Deng CY, Huang N, Chou YJ, Hsu YJ, Chen LS, Chou P. Comparison of perforation risk among physicians, other medical professionals and general adults with acute appendicitis in Taiwan. Br J Surg. 2006;93:1297–302.
Shen HN, Lu CL, Li CY. Do physicians have lower risk of severe sepsis and associated mortality? A matched cohort study. Crit Care Med. 2014;42:816–23.
Liu CJ, Huang N, Lin CC, et al. Outcome disparities between medical personnel and nonmedical personnel patients receiving definitive surgery for colorectal cancer: a nationwide population-based study. Medicine. 2015;94:e402.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funded by internal sources only.
Conflict of interest
None of the authors has a financial interest in this research.
Appendix
Appendix
See Table 3.
About this article
Cite this article
Panjasawatwong, K., Lin, P., Karimi, N. et al. Outcomes of physician patients after non-cardiac surgery: a registry analysis. J Anesth 31, 111–119 (2017). https://doi.org/10.1007/s00540-016-2273-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2273-3