Abstract
Purpose
Both single-injection transversus abdominis plane (TAP) block and continuous wound infiltration (CWI) provide postoperative analgesia, but no study has compared the two regional techniques. We tested the hypothesis that CWI is more effective for controlling postoperative pain compared with single-injection TAP block after laparotomy.
Methods
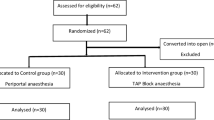
We conducted a prospective randomized study of patients undergoing gynecologic laparotomy with midline incision through the umbilicus under general anesthesia. The patients were allocated to receive either single-injection TAP block (TAP group) or CWI (CWI group) for postoperative analgesia. All patients received intravenous patient-controlled analgesia with morphine and intravenous flurbiprofen twice daily after surgery. Postoperative pain at rest and on coughing, postoperative morphine consumption, incidence of postoperative nausea and vomiting (PONV), pruritus and urinary retention, ambulation, and satisfaction score were recorded. Patients were assessed at 3 h after surgery and twice daily on postoperative days (POD) 1 and 2.
Results
Data of 54 patients were analyzed. Compared to the TAP group (n = 27), pain score on coughing was significantly lower in the CWI group (n = 27) on POD1 and POD2 (P < 0.05). Pain score on coughing at 3 h after surgery, pain score at rest at all assessed time points, morphine consumption, incidence of PONV, pruritus and urinary retention, ambulation, and satisfaction score were not different between the two groups.
Conclusion
CWI reduced pain on coughing after the day of surgery compared with single-injection TAP block when performed as part of multimodal analgesia in patients undergoing gynecologic laparotomy.

Similar content being viewed by others
References
Kehlet H, Dahl JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg. 1993;77:1048–56.
White PF, Kehlet H, Neal JM, Schricker T, Carr DB, Carli F. The role of the anesthesiologist in fast-track surgery: from multimodal analgesia to perioperative medical care. Anesth Analg. 2007;104:1380–96.
Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–60.
McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, Laffey JG. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106:186–91.
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–7.
El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, Kapral S, Marhofer P. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–7.
De Oliveira GS, Jr Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. 2014;118:454–63.
Gasanova I, Grant E, Way M, Rosero EB, Joshi GP. Ultrasound-guided transversus abdominal plane block with multimodal analgesia for pain management after total abdominal hysterectomy. Arch Gynecol Obstet. 2013;288:105–11.
Røjskjaer JO, Gade E, Kiel LB, Lind MN, Pedersen LM, Kristensen BB, Rasmussen YH, Foss NB. Analgesic effect of ultrasound-guided transversus abdominis plane block after total abdominal hysterectomy: a randomized, double-blind, placebo-controlled trial. Acta Obstet Gynecol Scand. 2015;94:274–8.
Kawahara R, Tamai Y, Yamasaki K, Okuno S, Hanada R, Funato T. The analgesic efficacy of ultrasound-guided transversus abdominis plane block with mid-axillary approach after gynecologic laparoscopic surgery: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2015;31:67–71.
Abdallah FW, Chan VW, Brull R. Transversus abdominis plane block: the effects of surgery, dosing, technique, and timing on analgesic outcomes: a systematic review. Reg Anesth Pain Med. 2012;37:193–209.
Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;. doi:10.1002/14651858.CD007705.pub2.
Kanazi GE, Aouad MT, Abdallah FW, Khatib MI, Adham AM, Harfoush DW, Siddik-Sayyid SM. The analgesic efficacy of subarachnoid morphine in comparison with ultrasound-guided transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2010;111:475–81.
McMorrow RCN, Ni Mhuircheartaigh RJ, Ahmed KA, Aslani A, Ng SC, Conrick-Martin I, Dowling JJ, Gaffney A, Loughrey JP, McCaul CL. Comparison of transversus abdominis plane block vs spinal morphine for pain relief after caesarean section. Br J Anaesth. 2011;106:706–12.
Wu Y, Liu F, Tang H, Wang Q, Chen L, Wu H, Zhang X, Miao J, Zhu M, Hu C, Goldsworthy M, You J, Xu X. The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomy. Anesth Analg. 2013;117:507–13.
Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014;14:121.
Telnes A, Skogvoll E, Lonnée H. Transversus abdominis plane block vs. wound infiltration in Caesarean section: a randomised controlled trial. Acta Anaesthesiol Scand. 2015;59:496–504.
Park JS, Choi GS, Kwak KH, Jung H, Jeon Y, Park S, Yeo J. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res. 2015;195:61–6.
Sivapurapu V, Vasudevan A, Gupta S, Badhe AS. Comparison of analgesic efficacy of transversus abdominis plane block with direct infiltration of local anesthetic into surgical incision in lower abdominal gynecological surgeries. J Anaesthesiol Clin Pharmacol. 2013;29:71–5.
Atim A, Bilgin F, Kilickaya O, Purtuloglu T, Alanbay I, Orhan ME, Kurt E. The efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing hysterectomy. Anaesth Intensive Care. 2011;39:630–4.
Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;203:914–32.
Scott NB. Wound infiltration for surgery. Anaesthesia. 2010;65(Suppl 1):67–75.
Beaussier M, El’Ayoubi H, Schiffer E, Rollin M, Parc Y, Mazoit JX, Azizi L, Gervaz P, Rohr S, Biermann C, Lienhart A, Eledjam JJ. Continuous preperitoneal infusion of ropivacaine provides effective analgesia and accelerates recovery after colorectal surgery. Anesthesiology. 2007;107:461–8.
Rackelboom T, Le Strat S, Silvera S, Schmitz T, Bassot A, Goffinet F, Ozier Y, Beaussier M, Mignon A. Improving continuous wound infusion effectiveness for postoperative analgesia after cesarean delivery: a randomized controlled trial. Obstet Gynecol. 2010;116:893–900.
Fredman B, Shapiro A, Zohar E, Feldman E, Shorer S, Rawal N, Jedeikin R. The analgesic efficacy of patient-controlled ropivacaine instillation after cesarean delivery. Anesth Analg. 2000;91:1436–40.
Givens VA, Lipscomb GH, Meyer NL. A randomized trial of postoperative wound irrigation with local anesthetic for pain after cesarean delivery. Am J Obstet Gynecol. 2002;186:1188–91.
Zohar E, Fredman B, Phillipov A, Jedeikin R, Shapiro A. The analgesic efficacy of patient-controlled bupivacaine wound instillation after total abdominal hysterectomy with bilateral salpingo-oophorectomy. Anesth Analg. 2001;93:482–7.
Fassoulaki A, Melemeni A, Stamatakis E, Petropoulos G, Sarantopoulos C. A combination of gabapentin and local anesthetics attenuates acute and late pain after abdominal hysterectomy. Eur J Anaesthesiol. 2007;24:521–8.
Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth. 2013;110:191–200.
Abdallah FW, Johnson J, Chan V, Murgatroyd H, Ghafari M, Ami N, Jin R, Brull R. Intravenous dexamethasone and perineural dexamethasone similarly prolong the duration of analgesia after supraclavicular brachial plexus block: a randomized, triple-arm, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2015;40:125–32.
Loizides S, Gurusamy KS, Nagendran M, Rossi M, Guerrini GP, Vadidson BR. Wound infiltration with local anaesthetic agents for laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2014;. doi:10.1002/14651858.CD007049.pub2.
Heil JW, Ilfeld BM, Loland VJ, Sandhu NS, Mariano ER. Ultrasound-guided transversus abdominis plane catheters and ambulatory perineural infusions for outpatient inguinal hernia repair. Reg Anesth Pain Med. 2010;35:556–8.
Kadam RV, Field JB. Ultasound-guided continuous transversus abdominis plane block for abdominal surgery. J Anaesthesiol Clin Pharmacol. 2011;27:333–6.
Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, Darbar A, Maheshwaran A, Powell R. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011;66:465–71.
Heil JW, Nakanote KA, Madison SJ, Loland VJ, Mariano ER, Sandhu NS, Bishop ML, Agarwal RR, Proudfoot JA, Ferguson EJ, Morgan AC, Ilfeld BM. Continuous transversus abdominis plane (TAP) blocks for postoperative pain control after hernia surgery: a randomized, triple-masked, placebo-controlled study. Pain Med. 2014;15:1957–64.
Niraj G, Kelkar A, Hart E, Horst C, Malik D, Yeow C, Singh B, Chaudhri S. Comparison of analgesic efficacy of four-quadrant transversus abdominis plane (TAP) block and continuous posterior TAP analgesia with epidural analgesia in patients undergoing laparoscopic colorectal surgery: an open-label, randomised, non-inferiority trial. Anaesthesia. 2014;69:348–55.
Acknowledgments
The authors thank Dr. Yuji Takei and Dr. Shizuo Machida, Department of Obstetrics and Gynecology, Jichi Medical University Hospital, for placing the wound infiltration catheters into the surgical site. The authors also thank Ms. Rieko Yasuda and Ms. Setsuko Sugimoto for assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kunihisa Hotta has no conflict of interest. Soichiro Inoue has no conflict of interest. Koki Taira has no conflict of interest. Naho Sata has no conflict of interest. Kenji Tamai has no conflict of interest. Mamoru Takeuchi has no conflict of interest.
About this article
Cite this article
Hotta, K., Inoue, S., Taira, K. et al. Comparison of the analgesic effect between continuous wound infiltration and single-injection transversus abdominis plane block after gynecologic laparotomy. J Anesth 30, 31–38 (2016). https://doi.org/10.1007/s00540-015-2083-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2083-z