Abstract
Purpose
We hypothesized that, after axillary block, positioning the patient in a lateral position with the injected side down and simultaneously in a 20° Trendelenburg position will increase the success rate and quality of the block.
Methods
Fifty patients with chronic renal failure (ASA 2–3) scheduled for arteriovenous fistula surgery were included in this study. In all patients, 30–40 ml of 0.25 % levobupivacaine were injected into the axillary sheath. The block was performed as three injections (multiple injection technique) with the arm in 90° abduction and 90° flexion in the supine position. Patients were randomly allocated to two groups. Group I (n = 25) patients were kept in the supine position after the block. Group II (n = 25) patients were positioned laterally after the block with the injected arm down and in a 20° Trendelenburg position. Sensory and motor block were evaluated at 2, 4, 6, 8, 10, 15, 20, and 25 min after the administration of the block. Thus, the patients in group II were evaluated in a lateral position during the first 30 min. Throughout the surgery and the recovery period, sensory and motor block were evaluated at 30-min intervals.
Results
There were no significant intergroup differences in the effects on radial, ulnar, median, and musculoskeletal nerve blockade. Thirty minutes after the injection, the patients in group II had higher levels of sensory axillary nerve blockade. Subscapular and thoracodorsal nerve motor block were not detected in group I, while 84 % of the patients in group II experienced blockade of both of these nerves (p < 0.01).
Conclusion
We conclude that, for patients undergoing an axillary block, positioning the patient laterally with the injected side down and in a 20° Trendelenburg position increases the success rate and quality of the block.

Similar content being viewed by others
References
Cousins MJ, Bridenbaugh PO, Carr DB, Horlocker TT. Neural blockade in clinical anesthesia and pain medicine. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2008.
Winnie AP. Plexus anesthesia. Volume 1: Perivascular techniques of brachial plexus block. Philadelphia: WB Saunders; 1984. p. 157.
Koscielniak-Nielsen ZJ, Horn A, Nielsen PR. Effect of arm position on the effectiveness of perivascular axillary nerve block. Br J Anaesth. 1995;74:387–91.
Ababou A, Marzouk N, Mosadiq A, Sbihi A. The effects of arm position on onset and duration of axillary brachial plexus block. Anesth Analg. 2007;104:980–1.
Orlowski O, Bullmann V, Vieth V, Filler T, Osada N, Van Aken H, Weber TP. Perivascular axillary brachial plexus block and patient positioning: the influence of a lateral, head-down position. Anaesthesia. 2006;61:528–34.
Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. ScientificWorldJournal. 2009;9:300–12.
Ongoiba N, Destrieux C, Koumare AK. Anatomical variations of the brachial plexus. Morphologie. 2002;86:31–4.
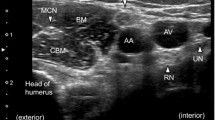
Helayel PE, Conceicao DB, Nascimento BS, Kohler A, Boos GL, Oliveira Filho GR. Learning curve for the ultrasound anatomy of the brachial plexus in the axillary region. Rev Bras Anestesiol. 2009;59:187–93.
Thompson GE, Rorie DK. Functional anatomy of the brachial plexus sheaths. Anesthesiology. 1983;59:117–22.
Partridge BL, Katz J, Benirschke K. Functional anatomy of the brachial plexus sheath: implications for anesthesia. Anesthesiology. 1987;66:743–7.
Retzl G, Kapral S, Greher M, Mauritz W. Ultrasonographic findings of the axillary part of the brachial plexus. Anesth Analg. 2001;92:1271–5.
Yamamoto K, Tsubokawa T, Ohmura S, Kobayashi T. The effects of arm position on central spread of local anesthetics and on quality of the block with axillary brachial plexus block. Reg Anesth Pain Med. 1999;24:36–42.
Vester-Andersen T, Broby-Johansen U, Bro-Rasmussen F. Perivascular axillary block VI: the distribution of gelatine solution injected into the axillary neurovascular sheath of cadavers. Acta Anaesthesiol Scand. 1986;30:18–22.
Acknowledgments
We thank Oguz Alp Turan for his assistance in language editing.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Salih Sevdi, M., Gunday, I., Arar, C. et al. Lateral Trendelenburg with the injected side down after the block improves the efficacy of the axillary approach to brachial plexus block. J Anesth 28, 538–543 (2014). https://doi.org/10.1007/s00540-013-1766-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1766-6