Abstract
Most patients suffering from trigeminal neuralgia (TN) benefit from medical therapy, for example carbamazepin, gabapentin, and pregabalin, individually or in combination. Nonetheless, some patients experience severe and intractable pain despite such medication, or the medication eliminates their pain but they experience intolerable side effects sufficient to warrant discontinuation. Intravenous magnesium and lidocaine have been used for management of intractable neuropathic pain. We treated nine patients with TN by using an intravenous infusion of a combination of 1.2 g magnesium and 100 mg lidocaine for 1 hour, once a week for 3 weeks. All patients experienced sound pain relief after the combined intravenous infusion therapy. Two patients experienced short and mild dizziness after the therapy, but no severe side effects were reported.
Similar content being viewed by others
Introduction
Trigeminal neuralgia (TN) is defined by the International Headache Society as “unilateral disorder characterized by brief electric shock-like pains, abrupt in onset and termination, and limited to the distribution of one or more divisions of the trigeminal nerve” [1]. Most patients benefit from medical therapy, for example carbamazepin, gabapentin, and pregabalin [2], initially, and their pain can be managed effectively for many years. Moreover, a combination of antiepileptic drugs can be an efficacious way of managing TN [2, 3]. Nonetheless, some patients experience severe and intractable pain, or the medications eliminate their pain but they experience intolerable side effects sufficient to warrant discontinuation. For such patients, a multimodal approach is necessary, for example a combination of non-antiepileptic drugs, Gamma Knife surgery, and microvascular decompression surgery [2, 4, 5].
Intravenous magnesium and lidocaine, individually or in combination, have been used for management of intractable pain [6–9]. We sometimes use this combination for management of TN when antiepileptic drugs fail. We report here nine patients with TN who were successfully treated by using a combination of intravenous magnesium and lidocaine after failure of antiepileptic drugs.
Case series
Retrospective analysis from January 2011 to June 2012 was performed for 9 patients suffering from TN who visited the pain centre of Aichi Medical University Hospital. All patients were referred from other hospitals to the pain centre because of intractable pain. Because there is no test for diagnosis of TN, correct diagnosis was based on the patient’s medical history, description of their face pain, and a thorough neurologic examination [1, 4]. Treatment protocols discussed in this report were based on institutional policy and clinical guidelines approved by the IRB of Aichi Medical University. Treatment guidelines for patients with intractable neuropathic pain are that patients who are referred to the pain centre will be treated with the recommended systemic analgesics, although intravenous magnesium and lidocaine are not indicated for patients with allergy to lidocaine. Information was extracted from medical records, after the patients provided oral consent for their information to be used for this case series report. All patients had an idiopathic form of TN. The pathophysiological characteristics and therapeutic management of the patients are described in Table 1. The patients had been taking antiepileptic drugs and non-antiepileptic drugs individually or in combination for a period of 6 months to 4 years without satisfactory pain relief, but with experience of a variety of side effects.
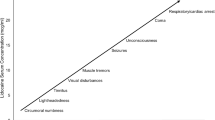
The treatment protocol was intravenous infusion of a combination of 1.2 g magnesium and 100 mg lidocaine for 1 hour, once a week for 3 weeks. A numerical rating scale (NRS) for pain on ranging from 0 to 10 (0 = no pain, 10 = worst pain imaginable) was evaluated and recorded on days 0, 7, 14, 21, and 28. Table 2 shows the individual changes of NRS. All patients experienced sound pain relief after the combined intravenous infusion therapy. Patients 5 and 7 experienced short and mild dizziness after the therapy, but no severe side effects were reported. Patients 2–5, 7, and 9 achieved secession of pharmacological treatment. Patients 1, 6, and 8 received the same pharmacological treatment. Patients 2 and 3 experienced recurrence of intractable TN 1 year later, and then received intravenous infusion of the same combination and experienced sound pain relief.
Discussion
Trigeminal neuralgia causes episodes of paroxysmal pain that are generally short-lasting (from less than 1 s up to 2 min) but intense in nature [2]. Between paroxysms the patient is usually free from painful symptoms, but continuous dull pain occasionally persists [2, 3]. Although carbamazepine is the initial drug of choice in the treatment of TN, and a combination of antiepileptic drugs is occasionally used, for some patients drug therapy results in severe side effects sufficient to warrant discontinuation, and the pain becomes more intractable as the disease progresses; this requires a multimodal approach [2, 3].
Lidocaine and magnesium are used safely in daily, clinical practice. Intravenous lidocaine, an amide local anaesthetic with class I antiarrhythmic action [10], has been used for several indications. Transmission of the peripheral nociceptive stimulus depends on the presence of voltage-gated sodium channels [11]. Lidocaine blocks impulses by inhibiting the sodium channels [12]. When used at sufficient concentration, local lidocaine causes complete nerve block. When administered intravenously, lidocaine has no apparent effects on the conduction of action potentials in normal Aβ, Aδ, or C afferent fibres [12]. In contrast, intravenous lidocaine has a substantial effect on damaged neural tissues. Moreover, administration of intravenous lidocaine blocks neuropathic pain via its action on sodium channels and blockade of central hyper-excitability [6, 11, 12].
Activation of N-methyl D-aspartate (NMDA) receptors is crucial to induction and continuation of central and peripheral nerve sensitization [8]. Magnesium is an antagonist of the NMDA receptors and exerts its effects by physically occluding the receptor pore and allosterically modulating the NR2B subunit [13]. In fact, several studies have shown significant benefits of magnesium in acute and chronic pain treatment [8, 9, 14].
Few reports have shown the usefulness of combined intravenous administration of lidocaine and magnesium in the management of intractable pain [9, 15]. A combination of intravenous lidocaine and magnesium provided sound pain relief for patients with intractable TN in this case series. Because lidocaine and magnesium work by different mechanisms, there is a possibility they could have synergistic rather than additional effects. Also, repeated administration of an intravenous infusion of a combination of magnesium and lidocaine might gradually have reduced the sensitization and thereby relieved the intractable TN.
A major limitation of this report is that it is a case series. Another major limitation is that we did not investigate the individual effect of magnesium and lidocaine on TN. Moreover, we need a randomized controlled trial to exclude the possibility of placebo effect. However, the incidence of TN is approximately 4 per 100,000 persons per year [2] and the incidence of intractable TN would be much lower than the figure, so it is very impractical for us to administer a randomized, placebo-controlled trial.
Because several researchers have used 20–70 mg/kg magnesium and/or 2–7 mg/kg lidocaine for pain management [8, 9, 14, 15], a lower and safer dose was chosen. We use a magnesium ampoule containing 1.2 g magnesium and a lidocaine ampoule containing 100 mg lidocaine in daily, clinical practice in Japan. We thus used an intravenous infusion of a combination of 1.2 g magnesium and 100 mg lidocaine in this case series.
In conclusion, we treated nine patients with intractable TN by using an intravenous infusion of a combination of 1.2 g magnesium and 100 mg lidocaine for 1 hour, once a week for 3 weeks. All patients experienced sound pain relief after the combined intravenous infusion therapy.
References
International Headache Society. The International classification of headache disorders: 2nd edn. Cephalalgia. 2004;24(Suppl 1):9–160.
Obermann M. Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord. 2010;3:107–15.
Prisco L, Ganau M, Bigotto F, Zornada F. Trigeminal neuralgia: successful antiepileptic drug combination therapy in three refractory cases. Drug Healthc Patient Saf. 2011;3:43–5.
Pollock BE. Surgical management of medically refractory trigeminal neuralgia. Curr Neurol Neurosci Rep. 2012;12:125–31.
Huang CF, Chuang JC, Tu HT, Chou MC. Microsurgical outcomes after failed repeated Gamma Knife surgery for refractory trigeminal neuralgia. J Neurosurg. 2006;105(Suppl):117–9.
Cahana A, Carota A, Montadon ML, Annoni JM. The long-term effect of repeated intravenous lidocaine on central pain and possible correlation in positron emission tomography measurements. Anesth Analg. 2004;98:1581–4.
Schwartzman RJ, Patel M, Grothusen JR, Alexander GM. Efficacy of 5-day continuous lidocaine infusion for the treatment of refractory complex regional pain syndrome. Pain Med. 2009;10:401–12.
Brill S, Sedgwick PM, Hamann W, Di Vadi PP. Efficacy of intravenous magnesium in neuropathic pain. Br J Anaesth. 2002;89:711–4.
Turan A, Memiş D, Karamanlioğlu B, Güler T, Pamukçu Z. Intravenous regional anesthesia using lidocaine and magnesium. Anesth Analg. 2005;100:1189–92.
Abdi S, Lee DH, Chung JM. The anti-allodynic effects of amitriptyline, gabapentin, and lidocaine in a rat model of neuropathic pain. Anesth Analg. 1998;87:1360–6.
Lauretti GR. Mechanisms of analgesia of intravenous lidocaine. Rev Bras Anestesiol. 2008;58:280–6.
McCleane G. Intravenous lidocaine: an outdated or underutilized treatment for pain? J Palliat Med. 2007;10:798–805.
Mony L, Kew JN, Gunthorpe MJ, Paoletti P. Allosteric modulators of NR2B-containing NMDA receptors: molecular mechanisms and therapeutic potential. Br J Pharmacol. 2009;157:1301–17.
Collins S, Zuurmond WW, de Lange JJ, van Hilten BJ, Perez RS. Intravenous magnesium for complex regional pain syndrome type 1 (CRPS 1) patients: a pilot study. Pain Med. 2009;10:930–40.
Noord Brandon Alan Van, Berger Jack, Motamed Arash. Opioid resistant pain successfully managed with magnesium, lidocaine and ketorolac in the Post-anesthesia Care Unit: a case series. J Anesthe Clinic Res. 2012;3:196.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Arai, YC.P., Hatakeyama, N., Nishihara, M. et al. Intravenous lidocaine and magnesium for management of intractable trigeminal neuralgia: a case series of nine patients. J Anesth 27, 960–962 (2013). https://doi.org/10.1007/s00540-013-1641-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1641-5