Abstract
Purpose
Intravenous cannulation is a painful and stressful procedure. The objective of this study was to compare the analgesic efficacy of the eutectic mixture of local anesthetics (EMLA®) with that of the Valsalva maneuver in adult patients during i.v. cannulation.
Methods
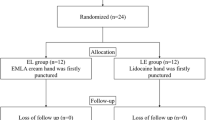
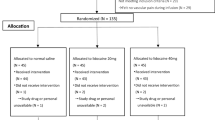
One hundred ninety-five patients were randomized prospectively to three groups. The dorsum of the nondominant hand was covered with a thick paste of 2.5 g of EMLA® cream in the EMLA® group (group E) and left for a minimum of 30 min before venipuncture. In the control group (group C), the same procedure was applied except that Vaseline® was used instead of the EMLA®. The Valsalva group (group V) were punctured during a Valsalva maneuver. The patients were placed in the supine position during venipuncture. The patients then scored the amount of pain on cannulation using an 11-point numerical rating scale (NRS; 0 = no pain, 10 = extreme pain).
Results
Thirteen patients were excluded from the analysis due to failed cannulation. There was no difference in the demographic profiles of the groups (p > 0.05). The success of VP was significantly higher in group V than in groups E and C (p < 0.001). The median pain score as assessed by the NRS after venipuncture in group C was 3 (range 0–9), whereas the median pain values in groups E and V were 2 (range 0–7) and 2 (range 1–8).
Conclusions
The Valsalva maneuver yields similar results to the EMLA® in terms of pain reduction during venipuncture.
Similar content being viewed by others
References
Speirs AF, Taylor KH, Joanes DN, Girdler NM. A randomised, double-blind, placebo controlled comparative study of topical skin analgesics and the anxiety and discomfort associated with venous cannulation. Br Dent J. 2001;190:444–9.
Agarwal A, Sinha PK, Tandon M, Dhiraaj S. Evaluating the efficacy of the Valsalva maneuver on venous cannulation pain: a prospective, randomized study. Anesth Analg. 2005;101:1230–2.
Selby IR, Bowles BJ. Analgesia for venous cannulation: a comparison of EMLA® (5 minutes application), lignocaine, ethylchloride, and nothing. J R Soc Med. 1995;88:264–7.
Romanò CL, Cecca E. A new method to reduce pin-prick pain of intra-muscular and subcutaneous injections. Minerva Anestesiol. 2005;71:609–15.
Usichenko TI, Pavlovic D, Foellner S, Wendt M. Reducing venipuncture pain by a cough trick: a randomized crossover volunteer study. Anesth Analg. 2004;98:343–5.
Basaranoglu G, Basaranoglu M, Erden V, Delatioglu H, Pekel AF, Saitoglu L. The effects of Valsalva manoeuvres on venepuncture pain. Eur J Anaesthesiol. 2006;23:591–3.
Tüfekci FG, Celebioğlu A, Küçükoğlu S. Turkish children loved distraction: using kaleidoscope to reduce perceived pain during venipuncture. J Clin Nurs. 2009;18:2180–6.
Zempsky WT, Bean-Lijewski J, Kauffman RE, Koh JL, Malviya SV, Rose JB, Richards PT, Gennevois DJ. Needle-free powder lidocaine delivery system provides rapid effective analgesia for venipuncture or cannulation pain in children: randomized, double-blind comparison of venipuncture and venous cannulation pain after fast-onset needle-free powder lidocaine or placebo treatment trial. Pediatrics. 2008;121:979–87.
Wagner KA, Gibbon KJ, Strom TL, Kurian JR, Trepanier LA. Adverse effects of EMLA (lidocaine/prilocaine) cream and efficacy for the placement of jugular catheters in hospitalized cats. J Feline Med Surg. 2006;8:141–4.
Jimenez N, Bradford H, Seidel KD, Sousa M, Lynn AM. A comparison of a needle-free injection system for local anesthesia versus EMLA for intravenous catheter insertion in the pediatric patient. Anesth Analg. 2006;102:411–4.
Massie BM, Amidon TM. Heart. In: Tierney LM, McPhee SJ, Papadakis MA, editors. Current medical diagnosis and treatment. McGraw-Hill, New York; 2002. p. 363–57.
Henry TR. Therapeutic mechanisms of vagus nerve stimulation. Neurology. 2002;24:3–4.
Liporace J, Hucko D, Morrow R, Barolat G, Nei M, Schnur J, Sperling M. Vagal nerve stimulation: adjustments to reduce painful side effects. Neurology. 2001;57:885–6.
Yamamoto LG, Boychuk RB. A blinded, randomized, paired, placebo-controlled trial of 20-minute EMLA cream to reduce the pain of peripheral i.v. cannulation in the ED. Am J Emerg Med. 1998;16:634–6.
Gupta D, Agarwal A, Dhiraaj S, Tandon M, Kumar M, Singh RS, Singh PK, Singh U. An evaluation of efficacy of balloon inflation on venous cannulation pain in children: a prospective, randomized, controlled study. Anesth Analg. 2006;102:1372–5.
Kirchner A, Birklein F, Stefan H, Handwerker HO. Left vagus nerve stimulation suppresses experimentally induced pain. Neurology. 2000;55:1167–71.
Ness TJ, Fillingim RB, Randich A, Backensto EM, Faught E. Low intensity vagal nerve stimulation lowers human thermal pain thresholds. Pain. 2000;86:81–5.
Suzuki T, Takeyama K, Hasegawa J, Nishiyama J, Takiguchi M. Valsalva maneuver prevents guide wire trouble associated with 22-gauge safe guide. Tokai J Exp Clin Med. 2001;26:113–8.
Kirchner A, Stefan H, Schmelz M, Haslbeck KM, Birklein F. Influence of vagus nerve stimulation on histamine-induced itching. Neurology. 2002;9:108–12.
Bennett T, Hosking DJ, Hampton JR. Baroreflex sensitivity and responses to the Valsalva manoeuvre in subjects with diabetes mellitus. J Neurol Neurosurg Psychiatry. 1976;39:178–83.
Lal MK, McClelland J, Phillips J, Taub NA, Beattie RM. Comparison of EMLA cream versus placebo in children receiving distraction therapy for venepuncture. Acta Paediatr. 2001;90:154–9.
Lewin MR, Stein J, Wang R, Lee MM, Kernberg M, Boukhman M, Hahn IH, Lewiss RE. Humming is as effective as Valsalva’s maneuver and Trendelenburg’s position for ultrasonographic visualization of the jugular venous system and common femoral veins. Ann Emerg Med. 2007;50:73–7.
Kwon TH, Kim YL, Cho DK. Ultrasound-guided cannulation of the femoral vein for acute haemodialysis access. Nephrol Dial Transplant. 1997;12:1009–12.
Mohammadi SS, Pajand AG, Shoeibi G. Efficacy of the valsalva maneuver on needle projection pain and hemodynamic responses during spinal puncture. Int J Med Sci. 2011;8:156–60.
Zhang R, Crandall CG, Levine BD. Cerebral hemodynamics during the Valsalva maneuver: insights from ganglionic blockade. Stroke. 2004;35:843–7.
Egekvist H, Bjerring P. Effect of EMLA cream on skin thickness and subcutaneous venous diameter. A randomized, placebo-controlled study in children. Acta Derm Venereol. 2000;80:340–3.
Fetzer SJ. Reducing venipuncture and intravenous insertion pain with eutectic mixture. Nurs Res. 2002;51:119–24.
Vaghadia H, al-Ahad OA, Nevin K. EMLA patch for intravenous cannulation in adult surgical outpatients. Can J Anaesth. 1997;44:798–802.
Singer AJ, Taira BR, Chisena EN, Gupta N, Chipley J. Warm lidocaine/tetracaine patch versus placebo before pediatric intravenous cannulation: a randomized controlled trial. J Ann Emerg Med. 2008;52:41–7.
Neri I, Savoia F, Guareschi E, Medri M, Patrizi A. Purpura after application of EMLA cream in two children. Pediatr Dermatol. 2005;22:566–8.
Acknowledgments
We wish to express our gratitude to Mr. Haluk Özdemir, Ismail Okan, and Bora Bostan for their critical reading of the manuscript. There was no financial support or sponsorship of this work, and the authors state that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Suren, M., Kaya, Z., Ozkan, F. et al. Comparison of the use of the Valsalva maneuver and the eutectic mixture of local anesthetics (EMLA®) to relieve venipuncture pain: a randomized controlled trial. J Anesth 27, 407–411 (2013). https://doi.org/10.1007/s00540-012-1540-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-012-1540-1