Abstract
Purpose
Preoperative administration of an N-methyl-d-aspartate (NMDA) receptor antagonist has been shown to attenuate tourniquet-induced blood pressure increase under general anesthesia, suggesting that the mechanism of this blood pressure increase includes NMDA receptor activation. The attenuation of this increase may be associated with the pain relief induced by NMDA receptor antagonism. We tested the hypothesis that magnesium sulfate, an NMDA receptor antagonist, attenuates tourniquet pain.
Methods
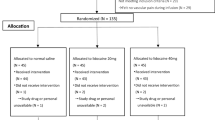
Twenty-four healthy volunteers were randomly assigned to four groups (n = 6 each): control (normal saline), M1 (magnesium, 1 g), M2 (magnesium, 2 g), and M4 (magnesium, 4 g). Normal saline or magnesium solution was given intravenously over a 15-min period, in a double-blind fashion, before tourniquet inflation, which was continued for 60 min or until the “pain score” (0 = no pain, 100 = highest tolerable pain) reached 100. Pain scores were recorded before and every 5 min during tourniquet inflation. If subjects reported a pain score of 100 before the end of the 60-min period, we adopted a pain score of 100 for the remaining period.
Results
The duration of tourniquet inflation in the M4 group was significantly longer than that in the control group (54.3 ± 8.3 vs. 42.9 ± 9.9 min, P = 0.03). Pain scores in the M4 group were significantly lower than those in the control group from 10 through 50 min after the start of tourniquet inflation. The area under the curve for pain scores in the M4 group was significantly smaller than the areas in the other groups.
Conclusion
Magnesium sulfate, 4 g, significantly attenuated tourniquet pain in healthy awake volunteers, suggesting that NMDA receptor activation is involved in tourniquet pain.

Similar content being viewed by others
References
Hagenouw RR, Bridenbaugh PO, van Egmond J, Stuebing R. Tourniquet pain: a volunteer study. Anesth Analg. 1986;65:1175–80.
Valli H, Rosenberg PH, Kytta J, Nurminen M. Arterial hypertension associated with the use of a tourniquet with either general or regional anaesthesia. Acta Anaesthesiol Scand. 1987;31:279–83.
McCartney CJ, Sinha A, Katz J. A qualitative systematic review of the role of N-methyl-d-aspartate receptor antagonists in preventive analgesia. Anesth Analg. 2004;98:1385–400.
Satsumae T, Yamaguchi H, Sakaguchi M, Yasunaga T, Yamashita S, Yamamoto S, Kida H. Preoperative small-dose ketamine prevented tourniquet-induced arterial pressure increase in orthopedic patients under general anesthesia. Anesth Analg. 2001;92:1286–9.
Yamashita S, Yamaguchi H, Hisajima Y, Ijima K, Saito K, Chiba A, Yasunaga T. Preoperative oral dextromethorphan attenuated tourniquet-induced arterial blood pressure and heart rate increases in knee cruciate ligament reconstruction patients under general anesthesia. Anesth Analg. 2004;98:994–8.
Lee DH, Jee DL, Kim SY, Kim JM, Lee HM. Magnesium sulphate attenuates tourniquet-induced hypertension and spinal c-fos mRNA expression: a comparison with ketamine. J Int Med Res. 2006;34:573–84.
Clements JA, Nimmo WS. Pharmacokinetics and analgesic effect of ketamine in man. Br J Anaesth. 1981;53:27–30.
Estebe JP, Le Naoures A, Chemaly L, Ecoffey C. Tourniquet pain in a volunteer study: effect of changes in cuff width and pressure. Anaesthesia. 2000;55:21–6.
Iseri LT, French JH. Magnesium: nature’s physiologic calcium blocker. Am Heart J. 1984;108:188–93.
Nowak L, Bregestovski P, Ascher P, Herbet A, Prochiantz A. Magnesium gates glutamate-activated channels in mouse central neurons. Nature. 1984;307:462–5.
Omote K, Kawamata M, Satoh O, Iwasaki H, Namiki A. Spinal antinociceptive action of an N-type voltage-dependent calcium channel blocker and the synergistic interaction with morphine. Anesthesiology. 1996;84:636–43.
Woolf CJ, Thompson SW. The induction and maintenance of central sensitization is dependent on N-methyl-d-aspartic acid receptor activation; implications for the treatment of post-injury pain hypersensitivity states. Pain. 1991;44:293–9.
Chabel C, Russell LC, Lee R. Tourniquet-induced limb ischemia: a neurophysiologic animal model. Anesthesiology. 1990;72:1038–44.
Maclver MB, Tanelian DL. Activation of C fibers by metabolic perturbations associated with tourniquet ischemia. Anesthesiology. 1992;76:617–23.
Coderre TJ, Katz J, Vaccarino AL, Melzack R. Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence. Pain. 1993;52:259–85.
Brill S, Sedqwick PM, Hammann W, Di Vadi PP. Efficacy of intravenous magnesium in neuropathic pain. Br J Anaesth. 2002;89:711–4.
Bondok RS, Abd El-Hady AM. Intra-articular magnesium is effective for postoperative analgesia in arthroscopic knee surgery. Br J Anaesth. 2006;97:389–92.
Elsharnouby NM, Eid HE. Abou Elezz NF, Moharram AN. Intraarticular injection of magnesium sulphate and/or bupivacaine for postoperative analgesia after arthroscopic knee surgery. Anesth Analg. 2008;106:1548–52.
Cairns BE, Svensson P, Wang K, Hupfeld S, Graven-Nielsen T, Sessle BJ, Berde CB, Arendt-Nielsen L. Activation of peripheral NMDA receptors contributes to human pain and rat afferent discharges evoked by injection of glutamate into the masseter muscle. J Neurophysiol. 2003;90:2098–105.
Petrenko AB, Yamakura T, Baba H, Shimoji K. The role of N-methyl-d-aspartate (NMDA) receptors in pain: a review. Anesth Analg. 2003;97:1108–16.
Fawcett WJ, Haxby EJ, Male DA. Magnesium: physiology and pharmacology. Br J Anaesth. 1999;83:302–20.
Xiao WH, Bennett GJ. Magnesium suppresses neuropathic pain responses in rats via a spinal site of action. Brain Res. 1994;666:168–72.
Fuchs-Buder T, Tramèr MR, Tassonyi E. Cerebrospinal fluid passage of intravenous magnesium sulphate in neurosurgical patients. J Neurosurg Anesthesiol. 1997;9:324–8.
Hwang JY, Na HS, Jeon YT, Ro YJ, Kim CS, Do SH. I.V. infusion of magnesium sulphate during spinal anaesthesia improves postoperative analgesia. Br J Anaesth. 2010;104:89–93.
Wadhwa A, Sengupta P, Durrani J, Akça O, Lenhardt R, Sessler DI, Doufas AG. Magnesium sulphate only slightly reduces the shivering threshold in humans. Br J Anaesth. 2005;94:756–62.
Ring C, Veldhuijzen van Zanten JJ, Kavussanu M. Effects of sex, phase of the menstrual cycle and gonadal hormones on pain in healthy humans. Biol Psychol. 2009;81:189–91.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Satsumae, T., Yamaguchi, H., Inomata, S. et al. Magnesium sulfate attenuates tourniquet pain in healthy volunteers. J Anesth 27, 231–235 (2013). https://doi.org/10.1007/s00540-012-1493-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-012-1493-4