Abstract
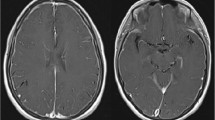
Posterior reversible encephalopathy syndrome (PRES) is a relatively new clinical entity characterized by reversible neurological symptoms with findings indicating leukoencephalopathy on imaging studies. Reports of PRES in the field of anesthesiology have been quite limited. A patient with therapeutic anticoagulant developed PRES immediately after emergence from anesthesia, in which her status was initially recognized as delayed recovery from anesthesia with transient hypertension because an emergent head computed tomography (CT) scan was almost normal. Subsequently, magnetic resonance imaging (MRI) was also performed according to a radiologist’s recommendation because the CT results showed areas of slightly low attenuation in the frontoparieto-occipital lobes bilaterally, suggesting PRES; otherwise, ischemic events. MRI showed subcortical increased T2 and fluid-attenuated inversion recovery (FLAIR) intensity in the occipitoparietal regions bilaterally with slight increase in the apparent diffusion coefficient signal on diffusion-weighted imaging, which confirmed a diagnosis of PRES. Gradually, the patient regained consciousness and became responsive with antihypertensive therapy. A prompt and accurate diagnosis of PRES is important to avoid irreversible brain damage, for example, intracranial hemorrhage, especially in a patient receiving anticoagulation therapy.

Similar content being viewed by others
References
Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, Lamy C, Mas JL, Caplan LR. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500.
Casey SO, Sampaio RC, Michel E, Truwit CL. Posterior reversible encephalopathy syndrome: utility of fluid-attenuated inversion recovery MR imaging in the detection of cortical and subcortical lesions. AJNR Am J Neuroradiol. 2000;21:1199–206.
McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, Teksam M. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007;189:904–12.
Kwon S, Jahoon K, Sangkwon L. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Pediatr Neurol. 2001;24:361–64.
Kim TK, Yoon JU, Park SC, Lee HJ, Kim WS, Yoon JY. Postoperative blindness associated with posterior reversible encephalopathy syndrome: a case report. J Anesth. 2010;24:783–5.
Schwartz RB, Jones KM, Kalina P, Bajakian RL, Mantello MT, Garada B, Holman BL. Hypertensive encephalopathy: findings on CT, MR imaging, and SPECT imaging in 14 cases. AJR Am J Roentgenol. 1992;159:379–83.
Rangi PS, Partridge WJ, Newlands ES, Waldman AD. Posterior reversible encephalopathy syndrome: a possible late interaction between cytotoxic agents and general anaesthesia. Neuroradiology. 2005;47:586–90.
Tominaga S, Strandgaard S, Uemura K, Ito K, Kutsuzawa T. Cerebrovascular CO2 reactivity in normotensive and hypertensive man. Stroke. 1976;7:507–10.
Joly V, Richebe P, Guignard B, Fletcher D, Maurette P, Sessler DI, Chauvin M. Remifentanil-induced postoperative hyperalgesia and its prevention with small-dose ketamine. Anesthesiology. 2005;103:147–55.
Långsjö JW, Kaisti KK, Aalto S, Hinkka S, Aantaa R, Oikonen V, Sipilä H, Kurki T, Silvanto M, Scheinin H. Effects of subanesthetic doses of ketamine on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology. 2003;99:614–23.
Hänel F, Werner C, von Knobelsdorff G, Schulte am Esch J. The effects of fentanyl and sufentanil on cerebral hemodynamics. J Neurosurg Anesthesiol. 1997;9:223–7.
Pirker A, Kramer L, Voller B, Loader B, Auff E, Prayer D. Type of edema in posterior reversible encephalopathy syndrome depends on serum albumin levels: an MR imaging study in 28 patients. AJNR Am J Neuroradiol. 2011;32:527–31.
Engelhardt T, Zaarour C, Naser B, Pehora C, de Ruiter J, Howard A, Crawford MW. Intraoperative low-dose ketamine does not prevent a remifentanil-induced increase in morphine requirement after pediatric scoliosis surgery. Anesth Analg. 2008;107:1170–5.
Stott VL, Hurrell MA, Anderson TJ. Reversible posterior leukoencephalopathy syndrome: a misnomer reviewed. Intern Med J. 2005;35:83–90.
Hefzy HM, Bartynski WS, Boardman JF, Lacomis D. Hemorrhage in posterior reversible encephalopathy syndrome: imaging and clinical features. AJNR Am J Neuroradiol. 2009;30:1371–9.
Mukherjee P, McKinstry RC. Reversible posterior leukoencephalopathy syndrome: evaluation with diffusion-tensor MR imaging. Radiology. 2001;219:756–65.
Acknowledgments
This case report does not include any conflict of interest. This case report was supported only by departmental sources.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Inoue, S., Kawaguchi, M. & Furuya, H. A case of posterior reversible encephalopathy syndrome after emergence from anesthesia. J Anesth 26, 111–114 (2012). https://doi.org/10.1007/s00540-011-1256-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1256-7