Abstract
Purpose
Levobupivacaine is metabolized hepatically. Whether postoperative epidural analgesia with levobupivacaine can lead to critical accumulation in patients undergoing major hepatic resection is unknown. Therefore, levobupivacaine concentrations were prospectively monitored in patients undergoing major liver resection and compared to patients undergoing rectal resection, who served as controls. Furthermore, we correlated levobupivacaine plasma concentrations with established liver function tests.
Methods
We analyzed plasma concentrations of levobupivacaine in 20 patients each scheduled for major liver or anterior rectal resection. All patients received general and epidural anesthesia (10 ml levobupivacaine 0.5% followed by 10 ml levobupivacaine 0.375% every 90 min) and postoperative continuous epidural analgesia (levobupivacaine 0.2%). Intraoperatively, and for 3 days postoperatively, levobupivacaine plasma concentrations were measured and correlated with bilirubin, fibrinogen, indocyanine green (ICG) clearance, and cholinesterase activity. Data (mean ± SD) were analyzed by two-way analysis of variance (ANOVA) with post hoc analysis or regression analysis (P < 0.05).
Results
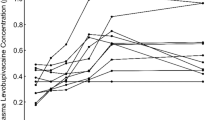
Intraoperatively and postoperatively, patients undergoing liver resection revealed significantly higher levobupivacaine concentrations (P= 0.0013 and P = 0.0016, respectively). Furthermore, significant differences were found for bilirubin (P = 0.0002), fibrinogen (P = 0.0002), and ICG (P < 0.0001). Highest levobupivacaine concentration correlated significantly with lowest ICG (P = 0.0004; R = 0.69), highest bilirubin (P = 0.0267; R = 0.49), lowest fibrinogen concentration (R = 0.32), but not with cholinesterase activity (R = 0.02).
Conclusion
Patients undergoing liver resection revealed significantly higher levobupivacaine concentrations compared to patients undergoing anterior rectal resection. However, although intraoperative levobupivacaine concentrations remained below 2.0 μg/ml, postoperative concentrations accumulated to a concentration above this threshold. This risk of levobupivacaine accumulation in patients with compromised liver function correlated best with ICG clearance.





Similar content being viewed by others
References
Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–41.
van Dam RM, Hendry PO, Coolsen MME, Bemelmans MHA, Lassen K, Revhaug A, Fearon KCH, Garden OJ, Dejong CHC. Initial experience with a multimodal enhanced recovery program in patients undergoing liver resection. Br J Surg. 2008;95:969–75.
Rodgers A, Walker N, Schug S, McKlee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomized trials. BMJ. 2000;321:1–12.
Foster RH, Markham A. Levobupivacaine—a review of its pharmacology and use as a local anaesthetic. Drugs. 2000;59:551–79.
Mather LE, McCall P, McNicol PL. Bupivacaine enantiomer pharmacokinetics after intercostals neural blockade in liver transplantation patients. Anesth Analg. 1995;80:328–35.
Meunier JF, Goujard E, Dubousset AM, Samii K, Mazoit JX. Pharmacokinetics of bupivacaine after continuous epidural infusion in infants with and without biliary atresia. Anesthesiology. 2001;95:87–95.
Jokinen MJ, Neuvonen PJ, Lindgren L, Höckerstedt K, Sjövall J, Breuer O, Askemark Y, Ahonen J, Olkkola KT. Pharmacokinetics of ropivacaine in patients with chronic end-stage liver disease. Anesthesiology. 2007;106:43–55.
Hofmann D, Thuemer O, Schelenz C, van Hout N, Sakka SG, et al. Increasing cardiac output by fluid loading: effects on indocyanine green plasma disappearance rate and splanchnic microcirculation. Acta Anaesthesiol Scand. 2005;49:1280–6.
Sakka SG, Reinhart K, Meier-Hellmann A. Comparison of invasive and noninvasive measurements of indocyanine green plasma disappearance rate in critically ill patients with mechanical ventilation and stable hemodynamics. Intensive Care Med. 2000;26:1553–6.
Clavien PA, Petrowsky H, DeOliviera ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. New Engl J Med. 2007;356:1545–59.
Oellerich M, Burdelski M, Lautz HU, Rodeck B, Duewel J, Schulz M, Schmidt FW, Brodehl J, Pichelmayr R. Assessment of pretransplant prognosis in patients with cirrhosis. Transplantation. 1991;51:801–6.
Groeben H, Schäfer B, Pavlakovic G, Silvanus MT, Peters J. Lung function under high thoracic segmental epidural anesthesia with ropivacaine or bupivacaine in patients with severe obstructive pulmonary disease undergoing breast surgery. Anesthesiology. 2002;96:536–41.
Matot I, Scheinin O, Eid A, Jurim O. Epidural anesthesia and analgesia in liver resection. Anesth Analg. 2002;95:1179–81.
Nishiyama T, Fujimoto T, Hanaoka K. A comparison of liver function after hepatectomy in cirrhotic patients between sevoflurane and isoflurane in anesthesia with nitrous oxide and epidural block. Anesth Analg. 2004;98:990–3.
Cywinski JB, Parker BM, Xu M, Irefin SA. A comparison of postoperative pain control in patients after right lobe donor hepatectomy and major hepatic resection for tumor. Anesth Analg. 2004;99:1747–52.
Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290:2455–63.
Bardsley H, Gristwood R, Watson N, Nimmo W. A comparison of the cardiovascular effects of levobupivacaine and rac-bupivacaine following intravenous administration to healthy volunteers. Br J Clin Pharmacol. 1998;46:245–9.
Knudsen K, Suurküla B, Blomberg S, Sjövall J, Edvardsson N, et al. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78:507–14.
Scott BD, Lee A, Fagan D, Bowler GMR, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg. 1989;69:563–9.
Santos AC, DeArmas PI. Systemic toxicity of levobupivacaine, bupivacaine, and ropivacaine during continuous intravenous infusion to non-pregnant and pregnant ewes. Anesthesiology. 2001;95:1256–64.
McLeod GA, Burke D. Levobupivacaine. Anaesthesia. 2001;56:331–41.
Kopacz DJ, Allen HW. Accidental intravenous levobupivacaine. Anesth Analg. 1999;89:1027–9.
Groban L, Deal DD, Vernon JC, James RL, Butterworth J. Cardiac resuscitation after incremental overdosage with lidocaine, bupivacaine, levobupivacaine, and ropivacaine in anesthetized dogs. Anesth Analg. 2001;92:37–43.
Hicks SD, Salcido DD, Logue ES, Suffoletto BP, Empey PE, Poloyac SM, Miller DR, Callaway CW, Menegazzi JJ. Lipid emulsion combined with epinephrine and vasopressin does not improve survival in a swine model of bupivacaine-induced cardiac arrest. Anesthesiology. 2009;111:138–46.
Scott DB. Evaluation of clinical tolerance of local anaesthetic agents. Br J Anaesth. 1975;47:328–31.
Gamsjaeger T, Brenner L, Sitzwohl C, Weinstabl C. Half-lives of albumin and cholinesterase in critically ill patients. Clin Chem Lab Med. 2008;46:1140–2.
Ostergaard D, Viby-Mogensen, Hanel HK, Skovgaard LT, et al. Half-life of plasma cholinesterase. Acta Anaesthesiol Scand. 1988;32:266–9.
Kimura S, Yoshioka T, Shibuya M, Sakano T, Tanaka R, Matsuyama S. Indocyanine green elimination rate detects hepatocellular dysfunction early in septic shock and correlates with survival. Crit Care Med. 2001;29:1159–63.
Kredel M, Muellenbach RM, Brock RW, Wilckens HH, Brederlau J, Roewer N, Wunder C. Liver dysfunction after lung recruitment manoeuvres during pressure-controlled ventilation in experimental acute respiratory distress. Crit Care. 2007;11:R13.
Krenn CG, Krafft P, Schaefer B, Pokorny H, Schneider B, Pinsky MR, Steltzer H. Effects of positive end-expiratory pressure on hemodynamics and indocyanine green kinetics in patients after orthotopic liver transplantation. Crit Care Med. 2000;28:1760–5.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lauprecht, AE., Wenger, F.A., El Fadil, O. et al. Levobupivacaine plasma concentrations following major liver resection. J Anesth 25, 369–375 (2011). https://doi.org/10.1007/s00540-011-1107-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1107-6