Abstract
Purpose
The purpose of this study was to compare the effects of norepinephrine (NE) and vasopressin on systemic hemodynamics, renal and mesenteric artery blood flow, inflammatory response and inducible nitric oxide synthase (iNOS) activity during endotoxin shock in streptozotocin-induced diabetic rats.
Methods
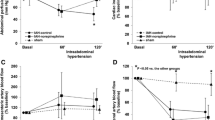
The study was designed to include three sets of experiments: (1) measurement of changes in systemic hemodynamics and mesenteric and renal artery blood flow; (2) measurement of biochemical variables; and (3) measurement of iNOS activity in the mesenteric artery. Systemic hemodynamics, regional artery blood flow changes and biochemical variables were assessed before treatment and 1, 2 and 3 h after treatment.
Results
Vasopressin, but not NE, prevented the decreases in aortic blood flow, but did not restore mesenteric artery blood flow. In addition, vasopressin partially restored renal artery blood flow in diabetic rats. Plasma nitrite levels and iNOS activity in the mesenteric artery were elevated after intravenous LPS in diabetic rats. Endotoxin-induced decreases in mesenteric arterial blood flow were partially restored by vasopressin with nonselective NOS inhibitor, N G-nitro-l-arginine methyl ester (l-NAME), in diabetic rats. Moreover, l-NAME prevented increases in plasma nitrite levels and iNOS activity in the mesenteric artery. In contrast, endotoxin-induced decreases in renal arterial blood flow were partially restored by vasopressin with l-NAME, but not by NE in diabetic rats.
Conclusions
Nitric oxide may be one possible contributor to reduced sensitivity of the mesenteric and renal arteries to vasopressin during septic shock in streptozotocin-induced diabetic rats.






Similar content being viewed by others
References
Ghosh S, Latimer RD, Gray BM, Harwood RJ, Oduro A. Endotoxin-induced organ injury. Crit Care Med. 1993;21:S19–24.
Parratt JR. Myocardial and circulatory effects of E. coli endotoxin: modification of responses to catecholamines. Br J Pharmacol. 1973;47:12–8.
Sprung CL, Bernard GR, Dellinger RP. Guidelines for the management of severe sepsis and septic shock. Int Care Med. 2001;27(Suppl):S128–34.
Task Force of the American Collage of Critical Care Medicine, Society of Critical Care Medicine. Practice parameters for hemodynamic support of sepsis in adult patients in sepsis. Crit Care Med 1999;27:639–660.
Meier-Hellman A, Reinhart K. Effects of catecholamines on regional perfusion and oxygenation in critically ill patients. Acta Anaesthesiol Scand. 1995;39(Suppl 107):239–48.
Tsuneyoshi I, Yamada H, Kakihana Y, Nakamura M, Nakano Y, Boyle WA III. Hemodynamic and metabolic effects of low-dose vasopressin infusions in vasodilatory septic shock. Crit Care Med. 2001;29:487–93.
Guzman JA, Rosado AE, Kruse JA. Vasopressin vs norepinephrine in endotoxic shock: systemic, renal, and splanchnic hemodynamic and oxygen transport effects. J Appl Physiol. 2003;95:803–9.
Klinzing S, Simon M, Reinhart K, Bredle DL, Meier-Hellmann A. High-dose vasopressin is not superior to norepinephrine in septic shock. Crit Care Med. 2003;31:2646–50.
Tsuneyoshi I, Kanmura Y, Yoshimura N. Nitric oxide as a mediator of reduced arterial responsiveness in septic patients. Crit Care Med. 1996;24:1083–6.
Patel S, Gaspers LD, Boucherie S, Memin E, Stellato KA, Guillon G, Combettes L, Thomas AP. Inducible nitric-oxide synthase attenuates vasopressin-dependent Ca2+ signaling in rat hepatocytes. J Biol Chem. 2002;277:33776–82.
Gando S, Hattori Y, Akaishi Y, Nishihira J, Kanno M. Impaired contractile response to beta adrenoceptor stimulation in diabetic rat hearts: alterations in beta adrenoceptors-G protein-adenylate cyclase system and phospholamban phosphorylation. J Pharmacol Exp Ther. 1997;282:475–84.
Cheng X, Cheng XS, Kuo KH, Pang CCY. Inhibition of iNOS augments cardiovascular action of noradrenaline in streptozotocin-induced diabetes. Cardiovasc Res. 2004;64:298–307.
Kadoi Y, Hinohara H, Kunimoto F, Saito S. Effects of the cannabinoid antagonist AM 281 on systemic hemodynamics and mortality rate in streptozotocin-induced diabetic rats with endotoxic shock: comparison between non-diabetic and diabetic rats. Acta Anaesthesiol Scand. 2008;52:664–72.
Kadoi Y, Goto F. Effects of selective iNOS inhibition on systemic hemodynamics and mortality rate on endotoxic shock in streptozotocin-induced diabetic rats. Shock. 2007;28:602–10.
Kadoi Y, Hinohara H, Kunimoto F, Kuwano H, Saito S, Goto G. Effects of AM 281, a cannabinoid antagonist, on systemic hemodynamics, internal carotid artery blood flow and mortality rate in septic shock in rats. Br J Anesth. 2005;94:563–8.
Kadoi Y, Saito S. An alteration in the gamma-aminobutyric acid receptor system in experimentally induced septic shock in rats. Crit Care Med. 1996;24:298–305.
Kadoi Y, Saito S, Kunimoto F, Imai T, Fujita T. Impairment of the brain beta-adrenergic system during experimental endotoxemia. J Surg Res. 1996;61:496–502.
Kadoi Y, Goto F. Selective inducible nitric oxide inhibition can restore hemodynamics, but does not improve neurological dysfunction in experimentally induced septic shock in rats. Anesth Analg. 2004;99:212–20.
Kadoi Y, Saito S, Kawahara F, Nishihara F, Goto F. G-protein coupled receptor kinase 2 is altered during septic shock in rats. J Surg Res. 2002;108:69–76.
Kadoi Y, Goto F. Comparative effects of vasopressin versus norepinephrine on systemic hemodynamics, renal and mesenteric blood flow during septic shock in rats. Sosei (Jpn J Reanimat) 2006;25:17–22 (in Japanese with English abstract).
Esposito K, Nappo F, Marfella R, Giugliano F, Giotola M, Quagliaro L, Geriello A, Giugliano D. Inflammatory cytokine concentrations are actually increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106:2067–72.
Bardell AL, Macleod KM. Evidence for inducible nitric-oxide synthase expression and activity in vascular smooth muscle of streptozotocin-diabetic rats. J Pharmacol Exp Ther. 2001;296:252–9.
Kirkeboen KA, Strand OA. The role of nitric oxide in sepsis—an overview. Acta Anaesthesiol Scand. 1999;43:275–88.
Treggiari MM, Romand JA, Burgener D, Suter PM, Aneman A. Effect of increasing norepinephrine dosage on regional blood flow in a porcine model of endotoxin shock. Crit Care Med. 2002;30:1334–9.
De Backer D, Creteur J, Silva E, Vincent JL. Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: which is best? Crit Care Med. 2003;31:1659–67.
Sautner T, Wessely C, Riegler M, Sedivy R, Gotzinger P, Losert U, Roth E, Jakesz R, Függer R. Early effects of catecholamine therapy on mucosal integrity, intestinal blood flow, and oxygen metabolism in porcine endotoxin shock. Ann Surg. 1998;228:239–48.
Meier-Hellmann A, Specht M, Hannemann L, Hassel H, Bredle DL, Reinhart K. Splanchnic blood flow is greater in septic shock treated with norepinephrine than in severe sepsis. Intensive Care Med. 1996;22:1354–9.
Di Giantomaso D, May CN, Bellomo R. Norepinephrine and vital organ blood flow during experimental hyperdynamic sepsis. Intensive Care Med. 2003;29:1774–81.
Revelly JP, Liaudet L, Frascarolo P, Joseph JM, Martinet O, Markert M. Effects of norepinephrine on the distribution of intestinal blood flow and tissue adenosine triphosphate content in endotoxic shock. Crit Care Med. 2000;28:2500–6.
Martikainen TJ, Tenhunen JJ, Uusaro A, Ruokonen E. The effects of vasopressin on systemic and splanchnic hemodynamics and metabolism in endotoxin shock. Anesth Analg. 2003;97:1756–63.
Malay MB, Ashton JL, Dahl K, Savage EB, Burchell SA, Ashton RC, Sciacca RR, Oliver JA, Landry DW. Heterogeneity of the vasoconstrictor effect of vasopressin in septic shock. Crit Care Med. 2004;32:1327–31.
García-Villalón AL, Garcia JL, Fernández N, Monge L, Gómez B, Diéguez G. Regional differences in the arterial response to vasopressin: role of endothelial nitric oxide. Br J Pharmacol. 1996;118:1848–54.
Okamura T, Ayajiki K, Fujioka H, Toda N. Mechanisms underlying arginine vasopressin-induced relaxation in monkey isolated coronary arteries. J Hypertens. 1999;17:673–8.
Ichinose F, Buys ES, Neilan TG, Furutani EM, Morgan JG, Jassal DS, Graveline AR, Searles RJ, Lim CC, Kaneki M, Picard MH, Scherrer-Crosbie M, Janssens S, Liao R, Bloch KD. Cardiomyocyte-specific overexpression of nitric oxide synthase 3 prevents myocardial dysfunction in murine models of septic shock. Circ Res. 2007;100:130–9.
Che YH, Tamatani M, Yamashita T, Gomi F, Ogawa S, Tohyama M. Changes in mRNA of protein inhibitor of neuronal nitric oxide synthase following facial nerve transection. J Chem Neuroanat. 2000;17:199–206.
Schwartz D, Brasowski E, Raskin Y, Schwartz IF, Wolman Y, Blum M, Blantz RC, Iaina A. The outcome of non-selective vs selective nitric oxide synthase inhibition in lipopolysaccharide treated rats. J Nephrol. 2001;14:110–4.
Liaudet L, Rosselet A, Schaller MD, Markert M, Perret C, Feihl F. Nonselective versus selective inhibition of inducible nitric oxide synthase in experimental endotoxic shock. J Infect Dis. 1998;177:127–32.
Aranow JS, Zhuang J, Wang H, Larkin V, Smith M, Fink MP. A selective inhibitor of inducible in nitric oxide synthase prolongs survival in a rat model of bacterial peritonitis: comparison with two nonselective strategies. Shock. 1996;5:116–21.
Smith JM, Paulson DJ, Romano FD. Inhibition of nitric oxide synthase by l-NAME improves ventricular performance in streptozotocin-diabetic rats. J Mol Cell Cardiol. 1997;29:2393–402.
Connelly L, Madhani M, Hobbs AJ. Resistance to endotoxic shock in endothelial nitric-oxide synthase (eNOS) knock-out mice: a pro-inflammatory role for eNOS-derived no in vivo. J Biol Chem. 2005;280:10040–6.
Acknowledgments
The authors wish to thank Forte (Tokyo, Japan) for assistance with preparing the manuscript in English. This study was supported by grants (to Dr. Kadoi, #21591998 and to Dr. Hinohara, #19592087) from the Japanese Ministry of Science, Education and Culture.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hinohara, H., Kadoi, Y., Tokue, A. et al. Comparison of the effects of vasopressin and norepinephrine on organ perfusion during septic shock in streptozotocin-induced diabetic rats. J Anesth 24, 553–563 (2010). https://doi.org/10.1007/s00540-010-0934-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-010-0934-1