Abstract
Background
Artificial intelligence (AI) performed variously among test sets with different diversity due to sample selection bias, which can be stumbling block for AI applications. We previously tested AI named ENDOANGEL, diagnosing early gastric cancer (EGC) on single-center videos in man–machine competition. We aimed to re-test ENDOANGEL on multi-center videos to explore challenges applying AI in multiple centers, then upgrade ENDOANGEL and explore solutions to the challenge.
Methods
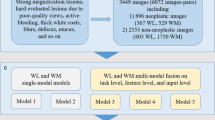
ENDOANGEL was re-tested on multi-center videos retrospectively collected from 12 institutions and compared with performance in previously reported single-center videos. We then upgraded ENDOANGEL to ENDOANGEL-2022 with more training samples and novel algorithms and conducted competition between ENDOANGEL-2022 and endoscopists. ENDOANGEL-2022 was then tested on single-center videos and compared with performance in multi-center videos; the two AI systems were also compared with each other and endoscopists.
Results
Forty-six EGCs and 54 non-cancers were included in multi-center video cohort. On diagnosing EGCs, compared with single-center videos, ENDOANGEL showed stable sensitivity (97.83% vs. 100.00%) while sharply decreased specificity (61.11% vs. 82.54%); ENDOANGEL-2022 showed similar tendency while achieving significantly higher specificity (79.63%, p < 0.01) making fewer mistakes on typical lesions than ENDOANGEL. On detecting gastric neoplasms, both AI showed stable sensitivity while sharply decreased specificity. Nevertheless, both AI outperformed endoscopists in the two competitions.
Conclusions
Great increase of false positives is a prominent challenge for applying EGC diagnostic AI in multiple centers due to high heterogeneity of negative cases. Optimizing AI by adding samples and using novel algorithms is promising to overcome this challenge.




Similar content being viewed by others
Abbreviations
- AI:
-
Artificial intelligence
- GC:
-
Gastric cancer
- EGC:
-
Early gastric cancer
- LNM:
-
Lymph node metastasis
- SM:
-
Submucosal
- CNN:
-
Conventional neural network
- WLE:
-
White light endoscopy
- M-NBI:
-
Magnifying narrow-band imaging
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
References
Smyth EC, Nilsson M, Grabsch HI, et al. Gastric cancer. Lancet. 2020;396:635–48.
Katai H, Ishikawa T, Akazawa K, et al. Five-year survival analysis of surgically resected gastric cancer cases in Japan: a retrospective analysis of more than 100,000 patients from the nationwide registry of the Japanese gastric cancer association (2001–2007). Gastric Cancer. 2018;21:144–54.
Banks M, Graham D, Jansen M, et al. British society of gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;68:1545–75.
Bi WL, Hosny A, Schabath MB, et al. Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J Clin. 2019;69:127–57.
Niazi MKK, Parwani AV, Gurcan MN. Digital pathology and artificial intelligence. Lancet Oncol. 2019;20:e253–61.
Yu TF, He W, Gan CG, et al. Deep learning applied to two-dimensional color Doppler flow imaging ultrasound images significantly improves diagnostic performance in the classification of breast masses: a multicenter study. Chin Med J (Engl). 2021;134:415–24.
Haggenmuller S, Maron RC, Hekler A, et al. Skin cancer classification via convolutional neural networks: systematic review of studies involving human experts. Eur J Cancer. 2021;156:202–16.
Hirasawa T, Aoyama K, Tanimoto T, et al. Application of artificial intelligence using a convolutional neural network for detecting gastric cancer in endoscopic images. Gastric Cancer. 2018;21:653–60.
Niikura R, Aoki T, Shichijo S, et al. Artificial intelligence versus expert endoscopists for diagnosis of gastric cancer in patients who have undergone upper gastrointestinal endoscopy. Endoscopy. 2022;54:780–4.
Johnson KB, Wei WQ, Weeraratne D, et al. Precision medicine, AI, and the future of personalized health care. Cts-Clin Transl Sci. 2021;14:86–93.
Chen M, Decary M. Artificial intelligence in healthcare: an essential guide for health leaders. Healthc Manage Forum. 2020;33:10–8.
Wu L, Wang J, He X, et al. Deep learning system compared with expert endoscopists in predicting early gastric cancer and its invasion depth and differentiation status (with videos). Gastrointest Endosc. 2022;95(92–104): e3.
Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182–8.
Skrede OJ, De Raedt S, Kleppe A, et al. Deep learning for prediction of colorectal cancer outcome: a discovery and validation study. Lancet. 2020;395:350–60.
van Engelen JE, Hoos HH. A survey on semi-supervised learning. Mach Learn. 2020;109:373–440.
Maron RC, Haggenmuller S, von Kalle C, et al. Robustness of convolutional neural networks in recognition of pigmented skin lesions. Eur J Cancer. 2021;145:81–91.
Sharmat P, Hassan C. Artificial intelligence and deep learning for upper gastrointestinal neoplasia. Gastroenterology. 2022;162:1056–66.
Benkarim O, Paquola C, Park BY, et al. Population heterogeneity in clinical cohorts affects the predictive accuracy of brain imaging. PLoS Biol. 2022;20: e3001627.
Norgeot B, Quer G, Beaulieu-Jones BK, et al. Minimum information about clinical artificial intelligence modeling: the MI-CLAIM checklist. Nat Med. 2020;26:1320–4.
Ryan M, Stahl BC. Artificial intelligence ethics guidelines for developers and users: clarifying their content and normative implications. J Inf Commun Ethics Soc. 2021;19:61–86.
de Hond AAH, Leeuwenberg AM, Hooft L, et al. Guidelines and quality criteria for artificial intelligence-based prediction models in healthcare: a scoping review. Npj Digital Med. 2022;5:2.
Luo H, Xu G, Li C, et al. Real-time artificial intelligence for detection of upper gastrointestinal cancer by endoscopy: a multicentre, case-control, diagnostic study. Lancet Oncol. 2019;20:1645–54.
Wu L, Zhou W, Wan X, et al. A deep neural network improves endoscopic detection of early gastric cancer without blind spots. Endoscopy. 2019;51:522–31.
Yu G, Sun K, Xu C, et al. Accurate recognition of colorectal cancer with semi-supervised deep learning on pathological images. Nat Commun. 2021;12:6311.
Wu L, Xu M, Jiang X, et al. Real-time artificial intelligence for detecting focal lesions and diagnosing neoplasms of the stomach by white-light endoscopy (with videos). Gastrointest Endosc. 2022;95:269-80.e6.
Chiu PWY, Uedo N, Singh R, et al. An Asian consensus on standards of diagnostic upper endoscopy for neoplasia. Gut. 2019;68:186–97.
Nakanishi H, Doyama H, Ishikawa H, et al. Evaluation of an e-learning system for diagnosis of gastric lesions using magnifying narrow-band imaging: a multicenter randomized controlled study. Endoscopy. 2017;49:957–67.
Tang D, Ni M, Zheng C, et al. A deep learning-based model improves diagnosis of early gastric cancer under narrow band imaging endoscopy. Surg Endosc. 2022;36:7800–10.
Yuan XL, Liu W, Liu Y, et al. Artificial intelligence for diagnosing microvessels of precancerous lesions and superficial esophageal squamous cell carcinomas: a multicenter study. Surg Endosc. 2022;36:8651–62.
Acknowledgements
College-enterprise Deepening Reform Project of Wuhan University (to Honggang Yu). Artificial Intelligence Application Demonstration Scenario Project Wuhan (grant no.2022YYCJ01) (to Honggang Yu). National Natural Science Foundation of China-Youth Science Fund (grant no.82202257) (To Lianlian Wu). Special projects for knowledge innovation of Wuhan (grant no.2022020801020482) (To Lianlian Wu).
Funding
College-enterprise Deepening Reform Project of Wuhan Universit, Artificial Intelligence Application Demonstration Scenario Project Wuhan, 2022YYCJ01, Hongang Yu, National Natural Science Foundation of China-Youth Science Fund, 82202257, Lianlian Wu, Special projects for knowledge innovation of Wuhan, 2022020801020482, Lianlian Wu.
Author information
Authors and Affiliations
Contributions
HGY and LLW made a big picture of the work and supervised the overall study. ZHD designed and did the experiments. ZHD and XT developed the system. CYH, ZFZ, XLM, YWA, BPZ, ML, HX, ZYJ, YWS, XLL, ZHL, JZC, YS, and GWL were involved in the data collection. ZHD and XT wrote the original draft. ZHD, HLD, CJL, LH, and XT analyzed the data. HGY and LLW revised the manuscript. JXW, XQZ, YXL, JL, and YJZ were involved in the format check and reviewing. HGY was responsible for the overall content as guarantor. All authors approved the final version of the report.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Video 1. Use of ENDOANGEL-2022 on detecting gastric neoplasm and diagnosing early gastric cancer. A pathologically confirmed high-grade intraepithelial neoplasia is shown. ENDOANGEL-2022 successfully detected it as a gastric neoplasm under white-light endoscopy, diagnosed it as an EGC under magnifying narrow-band imaging. Supplementary file1 (MP4 12917 KB)
Video 2. Use of ENDOANGEL-2022 for detecting and diagnosing chronic inflammation. A pathologically confirmed chronic inflammation lesion is shown. ENDOANGEL-2022 successfully detected the lesion as non-neoplasm under white-light endoscopy and diagnosed it as noncancerous under magnifying narrow-band imaging. Supplementary file2 (MP4 59998 KB)
535_2023_2025_MOESM4_ESM.tif
Figure S1. Flow chart of the eligibility of the videos and lesions in the present competition. Supplementary file4 (TIF 8192 KB)
535_2023_2025_MOESM5_ESM.tif
Figure S2. Flow chart of the eligibility of the endoscopists in the present competition. Supplementary file5 (TIF 9383 KB)
535_2023_2025_MOESM6_ESM.tif
Figure S3. Heat maps and bar graph showing answers of two AI systems and the error rate of endoscopists on each case on detecting gastric neoplasms. A. Single-center videos. B. Multi-center videos. Each column represents a different case. The 1st and 2nd rows showed the results of the two AI systems. The 3rd row showed the gold standard, neoplasms were shown in red color, and non-neoplasms were shown in blue color. Supplementary file6 (TIF 13191 KB)
535_2023_2025_MOESM7_ESM.tif
Figure S4. Heat maps and bar graph showing answers of two AI systems and the error rate of endoscopists in each case on diagnosing early gastric cancer. A. Single-center videos. B. Multi-center videos. Each column represents a different case. The 1st and 2nd rows showed the results of the two AI systems. The 3rd row showed the gold standard, early gastric cancers was shown in red color, and non-cancers were shown in blue color. Supplementary file7 (TIF 11925 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, Z., Tao, X., Du, H. et al. Exploring the challenge of early gastric cancer diagnostic AI system face in multiple centers and its potential solutions. J Gastroenterol 58, 978–989 (2023). https://doi.org/10.1007/s00535-023-02025-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-023-02025-3