Abstract
Background
Recent studies highlighted the clinicopathological heterogeneity of non-ampullary duodenal adenomas and adenocarcinomas, but the detailed process of the malignant transformation remains unclear.
Methods
We analyzed 144 adenomas and 54 adenocarcinomas of the non-ampullary duodenum for immunohistochemical phenotypes, genetic alterations, and mismatch repair (MMR) status to probe their histogenetic relationship.
Results
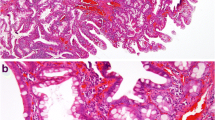
The median ages of patients with adenoma and adenocarcinoma were the same (66 years). Adenomas were histologically classified as intestinal-type adenoma (n = 124), pyloric gland adenoma (PGA, n = 10), gastric-type adenoma, not otherwise specified (n = 9), and foveolar-type adenoma (n = 1). Protein-truncating APC mutations were highly frequent in adenomas (85%), with the highest prevalence in intestinal-type adenomas (89%), but rare in adenocarcinomas (9%; P = 2.1 × 10–23). Close associations between phenotypic marker expression and genetic alterations were observed in adenomas, but not in adenocarcinomas, excluding the common association between GNAS mutations and MUC5AC expression. MMR deficiency was more frequent in adenocarcinomas (20%) than in adenomas (1%; P = 2.6 × 10–6). One MMR-deficient adenoma and three MMR-deficient adenocarcinomas occurred in patients with Lynch syndrome. Additionally, three other patients with an MMR-deficient adenocarcinoma fulfilled the revised Bethesda criteria.
Conclusion
The discrepant APC mutation frequency between adenomas and adenocarcinomas suggests that APC-mutated adenomas, which constitute the large majority of non-ampullary duodenal adenomas, are less prone to malignant transformation. Non-ampullary duodenal adenocarcinomas frequently exhibit MMR deficiency and should be subject to MMR testing to determine appropriate clinical management, including the identification of patients with Lynch syndrome.



Similar content being viewed by others
References
Lepage C, Bouvier A-M, Manfredi S, et al. Incidence and management of primary malignant small bowel cancers: a well-defined French population study. Am J Gastroenterol. 2006;101:2826–32.
Bilimoria KY, Bentrem DJ, Wayne JD, et al. Small bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg. 2009;249:63–71.
Lu Y, Fröbom R, Lagergren J. Incidence patterns of small bowel cancer in a population-based study in Sweden: increase in duodenal adenocarcinoma. Cancer Epidemiol. 2012;36:e158–63.
Ushiku T, Arnason T, Fukayama M, et al. Extra-ampullary duodenal adenocarcinoma. Am J Surg Pathol. 2014;38:1484–93.
Xue Y, Vanoli A, Balci S, et al. Non-ampullary-duodenal carcinomas: clinicopathologic analysis of 47 cases and comparison with ampullary and pancreatic adenocarcinomas. Mod Pathol. 2017;30:255–66.
Laforest A, Aparicio T, Zaanan A, et al. ERBB2 gene as a potential therapeutic target in small bowel adenocarcinoma. Eur J Cancer. 2014;50:1740–6.
Yuan W, Zhang Z, Dai B, et al. Whole-exome sequencing of duodenal adenocarcinoma identifies recurrent Wnt/β-catenin signaling pathway mutations: exome sequencing of duodenal cancer. Cancer. 2016;122:1689–96.
Yachida S, Wood LD, Suzuki M, et al. Genomic sequencing identifies ELF3 as adriver of ampullary carcinoma. Cancer Cell. 2016;29:229–40.
Network CGA. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Spigelman AD, Talbot IC, Penna C, et al. Evidence for adenoma-carcinoma sequence in the duodenum of patients with familial adenomatous polyposis. The Leeds Castle Polyposis Group (Upper Gastrointestinal Committee). J Clin Pathol. 1994;47:709–10.
Spigelman AD, Talbot IC, Williams CB, et al. Upper gastrointestinal cancer in patients with familial adenomatous polyposis. The Lancet. 1989;334:783–5.
Powell SM, Petersen GM, Krush AJ, et al. Molecular diagnosis of familial adenomatous polyposis. N Engl J Med. 1993;329:1982–7.
Offerhaus GJA, Giardiello FM, Krush AJ, et al. The risk of upper gastrointestinal cancer in familial adenomatous polyposis. Gastroenterology. 1992;102:1980–2.
Groves C, Saunders BP, Spigelman AD, et al. Duodenal cancer in patients with familial adenomatous polyposis (FAP): results of a 10 year prospective study. Gut. 2002;50:636–41.
Bülow S, Björk J, Christensen IJ, et al. Duodenal adenomatosis in familial adenomatous polyposis. Gut. 2004;53:381–6.
Latchford AR, Neale KF, Spigelman AD, et al. Features of duodenal cancer in patients with familial adenomatous polyposis. Clin Gastroenterol Hepatol. 2009;7:659–63.
Perzin KH, Bridge MF. Adenomas of the small intestine: a clinicopathologic review of 51 cases and a study of their relationship to carcinoma. Cancer. 1981;48:799–819.
Wagner PL, Chen Y-T, Yantiss RK. Immunohistochemical and molecular features of sporadic and FAP-associated duodenal aenomas of the ampullary and nonampullary mucosa. Am J Surg Pathol. 2008;32:1388–95.
Kushima R, Rüthlein HJ, Stolte M, et al. ’Pyloric gland-type adenoma’ arising in heterotopic gastric mucosa of the duodenum, with dysplastic progression of the gastric type. Virchows Arch. 1999;435:452–7.
Kushima R, Stolte M, Dirks K, et al. Gastric-type adenocarcinoma of the duodenal second portion histogenetically associated with hyperplasia and gastric-foveolar metaplasia of Brunner’s glands. Virchows Arch. 2002;440:655–9.
Sakurai T, Sakashita H, Honjo G, et al. Gastric foveolar metaplasia with dysplastic changes in Brunner gland hyperplasia: possible precursor lesions for Brunner gland adenocarcinoma. Am J Surg Pathol. 2005;29:1442–8.
Matsubara A, Ogawa R, Suzuki H, et al. Activating GNAS and KRAS mutations in gastric foveolar metaplasia, gastric heterotopia, and adenocarcinoma of the duodenum. Br J Cancer. 2015;112:1398–404.
Sekine S, Shia J. Non-ampullary adenoma. In: WHO Classification of Tumours Editorial Board, editor. Digestive system tumours. 5th ed. Lyon: IARC; 2019. p. 118–20.
Inoue T, Uedo N, Yamashina T, et al. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm: delayed perforation after duodenal ER. Dig Endosc. 2014;26:220–7.
Nonaka S, Oda I, Tada K, et al. Clinical outcome of endoscopic resection for nonampullary duodenal tumors. Endoscopy. 2014;47:129–35.
Adsay NV, Nagtegaal ID, Reid MD. Non-ampullary adenocarcinoma. In: WHO Classification of Tumours Editorial Board, editor. Digestive system tumours. 5th ed. Lyon: IARC; 2019. p. 124–6.
Hashimoto T, Ogawa R, Matsubara A, et al. Familial adenomatous polyposis-associated and sporadic pyloric gland adenomas of the upper gastrointestinal tract share common genetic features. Histopathology. 2015;67:689–98.
Mahajan D, Downs-Kelly E, Liu X, et al. Reproducibility of the villous component and high-grade dysplasia in colorectal adenomas <1 cm: implications for endoscopic surveillance. Am J SurgPathol. 2013;37:427–33.
Sekine S, Mori T, Ogawa R, et al. Mismatch repair deficiency commonly precedes adenoma formation in Lynch Syndrome-Associated colorectal tumorigenesis. Mod Pathol. 2017;30:1144–51.
Chan AO-O, Broaddus RR, Houlihan PS, et al. CpG island methylation in aberrant crypt foci of the colorectum. Am J Pathol. 2002;160:1823–30.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Christie M, Jorissen RN, Mouradov D, et al. Different APC genotypes in proximal and distal sporadic colorectal cancers suggest distinct WNT/β-catenin signalling thresholds for tumourigenesis. Oncogene. 2013;32:4675–82.
Matsubara A, Sekine S, Kushima R, et al. Frequent GNAS and KRAS mutations in pyloric gland adenoma of the stomach and duodenum. J Pathol. 2013;229:579–87.
Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. JNCI J Natl Cancer Inst. 2004;96:261–8.
Yoshida M, Shimoda T, Abe M, et al. Clinicopathological characteristics of non-ampullary duodenal tumors and their phenotypic classification. Pathol Int. 2019;69:398–406.
Mitsuishi T, Hamatani S, Hirooka S, et al. Clinicopathological characteristics of duodenal epithelial neoplasms: Focus on tumors with a gastric mucin phenotype (pyloric gland-type tumors). PLoS ONE. 2017;12:e0174985.
Hijikata K, Nemoto T, Igarashi Y, et al. Extra-ampullary duodenal adenoma: a clinicopathological study. Histopathology. 2017;71:200–7.
Campos FG, Martinez CAR, Bustamante Lopez LA, et al. Advanced duodenal neoplasia and carcinoma in familial adenomatous polyposis: outcomes of surgical management. J Gastrointest Oncol. 2017;8:877–84.
Chen Z-M, Scudiere JR, Abraham SC, et al. Pyloric gland adenoma: an entity distinct from gastric foveolar type adenoma. Am J Surg Pathol. 2009;33:186–93.
Miller GC, Kumarasinghe MP, Borowsky J, et al. Clinicopathological features of pyloric gland adenomas of the duodenum: a multicentre study of 57 cases. Histopathology. 2020;76:404–10.
Vieth M, Kushima R, Borchard F, et al. Pyloric gland adenoma: a clinico-pathological analysis of 90 cases. Virchows Arch. 2003;442:317–21.
Abraham SC, Nobukawa B, Giardiello FM, et al. Fundic gland polyps in familial adenomatous polyposis. Am J Pathol. 2000;157:747–54.
Rokutan H, Abe H, Nakamura H, et al. Initial and crucial genetic events in intestinal-type gastric intramucosal neoplasia: early mutations of gastric intramucosal neoplasia. J Pathol. 2019;247:494–504.
Ota R, Sawada T, Tsuyama S, et al. Integrated genetic and epigenetic analysis of cancer-related genes in non-ampullary duodenal adenomas and intramucosal adenocarcinomas. J Pathol. 2020;252:330–42.
Toyooka M, Konishi M, Kikuchi-Yanoshita R, et al. Somatic mutations of the adenomatous polyposis coli gene in gastroduodenal tumors from patients with familial adenomatous polyposis. Cancer Res. 1995;55:3165–70.
Groves C, Lamlum H, Crabtree M, et al. Mutation cluster region, association between germline and somatic mutations and genotype-phenotype correlation in upper gastrointestinal familial adenomatous polyposis. Am J Pathol. 2002;160:2055–61.
Loman NJ, Misra RV, Dallman TJ, et al. Performance comparison of benchtop high-throughput sequencing platforms. Nat Biotechnol. 2012;30:434–9.
Reid MD, Balci S, Ohike N, et al. Ampullary carcinoma is often of mixed or hybrid histologic type: an analysis of reproducibility and clinical relevance of classification as pancreatobiliary versus intestinal in 232 cases. Mod Pathol. 2016;29:1575–85.
Watari J, Mitani S, Ito C, et al. Molecular alterations and PD-L1 expression in non-ampullary duodenal adenocarcinoma: Associations among clinicopathological, immunophenotypic and molecular features. Sci Rep. 2019;9:10526.
Aparicio T, Svrcek M, Zaanan A, et al. Small bowel adenocarcinoma phenotyping, a clinicobiological prognostic study. Br J Cancer. 2013;109:3057–66.
Overman MJ, Pozadzides J, Kopetz S, et al. Immunophenotype and molecular characterisation of adenocarcinoma of the small intestine. Br J Cancer. 2010;102:144–50.
Planck M, Ericson K, Piotrowska Z, et al. Microsatellite instability and expression of MLH1 and MSH2 in carcinomas of the small intestine. Cancer. 2003;97:1551–7.
Jenkins MA, Hayashi S, O’Shea A-M, et al. Pathology features in Bethesda guidelines predict colorectal cancer microsatellite instability: a population-based study. Gastroenterology. 2007;133:48–56.
Koornstra JJ, Kleibeuker JH, Vasen HF. Small-bowel cancer in Lynch syndrome: is it time for surveillance? Lancet Oncol. 2008;9:901–5.
Acknowledgements
We thank Ms. Reiko Ogawa, Ms. Sachiko Miura, Ms. Toshiko Sakaguchi, and Ms. Chizu Kina for their skillful technical assistance. This work was supported by JSPS KAKENHI Grant Number 20K07401.
Author information
Authors and Affiliations
Contributions
KI, TH, and SS designed the study. TH and SS performed mutation analyses. KI, TH, TN, YY, and SS performed histological and immunohistochemical analyses. MK, TK, SN, IO, ME, MK, NG, TYoshida, and TYoshikawa provided tissue samples and clinical information. KI and SS wrote the manuscript. All authors contributed to discussions and gave final approval of the submitted manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ishizu, K., Hashimoto, T., Naka, T. et al. APC mutations are common in adenomas but infrequent in adenocarcinomas of the non-ampullary duodenum. J Gastroenterol 56, 988–998 (2021). https://doi.org/10.1007/s00535-021-01823-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-021-01823-x