Abstract
Background
Prophylactic somatostatin to reduce the incidence of clinically relevant postoperative pancreatic fistula after pancreaticoduodenectomy remains controversial. We assessed the preventive efficacy of somatostatin on clinically relevant postoperative pancreatic fistula in intermediate-risk patients who underwent pancreaticoduodenectomy at pancreatic centres in China.
Methods
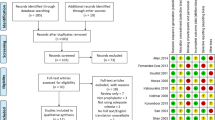
In this multicentre, prospective, randomised controlled trial, we used the updated postoperative pancreatic fistula classification criteria and cases were confirmed by an independent data monitoring committee to improve comparability between centres. The primary endpoint was the rate of clinically relevant postoperative pancreatic fistula within 30 days after pancreaticoduodenectomy.
Results
Eligible patients (randomised, n = 205; final analysis, n = 199) were randomised to receive postoperative intravenous somatostatin (250 μg/h over 120 h; n = 99) or conventional therapy (n = 100). The primary endpoint was significantly lower in the somatostatin vs control group (n = 13 vs n = 25; 13% vs 25%, P = 0.032). There were no significant differences for biochemical leak (P = 0.289), biliary fistula (P = 0.986), abdominal infection (P = 0.829), chylous fistula (P = 0.748), late postoperative haemorrhage (P = 0.237), mean length of hospital stay (P = 0.512), medical costs (P = 0.917), reoperation rate (P > 0.99), or 30 days’ readmission rate (P = 0.361). The somatostatin group had a higher rate of delayed gastric emptying vs control (n = 33 vs n = 21; 33% vs 21%, P = 0.050).
Conclusions
Prophylactic somatostatin treatment reduced clinically relevant postoperative pancreatic fistula in intermediate-risk patients after pancreaticoduodenectomy.
Trial registration
NCT03349424.


Similar content being viewed by others
References
Xiang Y, Wu J, Lin C, et al. Pancreatic reconstruction techniques after pancreaticoduodenectomy: a review of the literature. Expert Rev Gastroenterol Hepatol. 2019;13:797–806.
Nahm CB, Connor SJ, Samra JS, et al. Postoperative pancreatic fistula: a review of traditional and emerging concepts. Clin Exp Gastroenterol. 2018;11:105–18.
Wang J, Ma R, Churilov L, et al. The cost of perioperative complications following pancreaticoduodenectomy: a systematic review. Pancreatology. 2018;18:208–20.
Cheng Y, Briarava M, Lai M, et al. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction for the prevention of postoperative pancreatic fistula following pancreaticoduodenectomy. Cochrane Database Syst Rev. 2017;9: CD012257.
Huttner FJ, Fitzmaurice C, Schwarzer G, et al. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2016;2: CD006053.
Shubert CR, Wagie AE, Farnell MB, et al. Clinical risk score to predict pancreatic fistula after pancreatoduodenectomy: independent external validation for open and laparoscopic approaches. J Am Coll Surg. 2015;221:689–98.
Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:133–64.
Group of Pancreatic surgery, Surgical branch of Chinese Medical Association. A consensus statement on the diagnosis, treatment, and prevention of common complications after pancreatic surgery. Zhonghua wai ke za zhi Chinese J Surg 2017;55:328–334.
Callery MP, Pratt WB, Kent TS, et al. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013;216:1–14.
Han XL, Xu J, Wu WM, et al. Impact of the 2016 new definition and classification system of pancreatic fistula on the evaluation of pancreatic fistula after pancreatic surgery. Zhonghua Wai Ke Za Zhi. 2017;55:528–31 (Article in Chinese).
Gouillat C, Chipponi J, Baulieux J, et al. Randomized controlled multicentre trial of somatostatin infusion after pancreaticoduodenectomy. Br J Surg. 2001;88:1456–62.
Volk A, Nitschke P, Johnscher F, et al. Perioperative application of somatostatin analogs for pancreatic surgery-current status in Germany. Langenbecks Arch Surg. 2016;401:1037–44.
Adiamah A, Arif Z, Berti F, et al. The use of prophylactic somatostatin therapy following pancreaticoduodenectomy: a meta-analysis of randomised controlled trials. World J Surg. 2019;43:1788–801.
Goyert N, Eeson G, Kagedan DJ, et al. Pasireotide for the prevention of pancreatic fistula following pancreaticoduodenectomy: a cost-effectiveness analysis. Ann Surg. 2017;265:2–10.
Dominguez-Rosado I, Fields RC, Woolsey CA, et al. Prospective evaluation of pasireotide in patients undergoing pancreaticoduodenectomy: the Washington University experience. J Am Coll Surg. 2018;226:147-54.e1.
Allen PJ, Gönen M, Brennan MF, et al. Pasireotide for postoperative pancreatic fistula. N Engl J Med. 2014;370:2014–22.
Ratnayake CB, Loveday BP, Shrikhande SV, et al. Impact of preoperative sarcopenia on postoperative outcomes following pancreatic resection: a systematic review and meta-analysis. Pancreatology. 2018;18:996–1004.
Pulvirenti A, Marchegiani G, Pea A, et al. Clinical implications of the 2016 International Study Group on Pancreatic Surgery definition and grading of postoperative pancreatic fistula on 775 consecutive pancreatic resections. Ann Surg. 2018;268:1069–75.
Brennan MF. Quality pancreatic cancer care: it’s still mostly about volume. J Nat Cancer Inst. 2009;101:837–8.
Gani F, Johnston FM, Nelson-Williams H, et al. Hospital volume and the costs associated with surgery for pancreatic cancer. J Gastrointest Surg. 2017;21:1411–9.
Dusch N, Lietzmann A, Barthels F, et al. International study group of pancreatic surgery definitions for postpancreatectomy complications: applicability at a high-volume center. Scand J Surg. 2017;106:216–23.
Shan YS, Sy ED, Tsai ML, et al. Effects of somatostatin prophylaxis after pylorus-preserving pancreaticoduodenectomy: increased delayed gastric emptying and reduced plasma motilin. World J Surg. 2005;29:1319–24.
Sun L, Coy DH. Somatostatin and its analogs. Curr Drug Targets. 2016;17:529–37.
Sato N, Kimura T, Kenjo A, et al. Early intra-abdominal infection following pancreaticoduodenectomy: associated factors and clinical impact on surgical outcome. Fukushima J Med Sci. 2020;66:124–32.
Chen JS, Liu G, Li TR, et al. Pancreatic fistula after pancreaticoduodenectomy: risk factors and preventive strategies. J Cancer Res Ther. 2019;15:857–63.
Watanabe F, Noda H, Kamiyama H, et al. Risk factors for intra-abdominal infection after pancreaticoduodenectomy—a retrospective analysis to evaluate the significance of preoperative biliary drainage and postoperative pancreatic fistula. Hepatogastroenterology. 2012;59:1270–3.
Qu G, Wang D, Xu W, et al. The systemic inflammation-based prognostic score predicts postoperative complications in patients undergoing pancreaticoduodenectomy. Int J Gen Med. 2021;14:787–95.
van Dongen JC, Wismans LV, Suurmeijer JA, et al. The effect of preoperative chemotherapy and chemoradiotherapy on pancreatic fistula and other surgical complications after pancreatic resection: a systematic review and meta-analysis of comparative studies. HPB (Oxford). 2021 May 19:S1365-182X(21)00143-X.
Wang XY, Cai JP, Huang CS, et al. Impact of enhanced recovery after surgery protocol on pancreaticoduodenectomy: a meta-analysis of non-randomized and randomized controlled trials. HPB (Oxford). 2020;22:1373–83.
Liu X, Chen K, Chu X, et al. Prophylactic intra-peritoneal drainage after pancreatic resection: an updated meta-analysis. Front Oncol. 2021;11:658829.
Huan L, Fei Q, Lin H, et al. Is peritoneal drainage essential after pancreatic surgery? A meta-analysis and systematic review. Medicine (Baltimore). 2017;96: e9245.
Mengyi L, Xiaozhen Z, Chenxiang G, et al. External validation of alternative fistula risk score (a-FRS) for predicting pancreatic fistula after pancreatoduodenectomy. HPB (Oxford). 2020;22:58–66.
Acknowledgements
Writing support was provided by Sarah Bubeck, PhD, of Edanz Pharma. This study was funded by Merck Serono Ltd., Beijing, China, an affiliate of Merck KGaA, Darmstadt, Germany.
Author information
Authors and Affiliations
Contributions
Conception and design: TZ, BS, RQ, RC, YM, WL, YZ; Administrative support: JG, TZ, BS, RQ, RC, YM, WL, YZ; Provision of study materials or patients: JG, TZ, BS, RQ, RC, YM, WL, YZ; Collection and assembly of data: ZC, JQ, JG, GX, KJ, SZ, TK, YW; Data analysis and interpretation: ZC, JQ, JG, GX, KJ, SZ, TK, YW; Manuscript writing: all authors; Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cao, Z., Qiu, J., Guo, J. et al. A randomised, multicentre trial of somatostatin to prevent clinically relevant postoperative pancreatic fistula in intermediate-risk patients after pancreaticoduodenectomy. J Gastroenterol 56, 938–948 (2021). https://doi.org/10.1007/s00535-021-01818-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-021-01818-8