Abstract
Background
Achalasia has been reported to be associated with esophageal cancers (ECs). However, owing to the rarity of achalasia, details of achalasia-related ECs are not well investigated.
Method
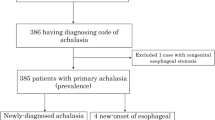
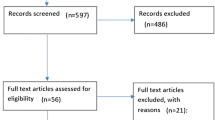
The incidence of ECs in Japanese patients with achalasia and achalasia-related esophageal motility disorders (EMDs) was estimated, and risk factors for achalasia-related ECs were determined. Characteristics of ECs and treatment courses were also analyzed.
Results
Between 2010 and 2019, 2714 Japanese patients with achalasia and achalasia-related EMDs were recorded in 7 high-volume centers; 24 patients (21 men, 3 women) developed ECs. The incidence of ECs was estimated at 0.078 and 0.28 per 100 person-years from the onset and the diagnosis of disease, respectively. Kaplan–Meier estimate suggested that, in addition to a long history of achalasia, advanced age, male sex, and regular alcohol consumption were statistically significant risk factors for EC development. A prevalence of 40 ECs (12.5% multiple lesions, and 22.7% metachronal lesions) was also noted, predominantly distributed over the thoracic esophagus. All were histologically diagnosed as squamous cell carcinoma. Superficial ECs were successfully treated with endoscopic treatment in all cases, except one. Achalasia-related Barret esophagus was extremely rare, and Barret adenocarcinoma was not detected in our cohort.
Conclusion
The high relative risk of ECs was clarified in Japanese achalasia patients, although the absolute risk remained low. Therefore, surveillance endoscopy may be recommended in limited patients with several aforementioned risk factors determined. Superficial cancer can be treated with endoscopic treatment. Multiple and metachronal ECs should be screened.



Similar content being viewed by others
References
Richter JE. Oesophageal motility disorders. Lancet. 2001;358:823–8.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83–93.
Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010;139:369–74.
Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404–14.
Sato H, Takahashi K, Mizuno KI, et al. Esophageal motility disorders: new perspectives from high-resolution manometry and histopathology. J Gastroenterol. 2018;53:484–93.
Duffield JA, Hamer PW, Heddle R, et al. Incidence of achalasia in South Australia based on esophageal manometry findings. Clin Gastroenterol Hepatol. 2017;15:360–5.
Samo S, Carlson DA, Gregory DL, et al. Incidence and prevalence of achalasia in central Chicago, 2004–2014, since the widespread use of high-resolution manometry. Clin Gastroenterol Hepatol. 2017;15:366–73.
Harvey PR, Thomas T, Chandan JS, et al. Incidence, morbidity and mortality of patients with achalasia in England: findings from a study of nationwide hospital and primary care data. Gut. 2019;68:790–5.
van Hoeij FB, Ponds FA, Smout AJ, et al. (2018) Incidence and costs of achalasia in The Netherlands. Neurogastroenterol Motil 30.
Kim E, Lee H, Jung HK, et al. Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci. 2014;29:576–80.
Booy JD, Takata J, Tomlinson G, et al. The prevalence of autoimmune disease in patients with esophageal achalasia. Dis Esophagus. 2012;25:209–13.
Sato H, Yokomichi H, Takahashi K, et al. Epidemiological analysis of achalasia in Japan using a large-scale claims database. J Gastroenterol. 2019;54:621–7.
Torres-Aguilera M, Remes Troche JM. Achalasia and esophageal cancer: risks and links. Clin Exp Gastroenterol. 2018;11:309–16.
Tustumi F, Bernardo WM, da Rocha JRM, et al. Esophageal achalasia: a risk factor for carcinoma. A systematic review and meta-analysis. Dis Esophagus. 2017;30:1–8.
Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108:1238–49.
Hirota WK, Zuckerman MJ, Adler DG, et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570–80.
Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020;115:1393–411.
Oude Nijhuis RAB, Zaninotto G, Roman S, et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and motility recommendations. United Eur Gastroenterol J. 2020;8:13–33.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015;221:256–64.
Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371:836–45.
The Japan Esophageal Society. Guidelines for the clinical and pathologic studies on carcinoma of the esophagus. 11th ed. Kanehara Co. Tokyo, Japan.
Japan ES. Japanese classification of esophageal cancer, 11th edition: part I. Esophagus. 2017;14:1–36.
Rice TW, Patil DT, Blackstone EH. 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: application to clinical practice. Ann Cardiothorac Surg. 2017;6:119–30.
Board WCoTE. WHO classification of tumours, 5th ed., Vol.1. 2019.
Statistics Bureau, Ministry of internal affairs and communications website (https://www.stat.go.jp/english/index.html).
Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010;105:2144–9.
Zendehdel K, Nyren O, Edberg A, et al. Risk of esophageal adenocarcinoma in achalasia patients, a retrospective cohort study in Sweden. Am J Gastroenterol. 2011;106:57–61.
Ohashi S, Miyamoto S, Kikuchi O, et al. Recent advances from basic and clinical studies of esophageal squamous cell carcinoma. Gastroenterology. 2015;149:1700–15.
Sikkema M, de Jonge PJ, Steyerberg EW, et al. Risk of esophageal adenocarcinoma and mortality in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–44.
Desai TK, Krishnan K, Samala N, et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012;61:970–6.
Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: orient to occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–35.
Ichkhanian Y, Benias P, Khashab MA. Case of early Barrett cancer following peroral endoscopic myotomy. Gut. 2019;68:2107–10.
Amano Y, Ishimura N, Furuta K, et al. Which landmark results in a more consistent diagnosis of Barrett’s esophagus, the gastric folds or the palisade vessels? Gastrointest Endosc. 2006;64:206–11.
Amano Y, Kinoshita Y. Barrett esophagus: perspectives on its diagnosis and management in asian populations. Gastroenterol Hepatol. 2008;4:45–53.
Lordick F, Mariette C, Haustermans K, et al. Oesophageal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27:v50–7.
Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive registry of esophageal cancer in Japan, 2012. Esophagus. 2019;16:221–45.
Ponds FA, Moonen A, Smout A, et al. Screening for dysplasia with Lugol chromoendoscopy in longstanding idiopathic achalasia. Am J Gastroenterol. 2018;113:855–62.
Markar SR, Wiggins T, MacKenzie H, et al. (2019) Incidence and risk factors for esophageal cancer following achalasia treatment: national population-based case-control study. Dis Esophagus 32.
Acknowledgements
We would like to thank Editage [http://www.editage.com] for editing and reviewing this manuscript for the English language.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
Hiroki Sato accepts official responsibility for the overall conduct of this study and the publication of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sato, H., Terai, S., Shimamura, Y. et al. Achalasia and esophageal cancer: a large database analysis in Japan. J Gastroenterol 56, 360–370 (2021). https://doi.org/10.1007/s00535-021-01763-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-021-01763-6