Abstract
Background
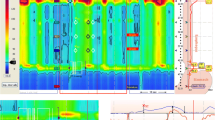
Achalasia and esophagogastric junction outflow obstruction (EGJOO) are idiopathic esophageal motility disorders characterized by impaired deglutitive relaxation of the lower esophageal sphincter (LES). High-resolution manometry (HRM) provides integrated relaxation pressure (IRP) which represents adequacy of LES relaxation. The Starlet HRM system is widely used in Japan; however, IRP values in achalasia/EGJOO patients assessed with the Starlet system have not been well studied. We propose the optimal cutoff of IRP for detecting achalasia/EGJOO using the Starlet system.
Methods
Patients undergone HRM test using the Starlet system at our institution between July 2018 and September 2020 were included. Of these, we included patients with either achalasia or EGJOO and those who had normal esophageal motility without hiatal hernia. Abnormally impaired LES relaxation (i.e., achalasia and EGJOO) was diagnosed if prolonged esophageal emptying was evident based on timed barium esophagogram (TBE).
Results
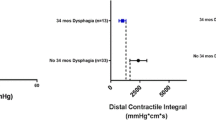
A total of 111 patients met study criteria. Of these, 48 patients were diagnosed with achalasia (n = 45 [type I, n = 20; type II, n = 22; type III, n = 3]) or EGJOO (n = 3). In the 48 patients who had a prolonged esophageal clearance based on TBE, IRP values distributed along a wide-range of minimal 14.1 to a maximal of 72.2 mmHg. The optimal cutoff value of IRP was 24.7 mmHg with sensitivity of 89.6% and specificity of 84.1% (AUC 0.94).
Conclusion
The optimal cutoff value of IRP to distinguish achalasia/EGJOO was ≥ 25 mmHg using the Starlet HRM system in our cohort. This indicates that the current proposed cutoff of 26 mmHg appears to be relevant.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the ROC curve
- CT:
-
Computed tomography
- EGD:
-
Esophagogastroduodenoscopy
- EGJ:
-
Esophagogastric junction
- EGJOO:
-
EGJ outflow obstruction
- FLIP:
-
Functional luminal imaging probe
- HRM:
-
High-resolution manometry
- IRP:
-
Integrated relaxation pressure
- LES:
-
Lower esophageal sphincter
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- TBE:
-
Timed barium esophagogram
References
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74.
Kuribayashi S, Iwakiri K, Kawada A, et al. Variant parameter values-as defined by the Chicago Criteria-produced by ManoScan and a new system with Unisensor catheter. Neurogastroenterol Motil. 2015;27:188–94.
Kuribayashi S, Iwakiri K, Shinozaki T, et al. Clinical impact of different cut-off values in high-resolution manometry systems on diagnosing esophageal motility disorders. J Gastroenterol. 2019;54:1078–82.
de Oliveira JM, Birgisson S, Doinoff C, et al. Timed barium swallow: a simple technique for evaluating esophageal emptying in patients with achalasia. Am J Roentgenol. 1997;169:473–9.
Kostic SV, Rice TW, Baker ME, et al. Timed barium esophagogram: a simple physiologic assessment for achalasia. J Thorac Cardiovasc Surg. 2000;120:935–46.
Kostic S, Andersson M, Hellström M, et al. Timed barium esophagogram in the assessment of patients with achalasia: reproducibility and observer variation. Dis Esophagus. 2005;18:96–103.
Hoshino M, Omura N, Yano F, et al. Is esophageal manometry essential for the diagnosis of achalasia? Identifying patients with achalasia by the esophageal clearance method. Esophagus. 2020;2:10–23.
Japan Esophageal Society. Descriptive rules for achalasia of the esophagus, June 2012: 4th Edition. Esophagus. 2017;14:275–89.
Bredenoord AJ, Hebbard GS. Technical aspects of clinical high-resolution manometry studies. Neurogastroenterol Motil. 2012;24(Suppl 1):5–10.
Xiang X, Tu L, Zhang X, et al. Influence of the catheter diameter on the investigation of the esophageal motility through solid-state high-resolution manometry. Dis Esophagus. 2013;26:661–7.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83–93.
Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA. 2015;313:1841.
Kawami N, Hoshino S, Hoshikawa Y, et al. Validity of the cutoff value for integrated relaxation pressure used in the starlet high-resolution manometry system. J Nippon Med Sch. 2020;86:322–6.
Lin Z, Kahrilas PJ, Roman S, et al. Refining the criterion for an abnormal integrated relaxation pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model: Improving IRP cutoff value for diagnosing achalasia. Neurogastroenterol Motil. 2012;24:e356–63.
Ponds FA, Bredenoord AJ, Kessing BF, et al. Esophagogastric junction distensibility identifies achalasia subgroup with manometrically normal esophagogastric junction relaxation. Neurogastroenterol Motil. 2017;29:e12908.
Rohof WO, Salvador R, Annese V, et al. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology. 2013;144:718–25.
Kane ED, Budhraja V, Desilets DJ, et al. Myotomy length informed by high-resolution esophageal manometry (HREM) results in improved per-oral endoscopic myotomy (POEM) outcomes for type III achalasia. Surg Endosc. 2019;33:886–94.
Acknowledgment
The authors are very grateful to Dr. Balázs Kovács for his critical review and his assistance of English language editing.
Author information
Authors and Affiliations
Contributions
TM: study conception and design, acquisition of data, analysis and interpretation of results, drafting of manuscript, study supervision. FY: critical review of manuscript, acquisition of data. NO: critical review of manuscript. KT, MH, SY, SA, YS, and NF: writing assistance, acquisition of data. HK: critical review of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Masuda, T., Yano, F., Omura, N. et al. Optimal cutoff value of integrated relaxation pressure on the esophagogastric junction to detect outflow obstruction using starlet high-resolution manometry system. J Gastroenterol 56, 231–239 (2021). https://doi.org/10.1007/s00535-020-01757-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-020-01757-w