Abstract
Background
The macroscopic type of hepatocellular carcinoma (HCC) is a predictor of prognosis. We clarified the diagnostic value of gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA)–enhanced magnetic resonance imaging (MRI) in the macroscopic classification of nodular hepatocellular carcinoma (HCC) as compared to angiography-assisted computed tomography (CT).
Methods
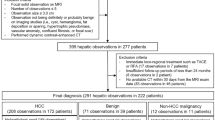
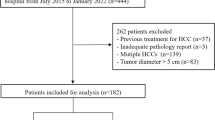
A total of 71 surgically resected nodular HCCs with a maximum diameter of ≤5 cm were investigated. HCCs were evaluated preoperatively using Gd-EOB-DTPA–enhanced MRI and angiography-assisted CT. HCCs were pathologically classified as simple nodular (SN), SN with extranodular growth (SN-EG), or confluent multinodular (CMN). SN-EG and CMN were grouped as non-SN. Five readers independently reviewed the images using a five-point scale. We examined the accuracy of both imaging modalities in differentiating between SN and non-SN HCC.
Results
Overall, the area under the receiver operating characteristic curve (A z ) for the diagnosis of non-SN did not differ between Gd-EOB-DTPA–enhanced MRI and angiography-assisted CT [0.879 (95 % confidence interval (CI), 0.779–0.937) and 0.845 (95 % CI, 0.723–0.919), respectively]. For HCCs >2 cm, the A z for Gd-EOB-DTPA–enhanced MRI was greater than 0.9. The sensitivity, specificity, and accuracy of Gd-EOB-DTPA–enhanced MRI for identifying non-SN were equal to or higher than values with angiography-assisted CT in all three categories (all tumors, ≤2 cm, and >2 cm), but the differences were not statistically significant.
Conclusions
Using Gd-EOB-DTPA–enhanced MRI to assess the macroscopic findings in nodular HCC was equal or superior to using angiography-assisted CT.




Similar content being viewed by others
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- CT:
-
Computed tomography
- CTAP:
-
CT during arterial portography
- CTHA:
-
CT during hepatic arteriography
- Gd-EOB-DTPA:
-
Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid
- MRI:
-
Magnetic resonance imaging
- SN:
-
Simple nodular
- SN-EG:
-
Simple nodular with extranodular growth
- CMN:
-
Confluent multinodular
- ROC:
-
Receiver operating characteristic
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
References
El-Serag HB. Epidemiology of hepatocellular carcinoma in USA. Hepatol Res. 2007;37(Suppl 2):88–94.
Shimada M, Rikimaru T, Hamatsu T, et al. The role of macroscopic classification in nodular-type hepatocellular carcinoma. Am J Surg. 2001;182:177–82.
Hui AM, Takayama T, Sano K, et al. Predictive value of gross classification of hepatocellular carcinoma on recurrence and survival after hepatectomy. J Hepatol. 2000;33:975–9.
Inayoshi J, Ichida T, Sugitani S, et al. Gross appearance of hepatocellular carcinoma reflects E-cadherin expression and risk of early recurrence after surgical treatment. J Gastroenterol Hepatol. 2003;18:673–7.
Kondo K, Chijiiwa K, Makino I, et al. Risk factors for early death after liver resection in patients with solitary hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2005;12:399–404.
Matsui O, Kadoya M, Kameyama T, et al. Benign and malignant nodules in cirrhotic livers: distinction based on blood supply. Radiology. 1991;178:493–7.
Hayashi M, Matsui O, Ueda K, et al. Progression to hypervascular hepatocellular carcinoma: correlation with intranodular blood supply evaluated with CT during intraarterial injection of contrast material. Radiology. 2002;225:143–9.
Matsui O, Takashima T, Kadoya M, et al. Dynamic computed tomography during arterial portography: the most sensitive examination for small hepatocellular carcinomas. J Comput Assist Tomogr. 1985;9:19–24.
Murakami T, Takamura M, Kim T, et al. Double phase CT during hepatic arteriography for diagnosis of hepatocellular carcinoma. Eur J Radiol. 2005;54:246–52.
Hayashi M, Matsui O, Ueda K, et al. Correlation between the blood supply and grade of malignancy of hepatocellular nodules associated with liver cirrhosis: evaluation by CT during intraarterial injection of contrast medium. AJR Am J Roentgenol. 1999;172:969–76.
Vogl TJ, Kümmel S, Hammerstingl R, et al. Liver tumors: comparison of MR imaging with Gd-EOB-DTPA and Gd-DTPA. Radiology. 1996;200:59–67.
Huppertz A, Balzer T, Blakeborough A, et al. Improved detection of focal liver lesions at MR imaging: multicenter comparison of gadoxetic acid-enhanced MR images with intraoperative findings. Radiology. 2004;230:266–75.
Bluemke DA, Sahani D, Amendola M, et al. Efficacy and safety of MR imaging with liver-specific contrast agent: US multicenter phase III study. Radiology. 2005;237:89–98.
Huppertz A, Haraida S, Kraus A, et al. Enhancement of focal liver lesions at gadoxetic acid-enhanced MR imaging: correlation with histopathologic findings and spiral CT–initial observations. Radiology. 2005;234:468–78.
Saito K, Kotake F, Ito N, et al. Gd-EOB-DTPA–enhanced MRI for hepatocellular carcinoma: quantitative evaluation of tumor enhancement in hepatobiliary phase. Magn Reson Med Sci. 2005;4:1–9.
Schuhmann-Giampieri G, Schmitt-Willich H, Press WR, et al. Preclinical evaluation of Gd-EOB-DTPA as a contrast agent in MR imaging of the hepatobiliary system. Radiology. 1992;183:59–64.
Hamm B, Staks T, Mühler A, et al. Phase I clinical evaluation of Gd-EOB-DTPA as a hepatobiliary MR contrast agent: safety, pharmacokinetics, and MR imaging. Radiology. 1995;195:785–92.
Ariizumi S, Kitagawa K, Kotera Y, et al. A non-smooth tumor margin in the hepatobiliary phase of gadoxetic acid disodium (Gd-EOB-DTPA)-enhanced magnetic resonance imaging predicts microscopic portal vein invasion, intrahepatic metastasis, and early recurrence after hepatectomy in patients with hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2011;18:575–85.
Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9.
Frericks BB, Loddenkemper C, Huppertz A, et al. Qualitative and quantitative evaluation of hepatocellular carcinoma and cirrhotic liver enhancement using Gd-EOB-DTPA. AJR Am J Roentgenol. 2009;193:1053–60.
Liver Cancer Study Group of Japan. General rules for the clinical and pathological study of primary liver cancer. 3rd ed. Tokyo: Kanehara & Co., Ltd; 2010. p. 17–8.
Akobeng AK. Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007;96:644–7.
Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–93.
Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003;228:303–8.
Nathan H, Raut CP, Thornton K, et al. Predictors of survival after resection of retroperitoneal sarcoma: a population-based analysis and critical appraisal of the AJCC staging system. Ann Surg. 2009;250:970–6.
Ikai I, Arii S, Kojiro M, et al. Reevaluation of prognostic factors for survival after liver resection in patients with hepatocellular carcinoma in a Japanese nationwide survey. Cancer. 2004;101:796–802.
Grazi GL, Cescon M, Ravaioli M, et al. Liver resection for hepatocellular carcinoma in cirrhotics and noncirrhotics. Evaluation of clinicopathologic features and comparison of risk factors for long-term survival and tumour recurrence in a single centre. Aliment Pharmacol Ther. 2003;17(Suppl 2):119–29.
Eguchi S, Takatsuki M, Hidaka M, et al. Predictor for histological microvascular invasion of hepatocellular carcinoma: a lesson from 229 consecutive cases of curative liver resection. World J Surg. 2010;34:1034–8.
Pawlik TM, Poon RT, Abdalla EK, et al. International Cooperative Study Group on Hepatocellular Carcinoma. Critical appraisal of the clinical and pathologic predictors of survival after resection of large hepatocellular carcinoma. Arch Surg. 2005;140:450–7.
Nakashima Y, Nakashima O, Tanaka M, et al. Portal vein invasion and intrahepatic micrometastasis in small hepatocellular carcinoma by gross type. Hepatol Res. 2003;26:142–7.
Yamamoto M, Takasaki K, Ohtsubo T, et al. Effectiveness of systematized hepatectomy with Glisson’s pedicle transection at the hepatic hilus for small nodular hepatocellular carcinoma: retrospective analysis. Surgery. 2001;130:443–8.
Reimer P, Rummeny EJ, Shamsi K, et al. Phase II clinical evaluation of Gd-EOB-DTPA: dose, safety aspects, and pulse sequence. Radiology. 1996;199:177–83.
Kogita S, Imai Y, Okada M, et al. Gd-EOB-DTPA-enhanced magnetic resonance images of hepatocellular carcinoma: correlation with histological grading and portal blood flow. Eur Radiol. 2010;20:2405–13.
Okada M, Imai Y, Kim T, et al. Comparison of enhancement patterns of histologically confirmed hepatocellular carcinoma between gadoxetate- and ferucarbotran-enhanced magnetic resonance imaging. J Magn Reson Imaging. 2010;32:903–13.
Fujinaga Y, Kadoya M, Kozaka K, et al. Prediction of macroscopic findings of hepatocellular carcinoma on hepatobiliary phase of gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging: correlation with pathology. Hepatol Res. 2013;43:488–94.
Kubota K, Tamura T, Aoyama N, et al. Correlation of liver parenchymal gadolinium-ethoxybenzyl diethylenetriaminepentaacetic acid enhancement and liver function in humans with hepatocellular carcinoma. Oncol Lett. 2012;3:990–4.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tada, T., Kumada, T., Toyoda, H. et al. Diagnostic accuracy for macroscopic classification of nodular hepatocellular carcinoma: comparison of gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging and angiography-assisted computed tomography. J Gastroenterol 50, 85–94 (2015). https://doi.org/10.1007/s00535-014-0947-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-014-0947-x