Abstract
Background
The ability of serum infliximab level to predict clinical outcome in infliximab therapy in Crohn’s disease is unclear. Here, we aimed to clarify the correlation between the timing of loss of response (LOR) to treatment and a decrease in serum infliximab level, and, in addition, to identify an indicator of infliximab level.
Methods
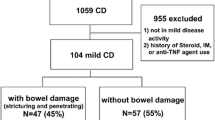
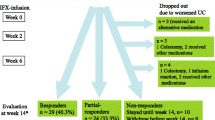
The study used data from a previous clinical study of infliximab for Crohn’s disease, in which infliximab was initially given at 0, 2, 6 weeks at 5 mg/kg, and then at 8-week intervals to 62 week-10 responders. Of these 62, here we analysed data from 57 in whom Crohn’s disease activity index and serum infliximab level were evaluated at week 14.
Results
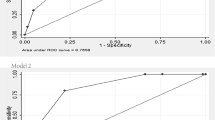
Twelve patients showed a clinical response despite an infliximab level <1 μg/mL at week 14; of these, 8 (67 %) experienced LOR by week 54. A decrease in infliximab level preceded LOR in 6 (75 %). In receiver operating characteristic curve analysis, C-reactive protein (CRP) showed better performance in detecting an infliximab level <1 μg/mL. Infliximab level was <1 μg/mL in 60–80 % of patients with CRP >0.5 mg/dL. Time to LOR (median: 22.0 weeks) was significantly longer than that to a decrease in infliximab level to <1 μg/mL (14.0 weeks, p < 0.05) or to an increase in CRP to >0.5 mg/dL (14.0 weeks, p < 0.01).
Conclusions
A decrease in serum infliximab level preceded LOR, and was easily detected by an increase in CRP. The CRP may be an indicator of serum infliximab level in predicting LOR.






Similar content being viewed by others
References
Peyrin-Biroulet L, Loftus EV Jr, Colombel J-F, Sandborn WJ. The natural history of adult Crohn’s disease in population-based cohorts. Am J Gastroenterol. 2010;105:289–97.
Targan SR, Hanauer SB, van Deventer SJ, Mayer L, Present DH, Braakman T, et al. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor α for Crohn’s disease. N Engl J Med. 1997;337:1029–35.
Hanauer SB, Feagan BG, Lichtenstein GR, Mayer LF, Schreiber S, Colombel JF, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359:1541–9.
Gisbert JP, Panés J. Loss of response and requirement of infliximab dose intensification in Crohn’s disease: a review. Am J Gastroenterol. 2009;104:760–7.
Allez M, Karmiris K, Louis E, Assche GV, Ben-Horin S, Klein A, et al. Report of the ECCO pathogenesis workshop on anti-TNF therapy failures in inflammatory bowel diseases: definitions, frequency and pharmacological aspects. J Crohns Colitis. 2010;4:355–66.
Sandborn WJ, Hanauer SB. Infliximab in the treatment of Crohn’s disease: a user’s guide for clinicians. Am J Gastroenterol. 2002;97:2962–72.
Hibi T, Sakuraba A, Watanabe M, Motoya S, Ito H, Motegi K, et al. Retrieval of serum infliximab level by shortening the maintenance infusion interval is correlated with clinical efficacy in Crohn’s disease. Inflamm Bowel Dis. 2012;18:1480–7.
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfarlane JD, et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor α monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998;41:1552–63.
Maser EA, Villela R, Silverberg MS, Greenberg GR. Association of trough serum infliximab to clinical outcome after scheduled maintenance treatment for Crohn’s disease. Clin Gastroenterol Hepatol. 2006;4:1248–54.
Afif W, Loftus EV Jr, Faubion WA, Kane SV, Bruining DH, Hanson KA, et al. Clinical utility of measuring infliximab and human anti-chimeric antibody concentrations in patients with inflammatory bowel disease. Am J Gastroenterol. 2010;105:1133–9.
Guerra I, Chaparro M, Bermejo F, Gisbert JP. Utility of measuring serum concentrations of anti-TNF agents and anti-drug antibodies in inflammatory bowel disease. Curr Drug Metab. 2011;12:594–8.
Sartor RB. Mechanisms of disease: pathogenesis of Crohn’s disease and ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol. 2006;3:390–407.
Louis E, Belaiche J, van Kemseke C, Franchimont D, de Groote D, Gueenen V, et al. A high serum concentration of interleukin-6 is predictive of relapse in quiescent Crohn’s disease. Eur J Gastroenterol Hepatol. 1997;9:939–44.
Song L, Hanlon DW, Chang L, Provuncher GK, Kan CW, Campbell TG, et al. Single molecule measurements of tumor necrosis factor α and interleukin-6 in the plasma of patients with Crohn’s disease. J Immunol Methods. 2011;372:177–86.
Kato K, Fukunaga K, Kamikozuru K, Kashiwamura S, Hida N, Ohda Y, et al. Infliximab therapy impacts the peripheral immune system of immunomodulator and corticosteroid naïve patients with Crohn’s disease. Gut Liver. 2011;5:37–45.
Charles P, Elliott MJ, Davis D, Potter A, Kalden JR, Antoni C, et al. Regulation of cytokines, cytokine inhibitors, and acute-phase proteins following anti-TNF-α therapy in rheumatoid arthritis. J Immunol. 1999;163:1521–8.
Knudsen LS, Ostergaard M, Baslund B, Narvestad E, Petersen J, Nielsen HJ, et al. Plasma IL-6, plasma VEGF, and serum YKL-40: relationship with disease activity and radiographic progression in rheumatoid arthritis patients treated with infliximab and methotrexate. Scand J Rheumatol. 2006;35:489–91.
Dain L, Braun-Moscovici Y, Baum E, Nahir AM, Hoffer E. Modification of neutrophil function by plasma of rheumatoid arthritis patients treated with infliximab. Clin Exp Rheumatol. 2006;24:38–44.
Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006;55:426–31.
Jürgens M, Mahachie John JM, Cleynen I, Schnitzler F, Fidder H, van Moerkercke W, et al. Levels of C-reactive protein are associated with response to infliximab therapy in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:421–7.
Reinisch W, Wang Y, Oddens BJ, Link R. C-reactive protein, an indicator for maintained response or remission to infliximab in patients with Crohn’s disease: a post-hoc analysis from ACCENT I. Aliment Pharmacol Ther. 2012;35:568–76.
Kiss LS, Papp M, Lovasz BD, Vegh Z, Golovics PA, Janka E, et al. High-sensitivity C-reactive protein for identification of disease phenotype, active disease, and clinical relapses in Crohn’s disease: a marker for patient classification? Inflamm Bowel Dis. 2012;18:1647–54.
Acknowledgments
This study was sponsored by Mitsubishi Tanabe Pharma Corporation. The authors thank the patients, investigators, and study personnel who made the trial possible. We also thank the following investigators for their involvement: Noriaki Watanabe (Department of Internal Medicine, Kitasato Institute Hospital, Tokyo, Japan), Tomoe Katsumata (Department of Gastroenterology, Kitasato University East Hospital, Sagamihara, Japan), Hidemi Goto (Department of Gastroenterology, Nagoya University Graduate School of Medicine, Nagoya, Japan), Akiyoshi Nishio (Department of Gastroenterological Endoscopy, Kyoto University Hospital, Kyoto, Japan).
Conflict of interest
T. Hibi has received grant/research support from Ajinomoto Pharmaceuticals, JIMRO, and Mitsubishi Tanabe Pharma. M. Watanabe has received grant/research support and lecture fees from Abbott Japan, Ajinomoto Pharmaceuticals, Asahi Kasei Medical, Astellas Pharma, AstraZeneca, Chugai Pharmaceutical, DAIICHI SANKYO, Eisai, JIMRO, Kyorin Pharmaceutical, Kyowa Hakko Kirin, Mitsubishi Tanabe Pharma, MSD, Otsuka Pharmaceutical, UCB Japan, and Zeria Pharmaceutical. H. Ito has received lecture fees from Mitsubishi Tanabe Pharma. N. Sato and T. Yoshinari are employees of Mitsubishi Tanabe Pharma. Y. Suzuki has received lecture fees from Mitsubishi Tanabe Pharma. T. Matsumoto has received grant/research support from Asahi Kasei Medical, Ajinomoto Pharmaceuticals, Astellas Pharma, Eisai, EN Otsuka Pharmaceutical, Kyorin Pharmaceutical, Mitsubishi Tanabe Pharma, Otsuka Pharmaceutical, Otsuka Pharmaceutical Factory, UCB Japan, and Zeria Pharmaceutical. The other authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hibi, T., Sakuraba, A., Watanabe, M. et al. C-reactive protein is an indicator of serum infliximab level in predicting loss of response in patients with Crohn’s disease. J Gastroenterol 49, 254–262 (2014). https://doi.org/10.1007/s00535-013-0807-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-013-0807-0