Abstract
Background
The present study aimed to evaluate etiology-based differences in the risk of waiting list mortality, and to compare the current Japanese transplant allocation system with the Child–Turcotte–Pugh (CTP) and the Model for End-Stage Liver Disease (MELD) scoring systems with regard to the risk of waiting list mortality in patients with primary biliary cirrhosis (PBC).
Methods
Using data derived from all adult candidates for deceased donor liver transplantation in Japan from 1997 to 2011, we assessed factors associated with waiting list mortality by the Cox proportional hazards model. The waiting list mortality risk of PBC patients was further estimated with adjustment for each scoring system.
Results
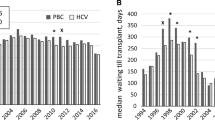
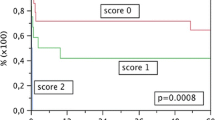
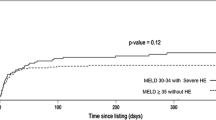
Of the 1056 patients meeting the inclusion criteria, 743 were not on the list at the end of study period; waiting list mortality was 58.1 % in this group. In multivariate analysis, increasing age and PBC were significantly associated with an increased risk of waiting list mortality. In comparison with patients with hepatitis C virus (HCV) infection, PBC patients were at 79 % increased risk and had a shorter median survival time by approximately 8 months. The relative hazard of PBC patients was statistically significant with adjustment for CTP score and medical point score, which was the priority for ranking candidates in the Japanese allocation system. However, it lost significance with adjustment for MELD score. Stratification by MELD score indicated a comparable waiting list survival time between patients with PBC and HCV.
Conclusions
PBC patients are at high risk of waiting list mortality in the current allocation system. MELD-based allocation could reduce this risk.




Similar content being viewed by others
References
OPTN/SRTR 2010 Annual Data Report. Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; 2011. Available at: http://www.srtr.org/annual_reports/2010/. Accessed 3 Sept 2012.
Dickson ER, Grambsch PM, Fleming TR, Fisher LD, Langworthy A. Prognosis in primary biliary cirrhosis: model for decision making. Hepatology. 1989;10:1–7.
Murtaugh PA, Dickson ER, Van Dam GM, Malinchoc M, Grambsch PM, Langworthy AL, et al. Primary biliary cirrhosis: prediction of short term survival based on repeated patients visits. Hepatology. 1994;20:126–34.
Dickson ER, Murtaugh PA, Wiesner RH, Grambsch PM, Fleming TR, Ludwig J, et al. Primary sclerosing cholangitis: refinement and validation of survival models. Gastroenterology. 1992;103:1893–901.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9.
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864–71.
Kamath PS, Wiesner R, Malinchoc M, Kremers W, Therneau TM, Kosbery CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–70.
Forman LM, Lucey MR. Predicting the prognosis of chronic liver disease: an evolution from Child to MELD. Mayo End-stage Liver Disease. Hepatology. 2001;33:473–5.
Said A, Williams J, Holden J, Remington P, Gangnon R, Musat A, et al. Model for end-stage liver disease score predicts mortality across a broad spectrum of liver disease. J Hepatol. 2004;40:897–903.
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–6.
Organ distribution: allocation of livers. Available at: http://optn.transplant.hrsa.gov/PoliciesandBylaws2/policies/pdfs/policy_8.pdf. Accessed 3 Sept 2012.
Murray KF, Carithers RI Jr. AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology. 2005;41:1–26.
Japan Organ Transplant Network. Available at: http://www.jotnw.or.jp/datafile/index.html in Japanese. Accessed 3 Sept 2012.
Poupon RE, Poupon R, Balkau B. Ursodiol for the long-term treatment of primary biliary cirrhosis. The UDCA-PBC study group. N Engl J Med. 1994;330:1342–7.
Corpechot C, Carrat F, Bonnand AM, Poupon RE, Poupon R. The effect of ursodeoxycholic acid therapy on liver fibrosis progression in primary biliary cirrhosis. Hepatology. 2000;32:1196–9.
Corpechot C, Carrat F, Bahr A, Chretien Y, Poupon RE, Poupon R. The effect of ursodeoxycholic acid therapy on the natural course of primary biliary cirrhosis. Gastroenterology. 2005;128:297–303.
Corpechot C, Abenavoli L, Rabahi N, Chretien Y, Andreani T, Johanet C, et al. Biochemical response to ursodeoxycholic acid and long-term prognosis in primary biliary cirrhosis. Hepatology. 2008;48:871–7.
Markus BH, Dickinson E, Grambsh P, Fleming TR, Mazzaferro V, Klintmalm GB, et al. Efficacy of liver transplantation in patients with primary biliary cirrhosis. N Engl J Med. 1989;320:1709–13.
Kim WR, Wiesner RH, Therneau TM, Poterucha JJ, Porayko MK, Evans RW, et al. Optimal timing of liver transplantation for primary biliary cirrhosis. Hepatology. 1998;28:33–8.
Acknowledgments
This study was supported by a Health Labor Sciences Research Grant, Research on Measures for Intractable Diseases, from the Ministry of Health, Labor and Welfare of Japan.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The Assessment Committee of Indication for Transplantation: T. Ichida, S. Sakisaka, M. Sata, E. Tanaka, A. Inui, H. Egawa, K. Umeshita, H. Furukawa, S. Kawasaki, Y. Inomata.
Rights and permissions
About this article
Cite this article
Genda, T., Ichida, T., Sakisaka, S. et al. Waiting list mortality of patients with primary biliary cirrhosis in the Japanese transplant allocation system. J Gastroenterol 49, 324–331 (2014). https://doi.org/10.1007/s00535-013-0782-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-013-0782-5