Abstract
Background
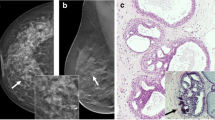
A mural nodule is a strong predictive factor for malignancy in branch duct intraductal papillary mucinous neoplasm (IPMN) of the pancreas, but the nodule size has hardly been considered. The aim of this study was to investigate whether a mural nodule of 10 mm was appropriate as an indicator of surgery for IPMN during follow-up.
Methods
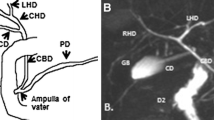
The follow-up outcomes of 100 patients who had branch duct IPMN without mural nodules or who had branch duct IPMN with mural nodules of less than 9 mm in a tertiary care setting were investigated retrospectively. The patients underwent abdominal ultrasound (US) every 3 months and additional imaging examinations or cytologic examination of pancreatic juice when necessary. Surgery was recommended to them when a mural nodule developed or when a nodule enlarged and reached 10 mm.
Results
During an average follow-up period of 97 months, branch duct IPMNs developed mural nodules that reached 10 mm in 5 patients (0.62% per year). In one patient the IPMN was revealed to be non-invasive carcinoma by resection, 1 IPMN was shown to be malignant by further follow-up, and 3 were not resected because of refusal or the patient’s age. In 7 patients, mural nodules stayed within 9 mm. The remaining 88 patients lacked mural nodules in their branch duct IPMNs throughout the follow-up. The occurrence of invasive carcinoma around the IPMN was not indicated by imaging examinations in any patient. Univariate analysis showed that the size of the cyst at baseline significantly predicted the development of a mural nodule that reached 10 mm during follow-up (P = 0.05).
Conclusions
A mural nodule of 10 mm is appropriate as an indicator of surgery in the follow-up of branch duct IPMN.




Similar content being viewed by others
Abbreviations
- IPMN:
-
Intraductal papillary mucinous neoplasm
- US:
-
Ultrasound
- EUS:
-
Endoscopic ultrasound
- CT:
-
Computed tomography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- MRCP:
-
Magnetic resonance cholangiopancreatography
References
Longnecker DS, Adler G, Hruban RH, et al. Intraductal papillary mucinous neoplasms of the pancreas. In: Hamilton SR, Aaltonen LA, editors. World Health Organization classification of tumors. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press; 2000. p. 237–40.
Hruban RH, Pitman MB, Klimstra DS. Intraductal papillary mucinous neoplasm. In: AFIP Atlas of tumor pathology. Tumors of the pancreas. Washington: ARP Press; 2007. p. 75–100.
D’Angelica M, Brennan MF, Suriawinata AA, et al. Intraductal papillary mucinous neoplasms of the pancreas: an analysis of clinicopathologic features and outcome. Ann Surg. 2004;239:400–8.
Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–99.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Rodriguez JR, Salvia R, Crippa S, et al. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology. 2007;133:72–9.
Salvia R, Crippa S, Falconi M, et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut. 2007;56:1086–90.
Pelaez-Luna M, Chari ST, Smyrk TC, et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol. 2007;102:1759–64.
Tang RS, Weinberg B, Dawson DW, et al. Evaluation of the guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol. 2008;6:815–9.
Woo SM, Ryu JK, Lee SH, et al. Branch duct intraductal papillary mucinous neoplasms in a retrospective series of 190 patients. Br J Surg. 2009;96:405–11.
Sugiyama M, Izumisato Y, Abe N, et al. Predictive factors for malignancy in intraductal papillary-mucinous tumors of the pancreas. Br J Surg. 2003;90:1244–9.
Serikawa M, Sasaki T, Fujimoto Y, et al. Management of intraductal papillary-mucinous neoplasm of the pancreas: treatment strategy based on morphologic classification. J Clin Gastroenterol. 2006;40:856–62.
Fujino Y, Matsumoto I, Ueda T, et al. Proposed new score predicting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Am J Surg. 2007;194:304–7.
Schmidt CM, White PB, Waters JA, et al. Intraductal papillary mucinous neoplasms. Predictors of malignant and invasive pathology. Ann Surg. 2007;246:644–54.
Rautou PE, Levy P, Vullierme MP, et al. Morphologic changes in branch duct intraductal papillary mucinous neoplasms of the pancreas: a midterm follow-up study. Clin Gastroenterol Hepatol. 2008;6:807–14.
Nara S, Onaya H, Hiraoka N, et al. Predictive evaluation of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas: clinical, radiological, and pathological analysis of 123 cases. Pancreas. 2009;38:8–16.
Kobayashi G, Fujita N, Noda Y, et al. Mode of progression of intraductal papillary-mucinous tumor of the pancreas: analysis of patients with follow-up by EUS. J Gastroenterol. 2005;40:744–51.
Okabayashi T, Kobayashi M, Nishimori I, et al. Clinicopathological features and medical management of intraductal papillary mucinous neoplasms. J Gastroenterol Hepatol. 2006;21:462–7.
Hirono S, Tani M, Kawai M, et al. Treatment strategy for intraductal papillary mucinous neoplasm of the pancreas based on malignant predictive factors. Arch Surg. 2009;144:345–9.
Kubo H, Chijiiwa Y, Akahoshi K, et al. Intraductal papillary-mucinous tumors of the pancreas: differential diagnosis between benign and malignant tumors by endoscopic ultrasonography. Am J Gastroenterol. 2001;96:1429–34.
Choi BS, Kim TK, Kim AY, et al. Differential diagnosis of benign and malignant intraductal papillary mucinous tumors of the pancreas: MR cholangiopancreatography and MR angiography. Korean J Radiol. 2003;4:157–62.
Yamaguchi T, Shira Y, Ishihara T, et al. Pancreatic juice cytology in the diagnosis of intraductal papillary mucinous neoplasm of the pancreas. Cancer. 2005;104:2830–6.
Uehara H, Nakaizumi A, Iishi H, et al. Cytologic examination of pancreatic juice for differential diagnosis of benign and malignant mucin-producing tumors of the pancreas. Cancer. 1994;74:826–33.
Tada M, Kawabe T, Arizumi M, et al. Pancreatic cancer in patients with pancreatic cystic lesions: a prospective study in 197 patients. Clin Gastroenterol Hepatol. 2006;4:1265–70.
Ingkakul T, Sadakari Y, Ienaga J, et al. Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Ann Surg. 2010;251:70–5.
Uehara H, Nakaizumi A, Ishikawa O, et al. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut. 2008;57:1561–5.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uehara, H., Ishikawa, O., Katayama, K. et al. Size of mural nodule as an indicator of surgery for branch duct intraductal papillary mucinous neoplasm of the pancreas during follow-up. J Gastroenterol 46, 657–663 (2011). https://doi.org/10.1007/s00535-010-0343-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0343-0