Abstract
Background/purpose
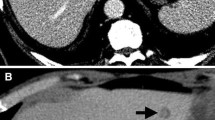
Along with advances in the chemotherapy for colorectal cancer, the strategy for hepatic metastasis has been changed. One of the most striking issues is that initially unresectable hepatic metastases can be resectable after chemotherapy with considerably high frequency. In addition, advanced chemotherapy leads to the downsizing of the metastatic foci in the liver, which is sometimes difficult to detect with conventional intraoperative ultrasonography (IOUS). To discover the undetectable hepatic lesions with IOUS, we have introduced contrast-enhanced intraoperative ultrasonography (CEIOUS). In the present study, we present evidence that viable cancer cells exist in even the shrunken tumors with high frequency and that CEIOUS contributes to detecting the minute foci.
Methods
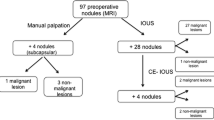
This study was composed of eight patients; four of them had initially unresectable metastasis, and the remaining four had either H2 or H3 status of hepatic metastases. All of them underwent hepatic resection after chemotherapy.
Results
A total of 57 metastatic lesions were detected before chemotherapy. Thirty lesions were demonstrated by CEIOUS with perflubutane and resected. In the pathological examination, tumor cells were not found in 12 of the 30 resected lesions. The degree of pathological liver damage was grade 1 or less in all patients, and no serious complication occurred after surgery in any of the patients.
Conclusion
The present study showed that viable cancer cells remained with high frequency, even in the minute hepatic metastasis which was reduced in size after chemotherapy, and CEIOUS was a useful examination for detecting the minute hepatic foci.





Similar content being viewed by others
References
Kerr DJ. Targeting angiogenesis in cancer: clinical development of bevacizumab. Nat Clin Pract Oncol. 2000;1:39–43.
Ellis LM. Mechanisms of action of bevacizumab as a component of therapy for metastatic colorectal cancer. Semin Oncol. 2006;33(Suppl 10):S1–7.
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–42.
Cassidy J, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A, Wong R, et al. XELOX vs FOLFOX-4 as first-line therapy for metastatic colorectal cancer: NO16966 updated results. Br J Cancer. 2011;105:58–64.
Van Cutsem E, Rivera F, Berry S, Kretzschmar A, Michael M, DiBartolomeo M, et al. Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: the BEAT study. Ann Oncol. 2009;20:1842–7.
Nuzzo G, Giuliante F, Ardito F, Vellone M, Pozzo C, Cassano A, et al. Liver resection for primarily unresectable colorectal metastases downsized by chemotherapy. J Gastrointest Surg. 2007;11:318–24.
Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240:644–57.
Folprecht G, Grothey A, Alberts S, Raab HR, Köhne CH. Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann Oncol. 2005;16:1311–9.
Pozzo C, Basso M, Cassano A, Quirino M, Schinzari G, Trigila N, et al. Neoadjuvant treatment of unresectable liver disease with irinotecan and 5-fluorouracil plus folic acid in colorectal cancer patients. Ann Oncol. 2004;15:933–9.
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16.
Japanese Classification of Colorectal carcinoma. Japanese society of cancer of the colon and rectum. Tokyo: Kanehara-Shuppan; 2009. p. 11.
Moriyasu F, Itoh K. Efficacy of perflubutane microbubble-enhanced ultrasound in the characterization and detection of focal liver lesions: phase 3 multicenter clinical trial. AJR Am J Roentgenol. 2009;193:86–95.
Uchikawa Y, Kitamura H, Miyagawa S. Portal blood flow via the peribiliary vascular plexus demonstrated by contrast-enhanced ultrasonography with Sonazoid. J Hepatobiliary Pancreat Sci. 2011;18:615–20.
Correas JM, Low G, Needleman L, Robbin ML, Cosgrove D, Sidhu PS, et al. Contrast enhanced ultrasound in the detection of liver metastases: a prospective multi-centre dose testing study using a perfluorobutane microbubble contrast agent (NC100100). J Ultrasound Med. 2011;30:441–53.
Uchiyama K, Ueno M, Ozawa S, Kiriyama S, Shigekawa Y, Yamaue H, et al. Combined use of contrast-enhanced intraoperative ultrasonography and a fluorescence navigation system for identifying hepatic metastases. World J Surg. 2010;34:2953–959.
Nakano H, Ishida Y, Hatakeyama T, Sakuraba K, Hayashi M, Sakurai O, et al. Contrast-enhanced intraoperative ultrasonography equipped with late Kupffer-phase image obtained by Sonazoid in patients with colorectal liver metastases. World J Gastroenterol. 2008;14:3207–11.
Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotheraphy: a model to predict long-term survival. Ann Surg. 2004;240:644–57.
Klinger M, Tamandl D, Eipeldauer S, Hacker S, Herberger B, Kaczirek K, et al. Bevacizumab improves pathological response of colorectal cancer liver metastases treated with XELOX/FOLFOX. Ann Surg Oncol. 2010;17:2059–65.
Ribero D, Wang H, Donadon M, Zorzi D, Thomas MB, Eng C. Bevacizumab improves pathologic response and protects against hepatic injury in patients treated with oxaliplatin-based chemotherapy for colorectal liver metastases. Cancer. 2007;110:2761–7.
Blazer DG 3rd, Kishi Y, Maru DM, Kopetz S, Chun YS, Overman MJ. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008;26:5344–51.
Duffy A, Shia J, Huitzil-Melendez FD, Fong Y, O’Reilly EM. Pathologic complete response to neoadjuvant FOLFOX in combination with bevacizumab in unresectable metastatic colorectal carcinoma. Clin Colorectal Cancer. 2008;7:140–3.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Uetake, H., Tanaka, S., Ishikawa, T. et al. Fate of metastatic foci after chemotherapy and usefulness of contrast-enhanced intraoperative ultrasonography to detect minute hepatic lesions. J Hepatobiliary Pancreat Sci 19, 509–514 (2012). https://doi.org/10.1007/s00534-012-0510-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-012-0510-1