Abstract
Background
The position of the catheter tip of totally implantable venous access devices (TIVAD) is a risk factor for postoperative complications. The study aim was to assess the early and late complications (EC and LC) associated with the position of the catheter tip in cancer patients.
Methods
We reviewed cancer patients who had a TIVAD placed in 2020. EC (≤ 90 days), LC (> 90 days) and risk factors for TIVAD-associated complications were assessed. The vertical mismatch of the catheter tip was compared to an “ideal position” (> 10 mm below the carina and ≥ 20 mm below the right main bronchus (RMB)) using chest x-ray, post-implantation.
Results
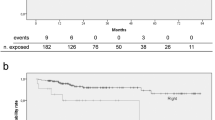
301 patients were included. Median follow-up after TIVAD implantation was 9.4 months. All TIVAD catheters were inserted via the internal jugular vein (IJV). The mean distance between the catheter tip and the carina and the RMB was 21.3 mm and 6.63 mm respectively. In total, 11.3% patients developed EC and 5.6% had LC. An association was found between the position of the catheter tip from the carina (≤ 10 mm vs. > 10 mm) and the occurrence of EC (18.3% vs. 8.6%, p = 0.01) and for the catheter insertion side (left IJV vs. right IJV) (19.1% vs. 9.0% p = 0.02). Multivariate analysis showed that left IJV catheter insertion (OR 2.76), and a catheter tip located ≤ 10 mm below the carina (OR 2.71) are significant independent risk factors of EC.
Conclusions
TIVAD catheter tip located at ≤ 10 mm below the carina, and a left-side inserted catheter, are higher risk of EC.

Similar content being viewed by others
Data availability
The data that support the findings of this study a are available from the corresponding author, C Florin Pop (catalin.florin.pop@hubriuxelles.be), upon reasonable request.
References
Desmarias S, Christen Y, Bounameaux H (1995) Central venous catheter thrombosis: prevention and treatment. Sang Thrombose Vaisseaux 7:523–528
Schutz JC, Patel AA, Clark TW, Solomon JA, Freiman DB, Tuite CM, Mondschein JI, Soulen MC, Shlansky-Goldberg RD, Stavropoulos SW, Kwak A, Chittams JL, Trerotola SO (2004) Relationship between chest port catheter tip position and port malfunction after interventional radiologic placement. J Vasc Interv Radiol : JVIR 15(6):581–587. https://doi.org/10.1097/01.rvi.0000127890.47187.91
Saber W, Moua T, Williams EC, Verso M, Agnelli G, Couban S, Young A, De Cicco M, Biffi R, van Rooden CJ, Huisman MV, Fagnani D, Cimminiello C, Moia M, Magagnoli M, Povoski SP, Malak SF, Lee AY (2011) Risk factors for catheter-related thrombosis (CRT) in cancer patients: a patient-level data (IPD) meta-analysis of clinical trials and prospective studies. J Thromb Haemost : JTH 9(2):312–319. https://doi.org/10.1111/j.1538-7836.2010.04126.x
Uchida Y, Sakamoto M, Takahashi H, Matsuo Y, Funahashi H, Sasano H, Sobue K, Takeyama H (2011) Optimal prediction of the central venous catheter insertion depth on a routine chest x-ray. Nutrition (Burbank, Los Angeles County, Calif) 27(5):557–560. https://doi.org/10.1016/j.nut.2010.07.005
Vinay M, Tejesh CA (2016) Depth of insertion of right internal jugular central venous catheter: Comparison of topographic and formula methods. Saudi J Anaesth 10(3):255–258. https://doi.org/10.4103/1658-354X.174904
Manudeep AR, Manjula BP, Dinesh Kumar US (2020) Comparison of Peres’ formula and radiological landmark formula for optimal depth of insertion of right internal jugular venous catheters. Indian J Crit Care Med : peer-reviewed, official publication of Indian Society of Critical Care Medicine 24(7):527–530. https://doi.org/10.5005/jp-journals-10071-23478
Jayaraman J, Shah V (2019) Bedside prediction of the central venous catheter insertion depth - Comparison of different techniques. J Anaesthesiol Clin Pharmacol 35(2):197–201. https://doi.org/10.4103/joacp.JOACP_125_16
Albrecht K, Nave H, Breitmeier D, Panning B, Tröger HD (2004) Applied anatomy of the superior vena cava-the carina as a landmark to guide central venous catheter placement. Br J Anaesth 92(1):75–77. https://doi.org/10.1093/bja/aeh013
Goossens GA, Verbeeck G, Moons P, Sermeus W, De Wever I, Stas M (2008) Functional evaluation of conventional ‘Celsite’ venous ports versus ‘Vortex’ ports with a tangential outlet: a prospective randomised pilot study. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer 16(12):1367–1374. https://doi.org/10.1007/s00520-008-0436-y
Granziera E, Scarpa M, Ciccarese A, Filip B, Cagol M, Manfredi V, Alfieri R, Celentano C, Cappellato S, Castoro C, Meroni M (2014) Totally implantable venous access devices: retrospective analysis of different insertion techniques and predictors of complications in 796 devices implanted in a single institution. BMC Surg 14:27. https://doi.org/10.1186/1471-2482-14-27
Liberale G (2017) Totally implantable vascular access device (TIVAD) placement: a modified technique that takes post-procedure aesthetic aspects into account. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer 25(4):1137–1140. https://doi.org/10.1007/s00520-016-3503-9
Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, Cozzi E (1982) Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery 92(4):706–712
Ballard DH, Samra NS, Gifford KM, Roller R, Wolfe BM, Owings JT (2016) Distance of the internal central venous catheter tip from the right atrium is positively correlated with central venous thrombosis. Emerg Radiol 23(3):269–273. https://doi.org/10.1007/s10140-016-1393-2
Mauri D, Zafeiri G, Tsali L, Chalkidou A, Zarkavelis G, Papadaki A, Filis P, Pentheroudakis G (2018) Identification of catheter misplacement in early port CVC dysfunction. Contemp Oncol (Poznan, Poland) 22(2):129–134. https://doi.org/10.5114/wo.2018.77044
Fu JY, Wu CF, Ko PJ, Wu CY, Kao TC, Yu SY, Liu YH, Hsieh HC (2014) Analysis of chest X-ray plain film images of intravenous ports inserted via the superior vena cava. Surg Today 44(8):1513–1521. https://doi.org/10.1007/s00595-014-0893-5
Hoareau-Gruchet F, Rtail R, Sulaj H, Khirnetkina A, Reyt E, Righini CA (2009) Complications d’un dispositif intraveineux implantable pour chimiothérapie dans les cancers des voies aérodigestives supérieures [Complications after insertion of a totally implantable venous access port in patients treated with chemotherapy for head and neck squamous cell carcinoma]. Annales d’oto-laryngologie et de chirurgie cervico faciale : bulletin de la Societe d’oto-laryngologie des hopitaux de Paris 126(2):43–52. https://doi.org/10.1016/j.aorl.2009.02.005
Stas M, Mulier S, Pattyn P, Vijgen J, De Wever I (2001) Peroperative intravasal electrographic control of catheter tip position in access ports placed by venous cut-down technique. Eur J Surg Oncol : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 27(3):316–320. https://doi.org/10.1053/ejso.2000.1047
Araújo C, Silva JP, Antunes P, Fernandes JM, Dias C, Pereira H, Dias T, Fougo JL (2008) A comparative study between two central veins for the introduction of totally implantable venous access devices in 1201 cancer patients. Euro J Surg Oncol : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 34(2):222–226. https://doi.org/10.1016/j.ejso.2007.04.003
Tumay LV, Guner OS (2021) Availability of totally implantable venous access devices in cancer patients is high in the long term: a seven-year follow-up study. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer 29(7):3531–3538. https://doi.org/10.1007/s00520-020-05871-6
Voog E, Campion L, du Rusquec P, Bourgeois H, Domont J, Denis F, Emmanuel E, Dupuis O, Ganem G, Lafont C, Le Du K, Pavluc E, Pointreau Y, Roche S, Juhel-Voog L, Zinger M, Solal-Celigny P (2018) Totally implantable venous access ports: a prospective long-term study of early and late complications in adult patients with cancer. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer 26(1):81–89. https://doi.org/10.1007/s00520-017-3816-3
Caers J, Fontaine C, Vinh-Hung V, De Mey J, Ponnet G, Oost C, Lamote J, De Greve J, Van Camp B, Lacor P (2005) Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer 13(5):325–331. https://doi.org/10.1007/s00520-004-0723-1
Narducci F, Jean-Laurent M, Boulanger L, El Bédoui S, Mallet Y, Houpeau JL, Hamdani A, Penel N, Fournier C (2011) Totally implantable venous access port systems and risk factors for complications: a one-year prospective study in a cancer centre. Euro J Surg Oncol : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 37(10):913–918. https://doi.org/10.1016/j.ejso.2011.06.016
Wolosker N, Yazbek G, Nishinari K, Malavolta LC, Munia MA, Langer M, Zerati AE (2004) Totally implantable venous catheters for chemotherapy: experience in 500 patients. Sao Paulo Med J Revista paulista de medicina 122(4):147–151. https://doi.org/10.1590/s1516-31802004000400003
Vesely TM (2003) Central venous catheter tip position: a continuing controversy. J Vasc Interv Radiol : JVIR 14(5):527–534. https://doi.org/10.1097/01.rvi.0000071097.76348.72
Liu W, Han Q, Li L, Chi J, Liu X, Gu Y (2023) Catheter malposition analysis of totally implantable venous access port in breast cancer patients. Front Surg 9:1061826. https://doi.org/10.3389/fsurg.2022.1061826
Lin WY, Lin CP, Hsu CH, Lee YH, Lin YT, Hsu MC, Shao YY (2017) Right or left? Side selection for a totally implantable vascular access device: a randomised observational study. Br J Cancer 117(7):932–937. https://doi.org/10.1038/bjc.2017.264
Smith T, Kaufman C, Quencer K (2022) Internal jugular central venous catheter tip migration: Patient and procedural factors. Tomography (Ann Arbor, Mich) 8(2):1033–1040. https://doi.org/10.3390/tomography8020083
Acknowledgements
The authors would like to acknowledge the contribution of a medical writer, Sandy Field, PhD, for English language editing and formatting of this manuscript.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: GL, HH, and CFP.
Management of data: HH, CFP, and MM.
Formal analysis: HH, CFP, MV and MM.
Contributed to resources: SM, CFP, CK, CD, MV and GL.
Project administration: GL.
Methodology: GL, CFP, MV, and MM.
Visualization and data presentation: HH, CFP, MM, CD, and GL.
Supervision: CFP, MM and GL.
Original draft preparation: HH and CFP.
Writing, review and editing the paper: HH, CFP, CK, CD, SM, MM, MV and GL.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics committee at the Jules Bordet Institute – HUB on 22 February, 2022 (CE3439) and complied with the Helsinki Declaration.
Human ethics and consent to participate declarations
Not applicable.
Competing interests
The authors have no competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hamri, H., Pop, C.F., Mauriac, S. et al. Evaluation of the position of the central venous catheter tip of implantable venous access devices in the occurrence of postoperative thrombotic and non-thrombotic complications. Support Care Cancer 32, 355 (2024). https://doi.org/10.1007/s00520-024-08563-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08563-7