Abstract
Objective
Our understanding of the experiences of prostate cancer survivors regarding their sexual life and related issues remains limited. Therefore, this study aimed to explore sexual dysfunction and associated coping strategies among Iranian prostate cancer survivors.
Methods
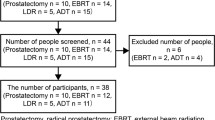
A qualitative study was undertaken. Participants were 15 Iranian prostate cancer survivors chosen using purposeful sampling. Data collection involved conducting in-depth semi-structured interviews, followed by the utilization of the conventional qualitative content analysis method for data analysis.
Results
Three themes were developed: (a) suspension of sexual life—treatment for prostate cancer significantly impacted participants’ sexual lives; (b) emotional resilience and psychological coping strategies—various psychological strategies were used to tackle sexual dysfunction; (c) efforts to regain sexual function—several strategies were applied to enhance sexual performance.
Conclusion
Our study findings provide insights into the experiences of prostate cancer survivors and subsequent shifts in their sexual dynamics and coping with the disease. Healthcare providers should actively identify patients’ concerns and develop culturally tailored care strategies to address sexual challenges and improve coping among prostate cancer survivors.
Similar content being viewed by others
Data availability
The interview transcripts will not be made publicly available to maintain the confidentiality of the data provided by the participants.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
World Health Organization (2018) International agency for research on cancer. Global cancer observatory. Available online: https://gco.iarc.fr/. Accessed 15 Oct 2020
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics, 2021. CA Cancer J Clin 71(1):7–33
Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C, Walsh E et al (2016) Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N Engl J Med 375(15):1425–1437
Nicolai M, Urkmez A, Sarikaya S, Fode M, Falcone M, Albersen M et al (2021) Penile rehabilitation and treatment options for erectile dysfunction following radical prostatectomy and radiotherapy: a systematic review. Front surg 8:636974
Edmunds K, Tuffaha H, Galvão DA, Scuffham P, Newton RU (2020) Incidence of the adverse effects of androgen deprivation therapy for prostate cancer: a systematic literature review. Support Care Cancer 28(5):2079–2093
Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F et al (2010) Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol 57(5):804–814
Chung E (2021) Male sexual dysfunction and rehabilitation strategies in the settings of salvage prostate cancer treatment. Int J Impot Res 33(4):457–463
Ilie G, Rutledge R, Sweeney E (2020) Anxiety and depression symptoms in adult males in Atlantic Canada with or without a lifetime history of prostate cancer. Psychooncology 29(2):280–286
Vyas N, Brunckhorst O, Fox L, Van Hemelrijck M, Muir G, Stewart R et al (2022) Undergoing radical treatment for prostate cancer and its impact on wellbeing: a qualitative study exploring men’s experiences. PLoS ONE 17(12):e0279250
Martin Hald G, Dahl Pind M, Borre M, Lange T (2018) Scandinavian prostate cancer patients’ sexual problems and satisfaction with their sex life following anti-cancer treatment. Sexual medicine 6(3):210–216
Wassersug RJ, Westle A, Dowsett GW (2017) Men’s sexual and relational adaptations to erectile dysfunction after prostate cancer treatment. Int J Sex Health 29(1):69–79
Bowie J, Brunckhorst O, Stewart R, Dasgupta P, Ahmed K (2022) Body image, self-esteem, and sense of masculinity in patients with prostate cancer: a qualitative meta-synthesis. J Cancer Surviv 16(1):95–110
Watson E, Wilding S, Matheson L, Brett J, McCaughan E, Downing A et al (2021) Experiences of support for sexual dysfunction in men with prostate cancer: findings from a UK-wide mixed methods study. J Sex Med 18(3):515–525
Nguyen D-D, Berlin A, Matthew AG, Perlis N, Elterman DS (2021) Sexual function and rehabilitation after radiation therapy for prostate cancer: a review. Int J Impot Res 33(4):410–417
Mardani A, Pedram Razi S, Mazaheri R, Haghani S, Vaismoradi M (2021) Effect of the exercise programme on the quality of life of prostate cancer survivors: a randomized controlled trial. Int J Nurs Pract 27(2):e12883
Mardani A, Razi SP, Mazaheri R, Dianatinasab M, Vaismoradi M (2020) Health-related quality of life in prostate cancer survivors: implications for nursing care. Int J Caring Sci 13(2):1322
Maleki M, Mardani A, Ghafourifard M, Vaismoradi M (2022) Changes and challenges in sexual life experienced by the husbands of women with breast cancer: a qualitative study. BMC Womens Health 22(1):326
Mardani-Hamooleh M, Heidari H (2017) Perception of Iranian patients with cancer regarding sexual health: a content analysis study. Sex Disabil 35:119–129
Vaismoradi M, Turunen H, Bondas T (2013) Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci 15(3):398–405
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357
Graneheim UH, Lundman B (2004) Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24(2):105–112
Thomas E, Magilvy JK (2011) Qualitative rigor or research validity in qualitative research. J Spec Pediatr Nurs 16(2):151–155
Green R (2021) Maintaining masculinity: moral positioning when accounting for prostate cancer illness. Health 25(4):399–416
Wang T, Cheng H-L, Wong PKK, Dong W (2022) Men’s experiences of sex and intimacy after prostate cancer treatment in China: a qualitative study. Support Care Cancer 30(4):3085–3092
Araújo JS, Conceição VMd, Zago MMF (2019) Transitory masculinities in the context of being sick with prostate cancer. Rev Lat Am Enfermagem 27:e3224
Maasoumi R, Taket A, Zarei F (2018) How Iranian women conceptualize the role of cultural norms in their sexual lives. Sex Cult 22:1376–1390
Evans J, Frank B, Oliffe JL, Gregory D (2011) Health, illness, men and masculinities (HIMM): a theoretical framework for understanding men and their health. J Men’s Health 8(1):7–15
Hayashi S, Oishi F, Sato K, Fukuda H, Ando S (2022) Sexual dysfunction associated with prostate cancer treatment in Japanese men: a qualitative research. Support Care Cancer 30(4):3201–3213
Chien CH, Pang ST, Chuang CK, Liu KL, Wu CT, Yu KJ et al (2022) Exploring psychological resilience and demoralisation in prostate cancer survivors. Eur J Cancer Care 31(6):e13759
McSorley O, McCaughan E, Prue G, Parahoo K, Bunting B, O’Sullivan J (2014) A longitudinal study of coping strategies in men receiving radiotherapy and neo-adjuvant androgen deprivation for prostate cancer: a quantitative and qualitative study. J Adv Nurs 70(3):625–638
Appleton L, Wyatt D, Perkins E, Parker C, Crane J, Jones A et al (2015) The impact of prostate cancer on men’s everyday life. Eur J Cancer Care 24(1):71–84
Chambers SK, Hyde MK, Laurie K, Legg M, Frydenberg M, Davis ID et al (2018) Experiences of Australian men diagnosed with advanced prostate cancer: a qualitative study. BMJ Open 8(2):e019917
Prashar J, Schartau P, Murray E (2022) Supportive care needs of men with prostate cancer: a systematic review update. Eur J Cancer Care 31(2):e13541
Buote R, Cameron E, Collins R, McGowan E (2020) Understanding men’s experiences with prostate cancer stigma: a qualitative study. Oncol Nurs Forum 47(5):577–585
Nelson CJ, Lacey S, Kenowitz J, Pessin H, Shuk E, Roth AJ et al (2015) Men’s experience with penile rehabilitation following radical prostatectomy: a qualitative study with the goal of informing a therapeutic intervention. Psychooncology 24(12):1646–1654
Pinks D, Davis C, Pinks C (2018) Experiences of partners of prostate cancer survivors: a qualitative study. J Psychosoc Oncol 36(1):49–63
Acknowledgements
The authors extend their gratitude to the participants who generously shared their valuable experiences and dedicated their time to contribute to this study.
Funding
This work was supported by the Iran University of Medical Sciences (grant number: 14011–3-23049).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. AM, AK, and MAF performed material preparation, data collection, and analysis. AM, MM, and MV wrote the first draft of the manuscript, and all authors commented on previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics committees of the Iran University of Medical Sciences (decree number: IR.IUMS.REC.1401.160).
Consent to participate
Informed consent was obtained from all participants.
Consent for publication
All participants consented to the research and subsequent publications.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mardani, A., Farahani, M.A., Khachian, A. et al. Qualitative exploration of sexual dysfunction and associated coping strategies among Iranian prostate cancer survivors. Support Care Cancer 32, 360 (2024). https://doi.org/10.1007/s00520-024-08548-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08548-6



