Abstract
Objectives
Evaluate the relationship between psychological distress, namely anxiety and depression, with urinary continence and recovery of erectile function in patients undergoing radical prostatectomy (RP).
Methods
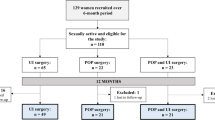
We retrospectively analyzed data from 33 consecutive patients who underwent RP in a single tertiary-referral academy between 01/2018 to 01/2019. We used the International Index of Erectile Function (IIEF-15), the Sexual Complaints Screener for Men (SCS-M), and the Hospital Anxiety and Depression Scale (HADS), validated questionnaires for the assessment of sexual function, anxiety, and depression experiences, respectively. These questionnaires were administered at the pre-surgical visit, after surgery, and at intermediate follow-ups (three, six, and twelve months).
Results
The analysis of the questionnaires completed during follow-up shows that erectile function is the most affected, with 90% erectile dysfunction (ED) at three months after surgery. In terms of emotional states, anxiety prevails in the first months following surgery and is statistically significantly associated with incontinence (p = 0.02). Depressive symptoms, on the other hand, appear later and prevail over anxiety at six months after surgery, although not statistically significant.
Conclusions
In the early post-surgical phase anxiety and ED are the most frequently detected components, while depressive experiences and decreased desire, typical of later stages, have not yet fully emerged.
Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Drabe N, Steinert H, Moergeli H, Weidt S, Strobel K, Jenewein J (2016) Perception of treatment burden, psychological distress, and fatigue in thyroid cancer patients and their partners - effects of gender, role, and time since diagnosis. Psychooncology 25(2):203–209. https://doi.org/10.1002/pon.3903
Pérez-Fortis A, Schroevers MJ, Fleer J, Alanís-López P, Veloz-Martínez MG, Ornelas Mejorada RE, Sanderman R, Ranchor AV, Sánchez Sosa JJ (2017) Psychological burden at the time of diagnosis among Mexican breast cancer patients. Psycho-Oncology 26:133–136. https://doi.org/10.1002/pon.4098
Koo K et al (2017) The burden of cystoscopic bladder cancer surveillance: anxiety, discomfort, and patient preferences for decision making. Urology 108:122–128. https://doi.org/10.1016/j.urology.2017.07.016
Kumar S, Kumar K, Singh B, Mehrotra D, Mahdi AA (2023) Association of salivary cortisol and psychological burden in patients with oral cancer and oral potentially malignant disorders: A prospective study. J Cancer Res Ther 19(Supplement):S0. https://doi.org/10.4103/jcrt.jcrt_530_22
Gould MK et al (2023) Emotional distress, anxiety, and general health status in patients with small pulmonary nodules shortly after their identification: results from the watch the spot trial. Chest. https://doi.org/10.1016/j.chest.2023.06.022
Thekdi SM et al (2015) Posttraumatic stress and depressive symptoms in renal cell carcinoma: association with quality of life and utility of single-item distress screening. Psychooncology 24(11):1477–1484. https://doi.org/10.1002/pon.3758
Barros R, Favorito LA, Nahar B, Almeida R, Ramasamy R (2023) Changes in male sexuality after urologic cancer: a narrative review. Int brazilian J Urol 49(2):175–183. https://doi.org/10.1590/S1677-5538.IBJU.2023.9901
Rossi MS et al (2016) Erectile function recovery after nerve-sparing radical prostatectomy for prostate cancer: is back to baseline status enough for patient satisfaction? J Sex Med 13(4):669–678. https://doi.org/10.1016/j.jsxm.2016.02.160
van der Poel HG, de Blok W (2009) Role of extent of fascia preservation and erectile function after robot-assisted laparoscopic prostatectomy. Urology 73(4):816–821. https://doi.org/10.1016/j.urology.2008.09.082
Martin Hald G, Dahl Pind M, Borre M, Lange T (2018) Scandinavian prostate cancer patients’ sexual problems and satisfaction with their sex life following anti-cancer treatment. Sex Med 6(3):210–216. https://doi.org/10.1016/j.esxm.2018.06.002
Terrier JE, Masterson M, Mulhall JP, Nelson CJ (2018) Decrease in Intercourse Satisfaction in Men Who Recover Erections After Radical Prostatectomy. J Sex Med 15(8):1133–1139. https://doi.org/10.1016/j.jsxm.2018.05.020
Rapoport L et al (2018) Radical prostatectomy performed via robotic, transperitoneal and extraperitoneoscopic approaches: Functional and early oncological outcomes. Cent Eur J Urol 71(4):378–385. https://doi.org/10.5173/ceju.2018.1739
Kadono Y, Nohara T, Kawaguchi S, Iwamoto H, Yaegashi H, Shigehara K, Izumi K, Mizokami A (2022) Impact of pelvic anatomical changes caused by radical prostatectomy. Cancers 14(13):3050. https://doi.org/10.3390/cancers14133050
Kretschmer A et al (2020) Health-related quality of life after open and robot-assisted radical prostatectomy in low- and intermediate-risk prostate cancer patients: a propensity score-matched analysis. World J Urol 38:3075–3083. https://doi.org/10.1007/s00345-020-03144-9
Nelson CJ, Mulhall JP, Roth AJ (2011) The association between erectile dysfunction and depressive symptoms in men treated for prostate cancer. J Sex Med 8(2):560–566. https://doi.org/10.1111/j.1743-6109.2010.02127.x
Liss MA et al (2010) Continence definition after radical prostatectomy using urinary quality of life: evaluation of patient reported validated questionnaires. J Urol 183(4):1464–1468. https://doi.org/10.1016/j.juro.2009.12.009
Hatzichristou D et al (2010) Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med 7(1_part_2):337–348. https://doi.org/10.1111/j.1743-6109.2009.01619.x
Cappelleri JC et al (1999) Some developments on the international index of erectile function (IIEF). Ther Innov Regul Sci 33(1):179–190. https://doi.org/10.1177/009286159903300122
Vedana L et al (2002) Clinical validation of an anxiety and depression screening test for intensive in-hospital rehabilitation. Monaldi Arch Chest Dis = Arch Monaldi Per Le Mal Del Torace 58(2):101–106
N IBM Corp (2017) IBM SPSS statistics for windows. Version 25.0. IBM corp Armonk, NY
Haglind E et al (2015) Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol 68(2):216–225. https://doi.org/10.1016/j.eururo.2015.02.029
Ficarra V et al (2012) Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 62(3):405–417. https://doi.org/10.1016/j.eururo.2012.05.045
Holze S et al (2019) Comparison of various continence definitions in a large group of patients undergoing radical prostatectomy: a multicentre, prospective study. BMC Urol 19(1):70. https://doi.org/10.1186/s12894-019-0500-6
Smith WJ, VanDyke ME, Venishetty N, Langford BT, Franzen BP, Morey AF (2023) Surgical management of male stress incontinence: techniques, indications, and pearls for success. Res reports Urol 15:217–232. https://doi.org/10.2147/RRU.S395359
Bratu O et al (2017) Erectile dysfunction post-radical prostatectomy - a challenge for both patient and physician. J Med Life 10(1):13–18
Soloway CT, Soloway MS, Kim SS, Kava BR (2005) Sexual, psychological and dyadic qualities of the prostate cancer ‘couple.’ BJU Int 95:780–785. https://doi.org/10.1111/j.1464-410X.2005.05400.x
Herlemann A, Cowan JE, Carroll PR, Cooperberg MR, Catto J (2023) Community-based Outcomes of Open versus Robot-assisted Radical Prostatectomy. Eur Urol 73(2):215–223. https://doi.org/10.1016/j.eururo.2017.04.027
Popiołek A, Brzoszczyk B, Jarzemski P, Piskunowicz M, Jarzemski M, Borkowska A, Bieliński M (2022) Quality of life of prostate cancer patients undergoing prostatectomy and affective temperament. Cancer Manag Res 14:1743–1755. https://doi.org/10.2147/CMAR.S358054
Namiki S, Saito S, Tochigi T, Numata I, Ioritani N, Arai Y (2007) Psychological distress in Japanese men with localized prostate cancer. Int J Urol 14:924–929. https://doi.org/10.1111/j.1442-2042.2007.01746.x
Boeri L et al (2018) Depressive symptoms and low sexual desire after radical prostatectomy: early and long-term outcomes in a real-life setting. J Urol 199(2):474–480. https://doi.org/10.1016/j.juro.2017.08.104
Watts S et al (2014) Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 4(3):e003901. https://doi.org/10.1136/bmjopen-2013-003901
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization and Conceptualization: MT, PMM; Data curation: MT, MS, PMM; Formal analysis: MT; Funding acquisition: N/A; Investigation: MT, MS; Methodology: MT, PMM; Project administration: MT, MS, PMM; Resources and Software: MT; Supervision and Validation: PMM, MS: Visualization and Writing: LMIJ, MT.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tozzi, M., Jannello, L.M.I., Silvaggi, M. et al. Anxiety, depression, urinary continence, and sexuality in patients undergoing radical prostatectomy: preliminary findings. Support Care Cancer 32, 294 (2024). https://doi.org/10.1007/s00520-024-08503-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08503-5