Abstract
Purpose
This overview of reviews aimed to summarize the prevalence of burnout and the dimensions of burnout (emotional exhaustion, depersonalization, and personal accomplishment) in oncology professionals around the world.
Methods
The CINAHL, Embase, PsycINFO, and PubMed databases were searched from inception to September 13, 2023. AMSTAR 2 was used to assess the quality of reviews. The overlap between reviews was calculated.
Results
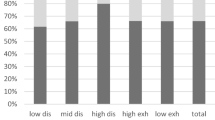
Twelve reviews were included. Overall, reviews showed that burnout was prevalent in oncologists and oncology nurses. On the other hand, no reviews meta-analyzed the prevalence of burnout in oncology radiation therapists. In addition, the dimensions of burnout, high emotional exhaustion, high depersonalization, and low personal accomplishment were highly prevalent across reviews in oncologists, oncology nurses, and oncology radiation therapists. In oncologists, the Americas (specifically Canada) showed the highest prevalence rates for high emotional exhaustion, whereas high depersonalization and low personal accomplishment were mainly prevalent in Europe and Asia, respectively. In oncology nurses, high emotional exhaustion and high depersonalization were mainly prevalent in Asia, whereas low personal accomplishment was more prevalent in the Americas (specifically Canada). The prevalence of overall levels of burnout was not meta-analyzed by continents.
Conclusion
Some methodological improvements may help to make more robust the findings of this overview (e.g., specific subgroup meta-analyses by oncology specialties), which may help readers reach more precise, direct, and consistent findings.
Protocol registration







Similar content being viewed by others
Data availability
All data relevant to the study are included in the article or are available as supplementary files.
References
Ghahramani S, Lankarani KB, Yousefi M et al (2021) A systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front Psychiatry 12:758849. https://doi.org/10.3389/fpsyt.2021.758849
Guseva Canu I, Marca SC, Dell’Oro F et al (2021) Harmonized definition of occupational burnout: a systematic review, semantic analysis, and Delphi consensus in 29 countries. Scand J Work Environ Health 47:95–107. https://doi.org/10.5271/sjweh.3935
Maslach C, Jackson SE, Leiter MP (1997) Maslach Burnout Inventory: third edition. In: Zalaquett CP, Wood RJ (eds) Evaluating stress: A book of resources. Scarecrow Education, pp 191–218
Kristensen TS, Borritz M, Villadsen E, Christensen KB (2005) The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress 19:192–207. https://doi.org/10.1080/02678370500297720
Stamm BH. The concise ProQOL manual 2010. Available from: https://proqol.org/. Accessed 01/10/2023
Al-Gobari M, Shoman Y, Blanc S, Canu IG (2022) Point prevalence of burnout in Switzerland: a systematic review and meta-analysis. Swiss Med Wkly 152:w30229. https://doi.org/10.4414/smw.2022.w30229
Arigoni F, Bovier PA, Sappino AP (2010) Trend of burnout among Swiss doctors. Swiss Med Wkly 140:w13070. https://doi.org/10.4414/smw.2010.13070
Ge M, Hu F, Jia Y et al (2023) Global prevalence of nursing burnout syndrome and temporal trends for the last 10 years: a meta-analysis of 94 studies covering over 30 countries. J Clin Nurs 32:5836–5854. https://doi.org/10.1111/jocn.16708
Guerra J, Patrício M (2019) Burnout in radiation therapists: systematic review with meta-analysis. Eur J Cancer Care (Engl) 28:e12938. https://doi.org/10.1111/ecc.12938
HaGani N, Yagil D, Cohen M (2022) Burnout among oncologists and oncology nurses: a systematic review and meta-analysis. Health Psychol 41:53–64. https://doi.org/10.1037/hea0001155
Balch CM, Shanafelt TD, Sloan J et al (2011) Burnout and career satisfaction among surgical oncologists compared with other surgical specialties. Ann Surg Oncol 18:16–25. https://doi.org/10.1245/s10434-010-1369-5
Cass I, Duska LR, Blank SV et al (2016) Stress and burnout among gynecologic oncologists: a Society Of Gynecologic Oncology evidence-based review and recommendations. Gynecol Oncol 143:421–427. https://doi.org/10.1016/j.ygyno.2016.08.319
Beltràn Ponce S, Small CJ, Amini A et al (2023) Overcoming burnout and promoting wellness in radiation oncology: a report from the ACR Commission on radiation oncology. J Am Coll Radiol JACR 20:487–493. https://doi.org/10.1016/j.jacr.2023.03.003
Rath KS, Huffman LB, Phillips GS et al (2015) Burnout and associated factors among members of the Society of Gynecologic Oncology. Am J Obstet Gynecol 213:824.e1–9. https://doi.org/10.1016/j.ajog.2015.07.036
Murali K, Makker V, Lynch J, Banerjee S (2018) From burnout to resilience: an update for oncologists. Am Soc Clin Oncol Educ Book Am Soc Clin Oncol Annu Meet 38:862–872. https://doi.org/10.1200/EDBK_201023
Doraiswamy S, Chaabna K, Jithesh A et al (2021) Physician burnout in the Eastern Mediterranean region: influence of gender and related factors - systematic review and meta-analysis. J Glob Health 11:1–15. https://doi.org/10.7189/jogh.11.04043
Yates M, Samuel V (2019) Burnout in oncologists and associated factors: a systematic literature review and meta-analysis. Eur J Cancer Care (Engl) 28:e13094. https://doi.org/10.1111/ecc.13094
Xie W, Wang J, Zhang Y et al (2021) The levels, prevalence and related factors of compassion fatigue among oncology nurses: a systematic review and meta-analysis. J Clin Nurs 30:615–632. https://doi.org/10.1111/jocn.15565
Cañadas-De la Fuente GA, Gómez-Urquiza JL, Ortega-Campos EM et al (2018) Prevalence of burnout syndrome in oncology nursing: a meta-analytic study. Psychooncology 27:1426–1433. https://doi.org/10.1002/pon.4632
Gates M, Gates A, Pieper D et al (2022) Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ 378:e070849. https://doi.org/10.1136/bmj-2022-070849
Beller EM, Glasziou PP, Altman DG et al (2013) PRISMA for Abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med 10:e1001419. https://doi.org/10.1371/journal.pmed.1001419
Morgan RL, Whaley P, Thayer KA, Schünemann HJ (2018) Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int 121:1027–1031. https://doi.org/10.1016/j.envint.2018.07.015
Kwon Y, Lemieux M, McTavish JWN (2015) Identifying and removing duplicate records from systematic review searches. J Med Libr Assoc 103:184–188
Shea BJ, Reeves BC, Wells G et al (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:1–9. https://doi.org/10.1136/bmj.j4008
Pieper D, Antoine SL, Mathes T et al (2014) Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol 67:368–375. https://doi.org/10.1016/j.jclinepi.2013.11.007
Low ZX, Yeo KA, Sharma VK et al (2019) Prevalence of burnout in medical and surgical residents: a meta-analysis. Int J Environ Res Public Health 16:1479. https://doi.org/10.3390/ijerph16091479
Medisauskaite A, Kamau C (2017) Prevalence of oncologists in distress: systematic review and meta-analysis. Psychooncology 26:1732–1740. https://doi.org/10.1002/pon.4382
Algamdi M (2022) Prevalence of oncology nurses’ compassion satisfaction and compassion fatigue: Systematic review and meta-analysis. Nurs Open 9:44–56. https://doi.org/10.1002/nop2.1070
De la Fuente-Solana EI, Pradas-Hernández L, Ramiro-Salmerón A et al (2020) Burnout syndrome in paediatric oncology nurses: a systematic review and meta-analysis. Healthc Basel Switz 8:309. https://doi.org/10.3390/healthcare8030309
Ma Y, Xie T, Zhang J, Yang H (2023) The prevalence, related factors and interventions of oncology nurses’ burnout in different continents: a systematic review and meta-analysis. J Clin Nurs 32:7050–7061. https://doi.org/10.1111/jocn.16838
Hlubocky FJ, Shanafelt TD, Back AL et al (2021) Creating a blueprint of well-being in oncology: an approach for addressing burnout from ASCO’s clinician well-being taskforce. Am Soc Clin Oncol Educ Book 41:e339–e353. https://doi.org/10.1200/EDBK_320873
Alabi RO, Hietanen P, Elmusrati M et al (2021) Mitigating burnout in an oncological unit: a scoping review. Front Public Health 9:677915. https://doi.org/10.3389/fpubh.2021.677915
Schünemann H, Brożek J, Guyatt G, Oxman A, editors. (2013) GRADE handbook for grading quality of evidence and strength of recommendations. The GRADE Working Group. Available from: https://gdt.gradepro.org/app/handbook/handbook.html. Accessed 02/10/2023
Borges Migliavaca C, Stein C, Colpani V et al (2020) How are systematic reviews of prevalence conducted? A methodological study. BMC Med Res Methodol 20:96. https://doi.org/10.1186/s12874-020-00975-3
Migliavaca CB, Stein C, Colpani V et al (2020) Quality assessment of prevalence studies: a systematic review. J Clin Epidemiol 127:59–68. https://doi.org/10.1016/j.jclinepi.2020.06.039
Heritage B, Rees CS, Hegney DG (2018) The ProQOL-21: a revised version of the Professional Quality of Life (ProQOL) scale based on Rasch analysis. PLoS ONE 13:e0193478. https://doi.org/10.1371/journal.pone.0193478
Li T, Higgins JPT, Deeks JJ Chapter 5: Collecting data. In: Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V, editor(s). Available from https://training.cochrane.org/handbook/current/chapter-05. Accessed 02/10/2023
Author information
Authors and Affiliations
Contributions
Conceptualization: JMC, data curation: JMC, formal analysis: all authors, funding acquisition: not applicable, investigation: not applicable, methodology: all authors, project administration: JMC, resources: not applicable, software: CGM, supervision: JMC, validation: not applicable, visualization: not applicable, writing—original draft: JMC, writing—review and editing: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient involvement
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martinez-Calderon, J., Infante-Cano, M., Casuso-Holgado, M.J. et al. The prevalence of burnout in oncology professionals: an overview of systematic reviews with meta-analyses including more than 90 distinct studies. Support Care Cancer 32, 196 (2024). https://doi.org/10.1007/s00520-024-08400-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08400-x