Abstract
Purpose
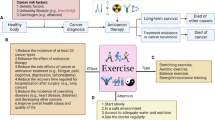
Growing recognition of the gut microbiome as an influential modulator of cancer treatment efficacy and toxicity has led to the emergence of clinical interventions targeting the microbiome to enhance cancer and health outcomes. The highly modifiable nature of microbiota to endogenous, exogenous, and environmental inputs enables interventions to promote resilience of the gut microbiome that have rapid effects on host health, or response to cancer treatment. While diet, probiotics, and faecal microbiota transplant are primary avenues of therapy focused on restoring or protecting gut function in people undergoing cancer treatment, the role of physical activity and exercise has scarcely been examined in this population.
Methods
A narrative review was conducted to explore the nexus between cancer care and the gut microbiome in the context of physical activity and exercise as a widely available and clinically effective supportive care strategy used by cancer survivors.
Results
Exercise can facilitate a more diverse gut microbiome and functional metabolome in humans; however, most physical activity and exercise studies have been conducted in healthy or athletic populations, primarily using aerobic exercise modalities. A scarcity of exercise and microbiome studies in cancer exists.
Conclusions
Exercise remains an attractive avenue to promote microbiome health in cancer survivors. Future research should elucidate the various influences of exercise modalities, intensities, frequencies, durations, and volumes to explore dose-response relationships between exercise and the gut microbiome among cancer survivors, as well as multifaceted approaches (such as diet and probiotics), and examine the influences of exercise on the gut microbiome and associated symptom burden prior to, during, and following cancer treatment.


Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM et al (2019) Cancer treatment and survivorship statistics. CA Cancer J Clin 69(5):363–385
Marzorati C, Riva S, Pravettoni G (2017) Who is a cancer survivor? A systematic review of published definitions. J Cancer Educ 32(2):228–237
Lai-Kwon J, Heynemann S, Hart NH, Chan RJ, Smith TJ, Nekhlyudov L et al (2023) Evolving landscape of metastatic cancer survivorship—reconsidering clinical care, policy, and research priorities for the modern era. J Clin Oncol 41(18):3304–3310
Wardill HR, Chan RJ, Chan A, Keefe D, Costello SP, Hart NH (2022) Dual contribution of the gut microbiome to immunotherapy efficacy and toxicity: supportive care implications and recommendations. Support Care Cancer 30(8):6369–6373
Sougiannis AT, VanderVeen BN, Davis JM, Fan D, Murphy EA (2021) Understanding chemotherapy-induced intestinal mucositis and strategies to improve gut resilience. Am J Physiol Gastrointest Liver Physiol 320(5):G712–G7G9
Hart NH, Crawford-Williams F, Crichton M, Yee J, Smith TJ, Koczwara B et al (2022) Unmet supportive care needs of people with advanced cancer and their caregivers: a systematic scoping review. Crit Rev Oncol Hematol 176:103728
Hart NH, Iyengar NM (2022) Chapter 8: rehabilitation in cancer — role of exercise and nutrition. In: Bošnjak SMB-SI, Mountzios G, Wood J (eds) European Society of Medical Oncology. ESMO Press, pp 196–206
Sepich-Poore GD, Zitvogel L, Straussman R, Hasty J, Wargo JA, Knight R (2021) The microbiome and human cancer. Science 371(6536):eabc4552
Yue B, Gao R, Wang Z, Dou W (2021) Microbiota-host-irinotecan axis: a new insight toward irinotecan chemotherapy. Front Cell Infect Microbiol 11:710945
Yu Z-K, Xie R-L, You R, Liu Y-P, Chen X-Y, Chen M-Y et al (2021) The role of the bacterial microbiome in the treatment of cancer. BMC Cancer 21(1):934
Subramaniam CB, Bowen JM, Gladman MA, Lustberg MB, Mayo SJ, Wardill HR (2020) The microbiota-gut-brain axis: an emerging therapeutic target in chemotherapy-induced cognitive impairment. Neurosci Biobehav Rev 116:470–479
Deleemans JM, Gajtani Z, Baydoun M, Reimer RA, Piedalue KA, Carlson LE (2021) The use of prebiotic and probiotic interventions for treating gastrointestinal and psychosocial health symptoms in cancer patients and survivors: a systematic review. Integr Cancer Ther 20:15347354211061733
Wang Z, Li L, Wang S, Wei J, Qu L, Pan L et al (2022) The role of the gut microbiota and probiotics associated with microbial metabolisms in cancer prevention and therapy. Front Pharmacol 13:1025860
Kennedy MA, Bayes S, Newton RU, Zissiadis Y, Spry NA, Taaffe DR et al (2022) Implementation barriers to integrating exercise as medicine in oncology: an ecological scoping review. J Cancer Surviv 16(4):865–881
Kennedy MA, Bayes S, Newton RU, Zissiadis Y, Spry NA, Taaffe DR et al (2020) We have the program, what now? Development of an implementation plan to bridge the research-practice gap prevalent in exercise oncology. Int J Behav Nutr Phys Act 17(1):128
Hart NH, Poprawski DM, Ashbury F, Fitch MI, Chan RJ, Newton RU et al (2022) Exercise for people with bone metastases: MASCC endorsed clinical recommendations developed by the International Bone Metastases Exercise Working Group. Support Care Cancer 30(9):7061–7065
Newton RU, Hart NH, Galvão DA, Taaffe DR, Saad F (2022) Prostate cancer treatment with exercise medicine. Trends in Urology & Men’s Health 13(6):14–19
Gustafson MP, Wheatley-Guy CM, Rosenthal AC, Gastineau DA, Katsanis E, Johnson BD et al (2021) Exercise and the immune system: taking steps to improve responses to cancer immunotherapy. J Immunother Cancer 9(7):e001872
Kim J-S, Taaffe DR, Galvão DA, Clay TD, Redfern AD, Hart NH et al (2023) Acute effect of high-intensity interval aerobic exercise on serum myokine levels and resulting tumour-suppressive effect in trained patients with advanced prostate cancer. Prostate Cancer Prostatic Dis 26(4):795–801
Kim J-S, Taaffe DR, Galvão DA, Hart NH, Gray E, Ryan CJ et al (2022) Exercise in advanced prostate cancer elevates myokine levels and suppresses in-vitro cell growth. Prostate Cancer Prostatic Dis 25(1):86–92
Farley MJ, Bartlett DB, Skinner TL, Schaumberg MA, Jenkins DG (2023) Immunomodulatory function of interleukin-15 and its role in exercise, immunotherapy, and cancer outcomes. Med Sci Sports Exerc 55(3):558–568
Deng R, Wang M, Song Y, Shi Y (2023) A bibliometric analysis on the research trend of exercise and the gut microbiome. Microorganisms. 11(4):903
Khosravi N, Stoner L, Farajivafa V, Hanson ED (2019) Exercise training, circulating cytokine levels and immune function in cancer survivors: a meta-analysis. Brain Behav Immun 81:92–104
Chan RJ, Milch VE, Crawford-Williams F, Agbejule OA, Joseph R, Johal J et al (2023) Patient navigation across the cancer care continuum: an overview of systematic reviews and emerging literature. CA Cancer J Clin 73(6):565–589
Rebersek M (2021) Gut microbiome and its role in colorectal cancer. BMC Cancer 21(1):1325
Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets TV et al (2018) Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 359(6371):97–103
Hasan N, Yang H (2019) Factors affecting the composition of the gut microbiota, and its modulation. PeerJ. 7:e7502
Scott N, Whittle E, Jeraldo P, Chia N (2022) A systemic review of the role of enterotoxic Bacteroides fragilis in colorectal cancer. Neoplasia. 29:100797
Sun CH, Li BB, Wang B, Zhao J, Zhang XY, Li TT et al (2019) The role of Fusobacterium nucleatum in colorectal cancer: from carcinogenesis to clinical management. Chronic Dis Transl Med 5(3):178–187
Yu L, Zhao G, Wang L, Zhou X, Sun J, Li X et al (2022) A systematic review of microbial markers for risk prediction of colorectal neoplasia. Br J Cancer 126(9):1318–1328
Mirzaei R, Afaghi A, Babakhani S, Sohrabi MR, Hosseini-Fard SR, Babolhavaeji K et al (2021) Role of microbiota-derived short-chain fatty acids in cancer development and prevention. Biomed Pharmacother 139:111619
Zitvogel L, Ma Y, Raoult D, Kroemer G, Gajewski TF (2018) The microbiome in cancer immunotherapy: diagnostic tools and therapeutic strategies. Science. 359(6382):1366–1370
Pouncey AL, Scott AJ, Alexander JL, Marchesi J, Kinross J (2018) Gut microbiota, chemotherapy and the host: the influence of the gut microbiota on cancer treatment. Ecancermedicalscience. 12:868
Secombe KR, Ball IA, Wignall AD, Bateman E, Keefe DM, Bowen JM (2022) Antibiotic treatment targeting gram negative bacteria prevents neratinib-induced diarrhea in rats. Neoplasia 30:100806
Wardill HR, van der Aa SAR, da Silva Ferreira AR, Havinga R, Tissing WJE, Harmsen HJM (2021) Antibiotic-induced disruption of the microbiome exacerbates chemotherapy-induced diarrhoea and can be mitigated with autologous faecal microbiota transplantation. Eur J Cancer 153:27–39
Ramakrishna C, Corleto J, Ruegger PM, Logan GD, Peacock BB, Mendonca S et al (2019) Dominant role of the gut microbiota in chemotherapy induced neuropathic pain. Sci Rep 9(1):20324
Heshiki Y, Vazquez-Uribe R, Li J, Ni Y, Quainoo S, Imamovic L et al (2020) Predictable modulation of cancer treatment outcomes by the gut microbiota. Microbiome. 8(1):28
Ervin SM, Ramanan SV, Bhatt AP (2020) Relationship between the gut microbiome and systemic chemotherapy. Dig Dis Sci 65(3):874–884
Al-Qadami GH, Secombe KR, Subramaniam CB, Wardill HR, Bowen JM (2022) Gut microbiota-derived short-chain fatty acids: impact on cancer treatment response and toxicities. Microorganisms. 10(10):2048
Bruno JS, Al-Qadami GH, Laheij A, Bossi P, Fregnani ER, Wardill HR (2023) From pathogenesis to intervention: the importance of the microbiome in oral mucositis. Int J Mol Sci 24(9):8274
Orland C, Emilson EJS, Basiliko N, Mykytczuk NCS, Gunn JM, Tanentzap AJ (2019) Microbiome functioning depends on individual and interactive effects of the environment and community structure. ISME J 13(1):1–11
Kers JG, Saccenti E (2021) The power of microbiome studies: some considerations on which alpha and beta metrics to use and how to report results. Front Microbiol 12:796025
Su X (2021) Elucidating the beta-diversity of the microbiome: from global alignment to local alignment. mSystems. 6(4):e0036321
Bruijning M, Ayroles JF, Henry LP, Koskella B, Meyer KM, Metcalf CJE (2023) Relative abundance data can misrepresent heritability of the microbiome. Microbiome. 11(1):222
Pfau M, Degregori S, Johnson G, Tennenbaum SR, Barber PH, Philson CS et al (2023) The social microbiome: gut microbiome diversity and abundance are negatively associated with sociality in a wild mammal. R Soc Open Sci 10(10):231305
Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar RD (2015) Role of the normal gut microbiota. World J Gastroenterol 21(29):8787–8803
Bokulich NA, Ziemski M, Robeson MS, Kaehler BD (2020) Measuring the microbiome: best practices for developing and benchmarking microbiomics methods. Comput Struct Biotechnol J 18:4048–4062
Montassier E, Gastinne T, Vangay P, Al-Ghalith GA, Bruley des Varannes S, Massart S et al (2015) Chemotherapy-driven dysbiosis in the intestinal microbiome. Aliment Pharmacol Ther 42(5):515–528
Secombe KR, Coller JK, Gibson RJ, Wardill HR, Bowen JM (2019) The bidirectional interaction of the gut microbiome and the innate immune system: implications for chemotherapy-induced gastrointestinal toxicity. Int J Cancer 144(10):2365–2376
Kok DE, Winkels RM, van Herpen CML, Kampman E (2018) Toxicity-induced modification of treatment: what is in a name? Eur J Cancer 104:145–150
Lyman GH (2009) Impact of chemotherapy dose intensity on cancer patient outcomes. J Natl Compr Cancer Netw 7(1):99–108
Nielson CM, Bylsma LC, Fryzek JP, Saad HA, Crawford J (2021) Relative dose intensity of chemotherapy and survival in patients with advanced stage solid tumor cancer: a systematic review and meta-analysis. Oncologist. 26(9):e1609–e1e18
Oh L, Ab Rahman S, Dubinsky K, Azanan MS, Ariffin H (2023) Manipulating the gut microbiome as a therapeutic strategy to mitigate late effects in childhood cancer survivors. Technol Cancer Res Treat 22:15330338221149799
Lu K, Dong S, Wu X, Jin R, Chen H (2021) Probiotics in cancer. Front. Oncol. 11:638148
Wardill HR, Van Sebille YZA, Ciorba MA, Bowen JM (2018) Prophylactic probiotics for cancer therapy-induced diarrhoea: a meta-analysis. Curr Opin Support Palliat Care 12(2):187–197
Wardill HR, Secombe KR, Bryant RV, Hazenberg MD, Costello SP (2019) Adjunctive fecal microbiota transplantation in supportive oncology: emerging indications and considerations in immunocompromised patients. EBioMedicine. 44:730–740
Baruch EN, Youngster I, Ben-Betzalel G, Ortenberg R, Lahat A, Katz L et al (2021) Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science. 371(6529):602–609
van Lier YF, Davids M, Haverkate NJE, de Groot PF, Donker ML, Meijer E et al (2020) Donor fecal microbiota transplantation ameliorates intestinal graft-versus-host disease in allogeneic hematopoietic cell transplant recipients. Sci Transl Med 12(556):eaaz8926
Song W, Anselmo AC, Huang L (2019) Nanotechnology intervention of the microbiome for cancer therapy. Nat Nanotechnol 14(12):1093–1103
Song M, Chan AT (2019) Environmental factors, gut microbiota, and colorectal cancer prevention. Clin Gastroenterol Hepatol 17(2):275–289
Song M, Chan AT, Sun J (2020) Influence of the gut microbiome, diet, and environment on risk of colorectal cancer. Gastroenterology. 158(2):322–340
Leeuwendaal NK, Stanton C, O’Toole PW, Beresford TP (2022) Fermented foods, health and the gut microbiome. Nutrients 14(7):1527
Fu J, Zheng Y, Gao Y, Xu W (2022) Dietary fiber intake and gut microbiota in human health. Microorganisms 10(12):2507
Cronin P, Joyce SA, O’Toole PW, O’Connor EM (2021) Dietary fibre modulates the gut microbiota. Nutrients 13(5):1655
Lin D, Peters BA, Friedlander C, Freiman HJ, Goedert JJ, Sinha R et al (2018) Association of dietary fibre intake and gut microbiota in adults. Br J Nutr 120(9):1014–1022
Lee KA, Shaw HM, Bataille V, Nathan P, Spector TD (2020) Role of the gut microbiome for cancer patients receiving immunotherapy: dietary and treatment implications. Eur J Cancer 138:149–155
Wastyk HC, Fragiadakis GK, Perelman D, Dahan D, Merrill BD, Yu FB et al (2021) Gut-microbiota-targeted diets modulate human immune status. Cell. 184(16):4137–53.e14
Withrow D, Bowers SJ, Depner CM, González A, Reynolds AC, Wright KP Jr (2021) Sleep and circadian disruption and the gut microbiome-possible links to dysregulated metabolism. Curr Opin Endocr Metab Res 17:26–37
Matenchuk BA, Mandhane PJ, Kozyrskyj AL (2020) Sleep, circadian rhythm, and gut microbiota. Sleep Med Rev 53:101340
Mailing LJ, Allen JM, Buford TW, Fields CJ, Woods JA (2019) Exercise and the gut microbiome: a review of the evidence, potential mechanisms, and implications for human health. Exerc Sport Sci Rev 47(2):75–85
Clauss M, Gérard P, Mosca A, Leclerc M (2021) Interplay between exercise and gut microbiome in the context of human health and performance. Front Nutr 8:637010
Wegierska AE, Charitos IA, Topi S, Potenza MA, Montagnani M, Santacroce L (2022) The connection between physical exercise and gut microbiota: implications for competitive sports athletes. Sports Med 52(10):2355–2369
Cronin O, O’Sullivan O, Barton W, Cotter PD, Molloy MG, Shanahan F (2017) Gut microbiota: implications for sports and exercise medicine. Br J Sports Med 51(9):700–701
Cronin O, Molloy MG, Shanahan F (2016) Exercise, fitness, and the gut. Curr Opin Gastroenterol 32(2):67–73
Jollet M, Nay K, Chopard A, Bareille MP, Beck A, Ollendorff V et al (2021) Does physical inactivity induce significant changes in human gut microbiota? New answers using the dry immersion hypoactivity model. Nutrients 13(11):3865
Dziewiecka H, Buttar HS, Kasperska A, Ostapiuk–Karolczuk J, Domagalska M, Cichoń J et al (2022) Physical activity induced alterations of gut microbiota in humans: a systematic review. BMC Sports Sci Med Rehabil 14(1):122
World Health Organization (2022) Physical activity. Geneva: World Health Organization. https://www.who.int/news-room/fact-sheets/detail/physical-activity. Accessed 18 Nov 2023
Hart NH, Galvão DA, Newton RU (2017) Exercise medicine for advanced prostate cancer. Curr Opin Support Palliat Care 11(3):247–257
Nilsen TS, Scott JM, Michalski M, Capaci C, Thomas S, Herndon JE 2nd et al (2018) Novel methods for reporting of exercise dose and adherence: an exploratory analysis. Med Sci Sports Exerc 50(6):1134–1141
Fairman CM, Nilsen TS, Newton RU, Taaffe DR, Spry N, Joseph D et al (2020) Reporting of resistance training dose, adherence, and tolerance in exercise oncology. Med Sci Sports Exerc 52(2):315–322
Ramsey I, Chan A, Charalambous A, Cheung YT, Darling HS, Eng L et al (2022) Exercise counselling and referral in cancer care: an international scoping survey of health care practitioners’ knowledge, practices, barriers, and facilitators. Support Care Cancer 30(11):9379–9391
Hayes SC, Newton RU, Spence RR, Galvão DA (2019) The Exercise and Sports Science Australia position statement: exercise medicine in cancer management. J Sci Med Sport 22(11):1175–1199
Newton RU, Kenfield SA, Hart NH, Chan JM, Courneya KS, Catto J et al (2018) Intense exercise for survival among men with metastatic castrate-resistant prostate cancer (INTERVAL-GAP4): a multicentre, randomised, controlled phase III study protocol. BMJ Open 8(5):e022899
Campbell KL, Neil SE, Winters-Stone KM (2012) Review of exercise studies in breast cancer survivors: attention to principles of exercise training. Br J Sports Med 46(13):909–916
Bland KA, Neil-Sztramko SE, Zadravec K, Medysky ME, Kong J, Winters-Stone KM et al (2021) Attention to principles of exercise training: an updated systematic review of randomized controlled trials in cancers other than breast and prostate. BMC Cancer 21(1):1179
Clarke SF, Murphy EF, O’Sullivan O, Lucey AJ, Humphreys M, Hogan A et al (2014) Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 63(12):1913–1920
Petersen LM, Bautista EJ, Nguyen H, Hanson BM, Chen L, Lek SH et al (2017) Community characteristics of the gut microbiomes of competitive cyclists. Microbiome. 5(1):98
O’Donovan CM, Madigan SM, Garcia-Perez I, Rankin A, O’Sullivan O, Cotter PD (2020) Distinct microbiome composition and metabolome exists across subgroups of elite Irish athletes. J Sci Med Sport 23(1):63–68
Estaki M, Pither J, Baumeister P, Little JP, Gill SK, Ghosh S et al (2016) Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Microbiome. 4(1):42
Barton W, Penney NC, Cronin O, Garcia-Perez I, Molloy MG, Holmes E et al (2018) The microbiome of professional athletes differs from that of more sedentary subjects in composition and particularly at the functional metabolic level. Gut. 67(4):625–633
Allen JM, Mailing LJ, Niemiro GM, Moore R, Cook MD, White BA et al (2018) Exercise alters gut microbiota composition and function in lean and obese humans. Med Sci Sports Exerc 50(4):747–757
O’Sullivan O, Cronin O, Clarke SF, Murphy EF, Molloy MG, Shanahan F et al (2015) Exercise and the microbiota. Gut Microbes 6(2):131–136
Jang LG, Choi G, Kim SW, Kim BY, Lee S, Park H (2019) The combination of sport and sport-specific diet is associated with characteristics of gut microbiota: an observational study. J Int Soc Sports Nutr 16(1):21
Barton W, Cronin O, Garcia-Perez I, Whiston R, Holmes E, Woods T et al (2021) The effects of sustained fitness improvement on the gut microbiome: a longitudinal, repeated measures case-study approach. Transl Sports Med 4(2):174–192
Kern T, Blond MB, Hansen TH, Rosenkilde M, Quist JS, Gram AS et al (2020) Structured exercise alters the gut microbiota in humans with overweight and obesity—a randomized controlled trial. Int J Obes 44(1):125–135
Motiani KK, Collado MC, Eskelinen J-J, Virtanen KA, Löyttyniemi E, Salminen S et al (2020) Exercise training modulates gut microbiota profile and improves endotoxemia. Med Sci Sports Exerc 52(1):94–104
Cronin O, Barton W, Moran C, Sheehan D, Whiston R, Nugent H et al (2019) Moderate-intensity aerobic and resistance exercise is safe and favorably influences body composition in patients with quiescent inflammatory bowel disease: a randomized controlled cross-over trial. BMC Gastroenterol 19(1):29
Huber Y, Pfirrmann D, Gebhardt I, Labenz C, Gehrke N, Straub BK et al (2019) Improvement of non-invasive markers of NAFLD from an individualised, web-based exercise program. Aliment Pharmacol Ther 50(8):930–939
Bycura D, Santos AC, Shiffer A, Kyman S, Winfree K, Sutliffe J et al (2021) Impact of different exercise modalities on the human gut microbiome. Sports (Basel) 9(2):14
Warbeck C, Dowd AJ, Kronlund L, Parmar C, Daun JT, Wytsma-Fisher K et al (2021) Feasibility and effects on the gut microbiota of a 12-week high-intensity interval training plus lifestyle education intervention on inactive adults with celiac disease. Appl Physiol Nutr Metab 46(4):325–336
Keohane DM, Woods T, O’Connor P, Underwood S, Cronin O, Whiston R et al (2019) Four men in a boat: ultra-endurance exercise alters the gut microbiome. J Sci Med Sport 22(9):1059–1064
Craven J, Cox AJ, Bellinger P, Desbrow B, Irwin C, Buchan J et al (2022) The influence of exercise training volume alterations on the gut microbiome in highly-trained middle-distance runners. Eur J Sport Sci 22(8):1222–1230
Hampton-Marcell JT, Eshoo TW, Cook MD, Gilbert JA, Horswill CA, Poretsky R (2020) Comparative analysis of gut microbiota following changes in training volume among swimmers. Int J Sports Med 41(5):292–299
Grosicki GJ, Fielding RA, Lustgarten MS (2018) Gut microbiota contribute to age-related changes in skeletal muscle size, composition, and function: biological basis for a gut-muscle axis. Calcif Tissue Int 102(4):433–442
Suryani D, Subhan Alfaqih M, Gunadi JW, Sylviana N, Goenawan H, Megantara I et al (2022) Type, intensity, and duration of exercise as regulator of gut microbiome profile. Curr Sports Med Rep 21(3):84–91
Boytar AN, Nitert MD, Morrision M, Skinner TL, Jenkins DG (2022) Exercise-induced changes to the human gut microbiota and implications for colorectal cancer: a narrative review. J Physiol 600(24):5189–5201
Cormie P, Zopf EM, Zhang X, Schmitz KH (2017) The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol Rev 39(1):71–92
Newton RU, Christophersen CT, Fairman CM, Hart NH, Taaffe DR, Broadhurst D et al (2019) Does exercise impact gut microbiota composition in men receiving androgen deprivation therapy for prostate cancer? A single-blinded, two-armed, randomised controlled trial. BMJ Open 9(4):e024872
Paulsen JA, Ptacek TS, Carter SJ, Liu N, Kumar R, Hyndman L et al (2017) Gut microbiota composition associated with alterations in cardiorespiratory fitness and psychosocial outcomes among breast cancer survivors. Support Care Cancer 25(5):1563–1570
Wang B, Jin Y-x, Dong J-l, Xiao H-w, Zhang S-q, Li Y et al (2021) Low-intensity exercise modulates gut microbiota to fight against radiation-induced gut toxicity in mouse models. Front Cell Dev Biol 9:706755
Allen JM, Mailing LJ, Cohrs J, Salmonson C, Fryer JD, Nehra V et al (2018) Exercise training-induced modification of the gut microbiota persists after microbiota colonization and attenuates the response to chemically-induced colitis in gnotobiotic mice. Gut Microbes 9(2):115–130
Lucia A. (2022). Exercise and Lifestyle Intervention for Patients With Adolescent Cancer: a Randomised Controlled Trial (HEALTHY ADOL). ClinicalTrials.gov ID: NCT05539794. Bethesda (MD): National Library of Medicine (US). https://www.clinicaltrials.gov/study/NCT05539794?term=NCT05539794. Accessed 18 Nov 2023
Marfil-Sánchez A, Seelbinder B, Ni Y, Varga J, Berta J, Hollosi V et al (2021) Gut microbiome functionality might be associated with exercise tolerance and recurrence of resected early-stage lung cancer patients. PLoS One 16(11):e0259898
Carter SJ, Hunter GR, Blackston JW, Liu N, Lefkowitz EJ, Van Der Pol WJ et al (2019) Gut microbiota diversity is associated with cardiorespiratory fitness in post-primary treatment breast cancer survivors. Exp Physiol 104(4):529–539
Machiels K, Joossens M, Sabino J, De Preter V, Arijs I, Eeckhaut V et al (2014) A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut. 63(8):1275–1283
Himbert C, Stephens WZ, Gigic B, Hardikar S, Holowatyj AN, Lin T et al (2022) Differences in the gut microbiome by physical activity and BMI among colorectal cancer patients. Am J Cancer Res 12(10):4789–4801
Sun L, Yan Y, Yan S, Yang Y (2022) Does physical activity associate with gut microbiome and survival outcomes of Chinese metastatic colorectal cancer patients? A secondary analysis of a randomized controlled trial. Heliyon. 8(11):e11615
Bielik V, Hric I, Šmahová S, Tkačiková M, Hlaváčová V, Nechalová L et al (2023) The effect of physical exercise and dairy probiotics (Lactobacillus casei) on gut microbiome in childhood cancer survivors. Neoplasma. 70(4):588–596
Donati Zeppa S, Natalucci V, Agostini D, Vallorani L, Amatori S, Sisti D et al (2023) Changes in gut microbiota composition after 12 weeks of a home-based lifestyle intervention in breast cancer survivors during the COVID-19 lockdown. Front Oncol 13:1225645
Gnagnarella P, Marvaso G, Jereczek-Fossa BA, de Cobelli O, Simoncini MC, Nevola Teixeira LF et al (2022) Life style and interaction with microbiota in prostate cancer patients undergoing radiotherapy: study protocol for a randomized controlled trial. BMC Cancer 22(1):794
Ryu J, Lee E-Y, Min J, Yeon S, Lee J-W, Chu SH et al (2023) Effect of a 1-year tailored exercise program according to cancer trajectories in patients with breast cancer: study protocol for a randomized controlled trial. BMC Cancer 23(1):200
Demark-Wahnefried W, Nix JW, Hunter GR, Rais-Bahrami S, Desmond RA, Chacko B et al (2016) Feasibility outcomes of a presurgical randomized controlled trial exploring the impact of caloric restriction and increased physical activity versus a wait-list control on tumor characteristics and circulating biomarkers in men electing prostatectomy for prostate cancer. BMC Cancer 16(1):61
Ueland K, Sanchez SC, Rillamas-Sun E, Shen H, Schattenkerk L, Garcia G et al (2022) A digital health intervention to improve nutrition and physical activity in breast cancer survivors: rationale and design of the Cook and Move for Your Life pilot and feasibility randomized controlled trial. Contemp Clin Trials 123:106993
Kenfield SA, Philip EJ, Phillips SM, Meyerhardt JA, Chan JM, Atreya CE et al (2022) Optimizing intervention tools to improve nutrition and physical activity for colorectal cancer survivors (tools to be fit): study protocol of a randomized factorial experiment. Contemp Clin Trials 123:107009
Boytar AN, Skinner TL, Wallen RE, Jenkins DG, Dekker NM (2023) The effect of exercise prescription on the human gut microbiota and comparison between clinical and apparently healthy populations: a systematic review. Nutrients 15(6):1534
Simpson CA, Schwartz OS, Eliby D, Butler CA, Huang K, Brien-Simpson N et al (2021) Bugs and brains, the gut and mental health study: a mixed-methods study investigating microbiota composition and function in anxiety, depression and irritable bowel syndrome. BMJ Open 11(3):e043221
Watson MD, Cross BL, Grosicki GJ (2021) Evidence for the contribution of gut microbiota to age-related anabolic resistance. Nutrients. 13(2):706
Ticinesi A, Lauretani F, Milani C, Nouvenne A, Tana C, Del Rio D et al (2017) Aging gut microbiota at the cross-road between nutrition, physical frailty, and sarcopenia: is there a gut-muscle axis? Nutrients 9(12):1303
Shanahan F, Ghosh TS, O’Toole PW (2021) The healthy microbiome—what is the definition of a healthy gut microbiome? Gastroenterology. 160(2):483–494
Lloyd-Price J, Abu-Ali G, Huttenhower C (2016) The healthy human microbiome. Genome Med 8(1):51
Aya V, Flórez A, Perez L, Ramírez JD (2021) Association between physical activity and changes in intestinal microbiota composition: a systematic review. PLoS One 16(2):e0247039
Marchbank T, Davison G, Oakes JR, Ghatei MA, Patterson M, Moyer MP et al (2011) The nutriceutical bovine colostrum truncates the increase in gut permeability caused by heavy exercise in athletes. Am J Physiol Gastrointest Liver Physiol 300(3):G477–G484
Zuhl MN, Lanphere KR, Kravitz L, Mermier CM, Schneider S, Dokladny K et al (1985) Effects of oral glutamine supplementation on exercise-induced gastrointestinal permeability and tight junction protein expression. J Appl Physiol 116(2):183–191
Keirns BH, Koemel NA, Sciarrillo CM, Anderson KL, Emerson SR (2020) Exercise and intestinal permeability: another form of exercise-induced hormesis? Am J Physiol Gastrointest Liver Physiol 319(4):G512–G518
Acknowledgements
NHH is MASCC Founding Chair of Exercise Oncology and MASCC Chair of Fatigue, HRW is MASCC Vice-Chair of Mucositis, and RJC is MASCC Chair of Survivorship for the Multinational Association of Supportive Care in Cancer. NHH is a MASCC Terry Langbaum Survivorship Fellow. DH is a MASCC Cognition Fellow.
Funding
NHH and RJC receive salary support from the National Health and Medical Research Council as investigator fellows (APP2018070 and APP1194051). HRW receives salary support from the Hospital Research Foundation Group as a research fellow.
Author information
Authors and Affiliations
Contributions
NHH, MPW, RJC, and HRW conceptualised the review topic, scope, and content. All authors contributed significantly to the preparation, drafting, revision, and completion of the manuscript at multiple stages throughout the process. All authors reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
NHH is an associate editor for the Supportive Care in Cancer journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nicolas H. Hart and Matthew P. Wallen are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hart, N.H., Wallen, M.P., Farley, M.J. et al. Exercise and the gut microbiome: implications for supportive care in cancer. Support Care Cancer 31, 724 (2023). https://doi.org/10.1007/s00520-023-08183-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-08183-7