Abstract
Purpose
To explore the correlation between financial toxicity, social support, and social functioning in post-chemotherapy breast cancer patients, as well as any possible interaction of financial toxicity and social support on social functioning.
Methods
Post-chemotherapy breast cancer patients admitted to the thyroid and breast surgery departments of three first-class general hospitals in East China from December 2020 to January 2022 were recruited by convenience sampling for a cross-sectional survey. The survey instruments included the general information form, the comprehensive scores for financial toxicity based on the patient-reported outcome measures (COST-PROM), the social roles and activity participation subscale from the patient-reported outcomes measurement system-breast-chemotherapy (PROMS-B-C) (score range: 8–40), and the social support subscale from PROMS-B-C (score range: 16–80).
Results
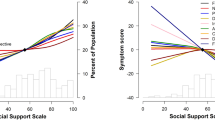
The results showed that low social functioning (low score) in post-chemotherapy breast cancer patients was positively correlated with high financial toxicity (low score) as well as poor economic resources (low score) and poor psychosocial responses (low score) (P<0.01) and negatively correlated with low economic expenditures (low score) (P<0.01); high social functioning (high score) was positively correlated with high social support (high score) (P<0.01). The interaction analysis results showed an additive interaction between financial toxicity and social support in social functioning.
Conclusion
There was an additive interaction of financial toxicity and social support in the social functioning of post-chemotherapy breast cancer patients. Those patients with high financial toxicity and low social support are the most likely to benefit from relevant intervention measures compared to other breast cancer populations.

Similar content being viewed by others
Data availability
The authors have full control of all primary data and agree to allow the journal to review the data on reasonable request.
References
World Health Organization (2020) World cancer report: cancer research for cancer prevention. International Agency for Research on. Cancer https://www.iarc.fr/cards_page/world-cancer-report/. Accessed 10 Dec 2022.
Fan L, Strasser-Weippl K, Li JJ, St Louis J, Finkelstein DM, Yu KD et al (2014) Breast cancer in China. Lancet Oncol 15(7):e279–e289
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM et al (2019) Cancer treatment and survivorship statistics, 2019. CA A Cancer J Clin. 69(5):363–385
China Anti-cancer Association Committee of Breast Cancer Society (2021) Chinese anti-cancer society guidelines and specifications for breast cancer diagnosis and treatment (2021 Edition). China Oncol 31:954–1040
Ahmed AE, Alharbi AG, Alsadhan MA, Almuzaini AS, Almuzaini HS, Ali YZ et al (2017) The predictors of poor quality of life in a sample of Saudi women with breast cancer. BCTT 9:51–58
Hahn EA, Beaumont JL, Pilkonis PA, Garcia SF, Magasi S, DeWalt DA et al (2016) The PROMIS satisfaction with social participation measures demonstrated responsiveness in diverse clinical populations. J Clin Epidemiol 73:135–141
Metternich B, Wagner K, Geiger MJ, Schulze-Bonhage A, Hirsch M, Schönenberg M (2022) Affective empathy, theory of mind and social functioning in patients with focal epilepsy. Front Psychiatry:13
Zhang D, Wei J, Li X (2022) The mediating effect of social functioning on the relationship between social support and fatigue in middle-aged and young recipients with liver transplant in China. Front Psychol:13
Gottlieb BH, Bergen AE (2010) Social support concepts and measures. J Psychosom Res. 69(5):511–520
Masoumi S, Amiri M, Yousefi AM (2022) Self-compassion: the factor that explains a relationship between perceived social support and emotional self-regulation in psychological well-being of breast cancer survivors. IJPS
Attai DJ, Cowher MS, Al-Hamadani M, Schoger JM, Staley AC, Landercasper J (2015) Twitter social media is an effective tool for breast cancer patient education and support: patient-reported outcomes by survey. J Med Internet Res 17(7):e188
Manandhar S, Shrestha DS, Taechaboonsermsk P, Siri S, Suparp J (2014) Quality of life among breast cancer patients undergoing treatment in national cancer centers in Nepal. Asian Pac J Cancer Prev 15(22):9753–9757
Nguyen NH, Khera R, Ohno-Machado L, Sandborn WJ, Singh S (2020) Estimates of the prevalence and effects of food insecurity and social support on financial toxicity in and healthcare use by patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol
La Vecchia C, Rota M, Malvezzi M, Negri E (2015) Potential for improvement in cancer management: reducing mortality in the European Union. The Oncol 20(5):495–498
Mariotto AB, Robin Yabroff K, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010-2020. JNCI J Nat Cancer Inst 103(2):117–128
Park J, Look KA (2019) Health care expenditure burden of cancer care in the United States. INQUIRY 56:004695801988069
Xu T, Wu J (2018) Financial toxicity of cancer in China. J Cancer Policy. 15:96–99
Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X et al (2013) The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. The Oncol 18(4):381–390
Gordon LG, Chan RJ (2017) Financial toxicity among patients with cancer—where to from here? Cancer Nurs 40(4):257–258
Semin JN, Palm D, Smith LM, Ruttle S (2020) Understanding breast cancer survivors’ financial burden and distress after financial assistance. Supp Care Cancer 28(9):4241–4248
Cancer Support Community. Elevating the patient voice: cancer experience registry index report 2013–2014 2014. Cancer Support Community Web. https://www.cancersupportcommunity.org/sites/default/files/d7/document/2014_cer_index_report.pdf. Accessed 10 Dec 2022.
Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR (2016) Financial hardships experienced by cancer survivors: a systematic review. JNCI. J Natl Cancer Inst 109(2):djw205
Byers TE, Wolf HJ, Bauer KR, Bolick-Aldrich S, Chen VW, Finch JL et al (2008) The impact of socioeconomic status on survival after cancer in the United States. Cancer 113(3):582–591
Ramsey SD, Bansal A, Fedorenko CR, Blough DK, Overstreet KA, Shankaran V et al (2016) Financial insolvency as a risk factor for early mortality among patients with cancer. JCO 34(9):980–986
Gordon LG, Walker SM, Mervin MC, Lowe A, Smith DP, Gardiner RA et al (2015) financial toxicity: a potential side effect of prostate cancer treatment among Australian men. Eur J Cancer Care 26(1):e12392
Rothman K (2004) Interaction and evolution in epidemiology. Sozial- und Präventivmedizin 49(2):105–106
de Souza JA, Yap BJ, Hlubocky FJ, Wroblewski K, Ratain MJ, Cella D et al (2014) The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer 120(20):3245–3253
Huihui Y, Xue B, Yunyong L (2017) Reliability and validity study of the economic toxicity scale for reported outcomes of Chinese cancer patients. Chinese J Epidemiol. https://doi.org/10.3760/cma.j.issn.0254-6450.2017.08.024
Wu Fu Lei (2019) A study on the construction of a stage-specific patient-reported outcome measurement system for breast cancer[dissertation]. Chinese People’s Liberation Army Naval Medical University, Shanghai
Rothman K (2002) Epidemiology: an introduction. Oxford University Press
Xu MR, Qiang DR, Zhou YH, Shi S, Qin J, Tao Y (2017) Interaction analysis of logistic regression models using R software. Chin J Health Stat 34(4):670–672
Carlozzi NE, Ianni PA, Lange RT, Brickell TA, Kallen MA, Hahn EA et al (2019) Understanding health-related quality of life of caregivers of civilians and service members/veterans with traumatic brain injury: establishing the reliability and validity of PROMIS social health measures. Arch Phys Med Rehabil 100(4):S110–S118
Meeker CR, Geynisman DM, Egleston BL, Hall MJ, Mechanic KY, Bilusic M et al (2016) Relationships among financial distress, emotional distress, and overall distress in insured patients with cancer. JOP 12(7):e755–e764
Fitch MI, Sharp L, Hanly P, Longo CJ (2021) Experiencing financial toxicity associated with cancer in publicly funded healthcare systems: a systematic review of qualitative studies. J Cancer Surviv
Fitch MI, Nicoll I (2019) Returning to work after cancer: survivors’, caregivers’, and employers’ perspectives. Psycho-Oncol 28(4):792–798
Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ (2009) The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat 119(1):213–220
Messina CR, Lane DS, Glanz K, West DS, Taylor V, Frishman W et al (2004) Relationship of social support and social burden to repeated breast cancer screening in the women’s health initiative. Health Psychol 23(6):582–594
Oh GH, Yeom CW, Shim EJ, Jung D, Lee KM, Son KL et al (2020) The effect of perceived social support on chemotherapy-related symptoms in patients with breast cancer: a prospective observational study. J Psychosom Res 130:109911
Durá-Ferrandis E, Mandelblatt JS, Clapp J, Luta G, Faul L, Kimmick G et al (2017) Personality, coping, and social support as predictors of long-term quality-of-life trajectories in older breast cancer survivors: CALGB protocol 369901 (Alliance). Psycho-Oncol 26(11):1914–1921
Trevino KM, Nelson CJ, Saracino RM, Korc-Grodzicki B, Sarraf S, Shahrokni A (2019) Is screening for psychosocial risk factors associated with mental health care in older adults with cancer undergoing surgery? Cancer 126(3):602–610
Niu Z, Bhurosy T, Heckman C (2021) Cancer survivors’ emotional well-being: roles of internet information seeking, patient-centered communication, and social support. J Health Commun 26(7):514–522
Coughlin SS (2019) Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat 177(3):537–548
VanderWeele TJ, Knol MJ (2014) A tutorial on interaction. Epidemiol Methods 3:1
Acknowledgements
We offer our heartfelt appreciation to the study participants and the affiliated hospitals.
Funding
This study was supported by National Natural Science Foundation of China (Grant No. 81801098) and the Key Project of Philosophy and Social Science Research in Colleges and Universities in Jiangsu Province (No. 2023SJZD144).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Qiuyun Chen, Lu Lin, Fengxia Lai, Daoxia Guo, and Jie Wang. The first draft of the manuscript was written by Qiuyun Chen and was supervised by Li Tian. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study acquired ethical approval from the Medical Ethics Committee of Soochow University (Approval No. 20201221H03). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, L., Chen, Q., Lai, F. et al. The interaction of financial toxicity and social support on social functioning in post-chemotherapy breast cancer patients: a cross-sectional study. Support Care Cancer 31, 583 (2023). https://doi.org/10.1007/s00520-023-08048-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-08048-z