Abstract
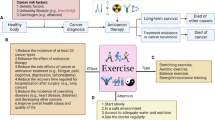
Exercise is effective for improving the physical and psychological health of breast cancer patients. However, there is still controversy around its role on the immune system. Therefore, this systematic review and meta-analysis is aimed to evaluate the effect of chronic exercise on the number and activity of the immune cells that can contribute to anti-tumor immune responses, such as natural killers (NK) cells, CD + 4, or CD + 8. The main hypothesis of this study was that exercise could improve the immune system or, at least, there will not be a reduction in the number or activity of immune cells because of exercise. The search was conducted in the PubMed and Web of Science databases. Out of 244 studies reviewed, 10 studies met the inclusion criteria. The studies included in the meta-analyses showed mixed results and no significant (p > 0.05) positive or negative effects of exercise interventions in women with breast cancer. Therefore, the current evidence indicates that exercise does not significantly improve or reduce the immune system; thus, the prescription of exercise must not be discouraged due to the effects on the number and activity of immune system cells, but should be recommended due to the well-known benefits in quality of life, physical function or fatigue, and the absence of negative effects on the immune system. Further studies are needed to evaluate the effects according to the type of exercise, the type of cancer, or the timing of the intervention.







Similar content being viewed by others
Data availability
The data that support the study findings are available from the corresponding author upon request.
References
Ma F, Laster K, Dong Z (2022) The comparison of cancer gene mutation frequencies in Chinese and U.S. patient populations. Nat Commun 13(1):5651
World Health Organization (WHO). Global Health Estimates 2020: deaths by cause, A., Sex, by country and by region, 2000–2019. WHO; 2020. Accessed December 11, 2020
Font-Clos F, Zapperi S, La Porta CAM (2022) Classification of triple negative breast cancer by epithelial mesenchymal transition and the tumor immune microenvironment. Sci Rep 12(1):9651
Saini A et al (2020) Cancer causes and treatments. Int J Pharm Sci Res 11(7):3121–3134
Saha M (2022) Medical oncology in cancer treatment. cancer diagnostics and therapeutics: current trends, challenges, and future perspectives. Springer, pp 271–285
Savas P, Loi S (2020) Expanding the role for immunotherapy in triple-negative breast cancer. Cancer Cell 37(5):623–624
Riondino S et al (2023) Obesity and breast cancer: interaction or interference with the response to therapy? Curr Oncol 30(1):1220–1231
Kamel HF, Al-Amodi HS, Abdelsattar S (2023) Obesity, cancer and the immune system: cross talks and complex interplay
Crespi E, Bottai G, Santarpia L (2016) Role of inflammation in obesity-related breast cancer. Curr Opin Pharmacol 31:114–122
Smith RT (1968) Tumor-specific immune mechanisms. N Engl J Med 278(22):1207–1214
De Souza AP, Bonorino C (2009) Tumor immunosuppressive environment: effects on tumor-specific and nontumor antigen immune responses. Expert Rev Anticancer Ther 9(9):1317–1332
McKallip R, Li R, Ladisch S (1999) Tumor gangliosides inhibit the tumor-specific immune response. J Immunol 163(7):3718–3726
Ostroumov D et al (2018) CD4 and CD8 T lymphocyte interplay in controlling tumor growth. Cell Mol Life Sci 75(4):689–713
Tay RE, Richardson EK, Toh HC (2021) Revisiting the role of CD4+ T cells in cancer immunotherapy—new insights into old paradigms. Cancer Gene Ther 28(1):5–17
Raskov H et al (2021) Cytotoxic CD8+ T cells in cancer and cancer immunotherapy. Br J Cancer 124(2):359–367
Waldman AD, Fritz JM, Lenardo MJ (2020) A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol 20(11):651–668
Wolf NK, Kissiov DU, Raulet DH (2023) Roles of natural killer cells in immunity to cancer, and applications to immunotherapy. Nat Rev Immunol 23(2):90–105
Erber R, Hartmann A (2020) Understanding PD-L1 testing in breast cancer: a practical approach. Breast Care (Basel) 15(5):481–490
Schütz F et al (2017) PD-1/PD-L1 Pathway in breast cancer. Oncol Res Treat 40(5):294–297
Arasanz H et al (2017) PD1 signal transduction pathways in T cells. Oncotarget 8(31):51936–51945
Zhou T et al (2018) Expression of programmed death ligand-1 and programmed death-1 in samples of invasive ductal carcinoma of the breast and its correlation with prognosis. Anticancer Drugs 29(9):904–910
Rizzo A, Ricci AD (2022) Biomarkers for breast cancer immunotherapy: PD-L1, TILs, and beyond. Expert Opin Investig Drugs 31(6):549–555
Quatrini L et al. (2020) The immune checkpoint PD-1 in Natural killer cells: expression, function and targeting in tumour immunotherapy. Cancers (Basel) 12(11)
Arianfar E et al (2023) Suppression of CD56(bright) NK cells in breast cancer patients is associated with the PD-1 and TGF-βRII expression. Clin Transl Oncol 25(3):841–851
Abdel-Latif M, Youness RA (2020) Why natural killer cells in triple negative breast cancer? World J Clin Oncol 11(7):464–476
Razeghian E et al (2022) The role of the natural killer (NK) cell modulation in breast cancer incidence and progress. Mol Biol Rep 49(11):10935–10948
Jones LW, Alfano CM (2013) Exercise—oncology research: past, present, and future. Acta Oncol 52(2):195–215
Holmen Olofsson G et al (2020) Exercise oncology and immuno-oncology; a (future) dynamic duo. Int J Mol Sci 21(11):3816
Stout NL et al (2020) An exercise oncology clinical pathway: screening and referral for personalized interventions. Cancer 126(12):2750–2758
Valenti M et al (2008) Exercise and quality of life in breast cancer survivors. Int J Med Sci 5(1):24
Schleicher E et al (2023) Moderators of physical activity and quality of life response to a physical activity intervention for breast cancer survivors. Support Care Cancer 31(1):53
Ye X-X et al (2022) Effectiveness of Baduanjin exercise on quality of life and psychological health in postoperative patients with breast cancer: a systematic review and meta-analysis. Integr Cancer Ther 21:15347354221104092
Brolinson PG, Elliott D (2007) Exercise and the immune system. Clin Sports Med 26(3):311–319
Fitzgerald L (1988) Exercise and the immune system. Immunol Today 9(11):337–339
Ligibel JA et al (2019) Impact of a pre-operative exercise intervention on breast cancer proliferation and gene expression: results from the Pre-Operative Health and Body (PreHAB) study. Clin Cancer Res 25(17):5398–5406
Sagarra-Romero L et al (2018) Influence of an exercise program on blood immune function in women with breast cancer. Med Dello Sport 71:604–616
Schmidt T et al (2018) Influence of physical activity on the immune system in breast cancer patients during chemotherapy. J Cancer Res Clin Oncol 144(3):579–586
Saxton JM et al (2014) Effects of an exercise and hypocaloric healthy eating intervention on indices of psychological health status, hypothalamic-pituitary-adrenal axis regulation and immune function after early-stage breast cancer: a randomised controlled trial. Breast Cancer Res 16(2):R39
Hutnick NA et al (2005) Exercise and lymphocyte activation following chemotherapy for breast cancer. Med Sci Sports Exerc 37(11):1827–1835
Hiensch AE et al (2021) Inflammation mediates exercise effects on fatigue in patients with breast cancer. Med Sci Sports Exerc 53(3):496–504
Hagstrom AD et al (2016) The effect of resistance training on markers of immune function and inflammation in previously sedentary women recovering from breast cancer: a randomized controlled trial. Breast Cancer Res Treat 155(3):471–482
Fairey AS et al (2005) Randomized controlled trial of exercise and blood immune function in postmenopausal breast cancer survivors. J Appl Physiol (1985) 98(4):1534–40
Nieman DC et al (1995) Moderate exercise training and natural killer cell cytotoxic activity in breast cancer patients. Int J Sports Med 16(5):334–337
Lee KJ, An KO (2022) Impact of high-intensity circuit resistance exercise on physical fitness, inflammation, and immune cells in female breast cancer survivors: a randomized control trial. Int J Environ Res Public Health, 19(9)
Valenzuela PL et al (2022) Exercise training and natural killer cells in cancer survivors: current evidence and research gaps based on a systematic review and meta-analysis. Sports Med Open 8(1):36
Gustafson MP et al. (2021) Exercise and the immune system: taking steps to improve responses to cancer immunotherapy. J Immunother Cancer, 9(7)
Forte P, Branquinho L, Ferraz R (2022) The relationships between physical activity, exercise, and sport on the immune system. Int J Environ Res Public Health, 19(11)
Kruger K, Mooren F (2007) T cell homing and exercise. Exerc Immunol Rev 13:37–54
Pedersen BK, Hoffman-Goetz L (2000) Exercise and the immune system: regulation, integration, and adaptation. Physiological reviews
Pedersen BK (2000) Exercise and cytokines. Immunol Cell Biol 78(5):532–535
Page M, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. MetaArXiv 2020:2020
Higgins JP et al. (2019) Assessing risk of bias in a randomized trial. Cochrane handbook for systematic reviews of interventions 205–228
McGuinness LA, Higgins JP (2021) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12(1):55–61
Montaño-Rojas LS et al (2020) Resistance training in breast cancer survivors: a systematic review of exercise programs. Int J Environ Res Public Health 17(18):6511
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):1–10
Schmidt FL, Oh IS, Hayes TL (2009) Fixed- versus random-effects models in meta-analysis: model properties and an empirical comparison of differences in results. Br J Math Stat Psychol 62(Pt 1):97–128
Deeks JJ et al. (2019) Analysing data and undertaking meta‐analyses. Cochrane handbook for systematic reviews of interventions, 241–284
Higgins J, Green S (2011) 17.8. 2 Study summaries using more than one patient-reported outcome. Cochrane handbook for systematic reviews of interventions
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Lavín-Pérez AM et al (2021) High-intensity exercise to improve cardiorespiratory fitness in cancer patients and survivors: a systematic review and meta-analysis. Scand J Med Sci Sports 31(2):265–294
Lavín-Pérez AM et al (2021) Effects of high-intensity training on the quality of life of cancer patients and survivors: a systematic review with meta-analysis. Sci Rep 11(1):15089
Villasenor A et al (2012) Prevalence and prognostic effect of sarcopenia in breast cancer survivors: the HEAL study. J Cancer Surviv 6(4):398–406
Caan BJ, Cespedes Feliciano EM, Kroenke CH (2018) The importance of body composition in explaining the overweight paradox in cancer-counterpoint. Cancer Res 78(8):1906–1912
Collado-Mateo D et al (2021) Key factors associated with adherence to exercise in patients with chronic diseases and older adults: an umbrella review. Int J Environ Res Public Health 18(4):2023
Dunne D et al (2016) Randomized clinical trial of prehabilitation before planned liver resection. Journal of British Surgery 103(5):504–512
Castro F et al (2018) Interferon-gamma at the crossroads of tumor immune surveillance or evasion. Front Immunol 9:847
Gocher AM, Workman CJ, Vignali DA (2022) Interferon-γ: teammate or opponent in the tumour microenvironment? Nat Rev Immunol 22(3):158–172
Emery A et al (2022) Reframing how physical activity reduces the incidence of clinically-diagnosed cancers: appraising exercise-induced immuno-modulation as an integral mechanism. Front Oncol 12:221
Campbell JP et al (2009) Acute exercise mobilises CD8+ T lymphocytes exhibiting an effector-memory phenotype. Brain Behav Immun 23(6):767–775
Author information
Authors and Affiliations
Contributions
Idea, conceptualization, project administration, and editing, A.A.H.; writing—original draft preparation, A.A.H., SH.A., and J.B.F.J.; analysis and editing, A.M.L.P. and D.C.M. Authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• There is large controversy around the effects of exercise on the number and activity of immune cells.
• Meta-analyses results showed mixed results and no significant positive or negative effects of exercise interventions on the number and activity of immune cells in women with breast cancer.
• The prescription of exercise must not be discouraged due to the effects on the number and activity of immune system cells.
• Participant’s adherence to exercise must be taken into account in exercise interventions in breast cancer patients.
• Conducting more research studies in this area could lead to the development of exercise immunology during breast cancer treatment and survivorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lavín-Pérez, A.M., Collado-Mateo, D., Abbasi, S. et al. Effects of exercise on immune cells with tumor-specific activity in breast cancer patients and survivors: a systematic review and meta-analysis. Support Care Cancer 31, 507 (2023). https://doi.org/10.1007/s00520-023-07968-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07968-0