Abstract
Purpose
The goal of this study is to investigate the social isolation (SI) subtypes of patients with breast cancer (BC) and to explore its influencing factors.
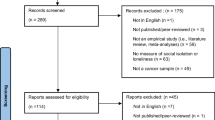
Methods
A sample of 303 BC patients participated in the study from September to December, 2021. Latent profile analysis (LPA) was performed to identify SI clusters based on the three sub-scales of the Chinese version of the Social Anxiety Scale, the Chinese version of the Social Avoidance and Distress Scale, and the Chinese version of the Loneliness Scale.
Results
We found that SI can be divided into three categories: high-level (Class 1), middle-level (Class 2), and low-level (Class 3), accounting for 20.46%, 33.00%, and 46.54%, respectively. Compared to Class 3, Class 1, which had the lower average monthly income per family member (RMB) (< 3000: OR = 5.298, P = .021; 3000 ~ 5000: OR = 5.320, P = .018), was more likely to suffer from SI due to occupation (Laborer: OR = 12.023, P = .009). Surgery (OR = 14.138, P < .001; OR = 2.777, P = .020), chemotherapy (OR = 10.224, P = .001; OR = 3.545, P = .001); poorer family functioning (OR = .671, P < .001; OR = .801, P = .002), and lower levels of self-transcendence (OR = .806, P < .001; OR = .911, P < .001) were important influencing factors for SI in Class 1 and Class 2 compared to Class 3.
Conclusion
SI is classifiably heterogeneous among patients with BC. Strategies that identify characteristics of SI and give targeted intervention focusing on family functioning and improving self-transcendence levels contribute to the prevention of SI among patients with BC.

Similar content being viewed by others
Data Availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. Go to contact the corresponding author.
Abbreviations
- SI:
-
Social isolation
- BC:
-
Breast cancer
- LPA:
-
Latent Profile Analysis
- C-SAS:
-
The Chinese version of the Social Anxiety Scale
- C-SADS:
-
The Chinese version of the Social Avoidance and Distress Scale
- C-LS:
-
The Chinese version of the Loneliness Scale
- AIC:
-
Akaike Information Criterion
- BIC:
-
Bayesian Information Criterion
- aBIC:
-
Samplesize-adjusted Bayesian Information Criterion
- LMR:
-
Lo-Mendell-Rubin Adjusted Likelihood Ratio Test
- BLRT:
-
Bootstrap Likelihood Ratio Test
References
Sung H et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Huang J et al (2021) Global incidence and mortality of breast cancer: a trend analysis. Aging (Albany NY) 13(4):5748–5803. https://doi.org/10.18632/aging.202502
Smith T et al (2007) The rationale, design, and implementation of the American Cancer Society’s studies of cancer survivors. Cancer 109(1):1–12. https://doi.org/10.1002/cncr.22387
Jakobsen K et al (2018) Everyday life in breast cancer survivors experiencing challenges: A qualitative study. Scand J Occup Ther 25(4):298–307. https://doi.org/10.1080/11038128.2017.1335777
Kugbey N, Oppong AK, Meyer-Weitz A (2020) Depression, anxiety and quality of life among women living with breast cancer in Ghana: mediating roles of social support and religiosity. Support Care Cancer 28(6):2581–2588. https://doi.org/10.1007/s00520-019-05027-1
Maass SW et al (2015) The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: A systematic review. Maturitas 82(1):100–108. https://doi.org/10.1016/j.maturitas.2015.04.010
Watson D, Friend R (1969) Measurement of social-evaluative anxiety. J Consult Clin Psychol 33(4):448–457. https://doi.org/10.1037/h0027806
Finelay M, Spencer R (2009) Social isolation: Development of an Assessment Tool for HACC Services[R]. Macquarie University Press, Sydney
Nicholson NR-Jr (2009) Social isolation in older adults: an evolutionary concept analysis. J Adv Nurs 65(6):1342–1352. https://doi.org/10.1111/j.1365-2648.2008.04959.x
Liang Y, Hao G, Wu M et al (2022) Social isolation in adults with cancer An evolutionary concept analysis. Front Psychol 13:973640. https://doi.org/10.3389/fpsyg.2022.973640
Kroenke CH et al (2017) Postdiagnosis Social Networks and Breast Cancer Mortality in the After Breast Cancer Pooling Project. Cancer: J Am Cancer Soc 123(7):1228–1237
Coughlin SS (2019) Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat 177(3):537–548. https://doi.org/10.1007/s10549-019-05340-7
Freedman A, Nicolle J (2020) Social isolation and loneliness: the new geriatric giants: Approach for primary care. Can Fam Physician 66(3):176–182
Kroenke CH et al (2013) Social networks, social support, and burden in relationships, and mortality after breast cancer diagnosis in the Life After Breast Cancer Epidemiology (LACE) study. Breast Cancer Res Treat 137(1):261–271. https://doi.org/10.1007/s10549-012-2253-8
Li Y et al (2018) Bayesian Latent Class Analysis Tutorial. Multivar Behav Res 53(3):430–451. https://doi.org/10.1080/00273171.2018.1428892
Mullins LB et al (2020) Internet Programming to Reduce Loneliness and Social Isolation in Aging. Res Gerontol Nurs 13(5):233–242. https://doi.org/10.3928/19404921-20200320-01
Aparna S et al (2011) Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol 30(4):377–385. https://doi.org/10.1037/a0022826
Hajek A, Konig HH, (2021) The Association between oral health-related quality of life, loneliness, perceived and objective social isolation-results of a nationally representative survey. Int J Environ Res Public Health 18(24): 2886. https://doi.org/10.3390/ijerph182412886
James L et al (2006) Performance of an Abbreviated Version of the Lubben Social Network Scale Among Three European Community-Dwelling Older Adult Populations. Narnia 46(4):503–513. https://doi.org/10.1093/geront/46.4.503
Qi YZ (2010) On social isolation. J Chongqing Univ Commer Ind (Social Science Edition) 27(1):82–86. https://doi.org/10.3969/j.issn.1672-0598.2010.01.013
Wang S et al (2020) Research on the status and influencing factors of social isolation in breast cancer patients. P.L.A. Nurs J 37(12):5–9. https://doi.org/10.3969/j.issn.1008-9993.2020.12.002
Nancy AB et al (2015) Partner support and anxiety in young women with breast cancer. Psychooncology 24(12):1679–1685. https://doi.org/10.1002/pon.3780
Liu B et al (2021) Correlations of social isolation and anxiety and depression symptoms among patients with breast cancer of Heilongjiang province in China: The mediating role of social support. Nurs Open 8(4):1981–1989. https://doi.org/10.1002/nop2.876
Li Y et al (2018) Relationships between family resilience, breast cancer survivors’ individual resilience, and caregiver burden: A cross-sectional study. Int J Nurs Stud 88:79–84. https://doi.org/10.1016/j.ijnurstu.2018.08.011
Zhang Y (2018) Family functioning in the context of an adult family member with illness: A concept analysis. J Clin Nurs 27(15–16):3205–3224. https://doi.org/10.1111/jocn.14500
Schuler TA et al (2014) Typology of perceived family functioning in an American sample of patients with advanced cancer. J Pain Symptom Manag 48(2):281–288. https://doi.org/10.1016/j.jpainsymman.2013.09.013
Jeong A et al (2016) Avoidance of cancer communication, perceived social support, and anxiety and depression among patients with cancer. Psychooncology 25(11):1301–1307. https://doi.org/10.1002/pon.4060
Yang Y et al (2018) Factors associated with fear of progression in chinese cancer patients: sociodemographic, clinical and psychological variables. J Psychosom Res 114:18–24. https://doi.org/10.1016/j.ijnurstu.2018.08.011
Haugan G, Moksnes UK, Lohre A (2016) Intrapersonal self-transcendence, meaning-in-life and nurse-patient interaction: powerful assets for quality of life in cognitively intact nursing-home patients. Scand J Caring Sci 30(4):790–801. https://doi.org/10.1111/scs.12307
Haugan G, Innstrand ST (2012) The effect of self-transcendence on depression in cognitively intact nursing home patients. ISRN Psychiatry 2012:301–325. https://doi.org/10.5402/2012/301325
Reed PG (1991) Toward a nursing theory of self-transcendence: deductive reformulation using developmental theories. ANS Adv Nurs Sci 13(4):64–77. https://doi.org/10.1097/00012272-199106000-00008
Abdollahi A et al (2021) Effects of Death Anxiety on Perceived Stress in Individuals With Multiple Sclerosis and the Role of Self-Transcendence. Omega (Westport) 84(1):91–102. https://doi.org/10.1177/0030222819880714
Palmer B et al (2010) Self-transcendence and work engagement in acute care staff registered nurses. Crit Care Nurs Q 33(2):138–147. https://doi.org/10.1097/CNQ.0b013e3181d912d8
Liu P, et al (2022) Why does one want to feel socially engaging emotions? The role of self-transcendence values on desired emotions among adolescents. Pers Individ Differ 185:111257. https://doi.org/10.1016/j.paid.2021.111257
Wang X, et al (1999) Manual of mental health rating scale [M]. Beijing, Chin J Ment Health
Wang D. (1995) Reliability and validity of the russell loneliness scale. Chin J Clin Psychol 1(01):23–25. http://ir.calis.edu.cn/hdl/211010/16747
Smilkstein G (1978) The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract 6(6):1231–1239
Lv F, Gu Y (1995) The family APGAR questionnaire and its clinical application. Foreign Medicine (Hospital Management Volume) 3(02):56–59. cnki/sun/gwyg.0.1995–02–002
Reed PG (1991) Self-transcendence and mental health in oldest-old adults. Nurs Res 40(1):5–11. https://doi.org/10.1097/00006199-199101000-00002
Zhang J (2014) Reliability and validity of Chinese version of self-transcendence scale in the elderly. Chin J Gerontol 34(07):1910–1. https://doi.org/10.3969/j.issn.1005-9202.2014.07.083
Lee MK et al (2017) Three-Year Prospective Cohort Study of Factors Associated with Return to Work After Breast Cancer Diagnosis. J Occup Rehabil 27(4):547–558. https://doi.org/10.1007/s10926-016-9685-7
Bargon CA et al (2021) Impact of the COVID-19 Pandemic on Patient-Reported Outcomes of Breast Cancer Patients and Survivors. JNCI Cancer Spectr 5(1):a104. https://doi.org/10.1093/jncics/pkaa104
Yuan Y et al (2022) The relationship between depression and social avoidance of college students: A moderated mediation model. J Affect Disord 300:249–254. https://doi.org/10.1016/j.jad.2021.12.119
Dai J, et al (2011) Prevalence and influencing factors of social avoidance and distress in college students. Chin Public Health 27(9):1084–1086. cnki/sun/zggw.0.2011–09–005
Holt-Lunstad J et al (2015) Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 10(2):227–237. https://doi.org/10.1177/1745691614568352
Puigpinós-Riera R et al (2018) Anxiety and depression in women with breast cancer: Social and clinical determinants and influence of the social network and social support (DAMA cohort). Cancer Epidemiol 55:123–129. https://doi.org/10.1016/j.canep.2018.06.002
Kolokotroni P, Anagnostopoulos F, Hantzi A (2018) The Role of Optimism, Social Constraints, Coping, and Cognitive Processing in Psychosocial Adjustment Among Breast Cancer Survivors. J Clin Psychol Med Settings 25(4):452–462. https://doi.org/10.1007/s10880-018-9555-x
Yeung N, Lu Q, Mak W (2019) Self-perceived burden mediates the relationship between self-stigma and quality of life among Chinese American breast cancer survivors. Support Care Cancer 27(9):3337–3345. https://doi.org/10.1007/s00520-018-4630-2
Rentscher KE et al (2021) Loneliness and mental health during the COVID-19 pandemic in older breast cancer survivors and noncancer controls. Cancer 127(19):3671–3679. https://doi.org/10.1002/cncr.33687
Kroenke CH et al (2006) Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol 24(7):1105–1111. https://doi.org/10.1200/JCO.2005.04.2846
Benedict C et al (2022) Greater financial toxicity relates to greater distress and worse quality of life among breast and gynecologic cancer survivors. Psychooncology 31(1):9–20. https://doi.org/10.1002/pon.5763
Ngan TT et al (2021) Financial toxicity due to breast cancer treatment in low- and middle-income countries: evidence from Vietnam. Support Care Cancer 29(11):6325–6333. https://doi.org/10.1007/s00520-021-06210-z
Meernik C et al (2021) Breast Cancer-Related Employment Disruption and Financial Hardship in the Sister Study. JNCI Cancer Spectr 5(3):kab024. https://doi.org/10.1093/jncics/pkab024
Thomas BE et al (2016) Psycho-Socio-Economic Issues Challenging Multidrug Resistant Tuberculosis Patients: A Systematic Review. Plos One 11(1):e0147397. https://doi.org/10.1371/journal.pone.0147397
Nizamli F, Anoosheh M, Mohammadi E (2011) Experiences of Syrian women with breast cancer regarding chemotherapy: a qualitative study. Nurs Health Sci 13(4):481–487. https://doi.org/10.1111/j.1442-2018.2011.00644.x
Silva AVD, Zandonade E, Amorim MHC (2017) Anxiety and coping in women with breast cancer in chemotherapy. Revista Latino-Americana de Enfermagem 25:e2891. https://doi.org/10.1590/1518-8345.1722.2891
Alves PC, Santos MCL, Fernandes AFC (2012) Stress and coping strategies for women diagnosed with breast cancer: a transversal study. Online Braz J Nurs 11(2):305–18. https://doi.org/10.5935/1676-4285.20120028
Yang H et al (2021) A qualitative study of the experience of returning to family life and the coping styles of patients after total laryngectomy. Ann Palliat Med 10(11):11482–11491. https://doi.org/10.21037/apm-21-2687
Kim JJ et al (2021) Personal Growth and Well-Being in the Time of COVID: An Exploratory Mixed-Methods Analysis. Front Psychol 12:648060. https://doi.org/10.3389/fpsyg.2021.648060
Norberg A et al (2015) Self-transcendence (ST) among very old people–its associations to social and medical factors and development over five years. Arch Gerontol Geriatr 61(2):247–253. https://doi.org/10.1016/j.archger.2015.04.003
Kang Y et al (2018) Effects of self-transcendence on neural responses to persuasive messages and health behavior change. Proc Natl Acad Sci U S A 115(40):9974–9979. https://doi.org/10.1073/pnas.1805573115
Funding
This study was supported with grants of the Key Research and Development Plan of Shaanxi Province: General Projects—social development field (Grant 2022SF-371).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Chunyan He, Yawei Lin, Tianqi Yang, Wei Chang, Fangning Gao, Shuzhi Xue, Yi Wan, and Rongrong Liu. The first draft of the manuscript was written by Chunyan He, Chao Wu, Yang He. Hongjuan Lang, Baohua Cao gave useful comments to the experiment and helped to revise the manuscript for several times, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The research followed the ethical principles of the Declaration of Helsinki, and ethical approval (KY20192117-F-1) was obtained by the Ethics Committee of the First Affiliated Hospital of the Fourth Military Medical University.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
He, C., Wu, C., He, Y. et al. Characteristics and influencing factors of social isolation in patients with breast cancer: a latent profile analysis. Support Care Cancer 31, 363 (2023). https://doi.org/10.1007/s00520-023-07798-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07798-0