Abstract
Purpose
Despite clinical guidelines, palliative care is underutilized during advanced stage lung cancer treatment. To inform interventions to increase its use, patient-level barriers and facilitators (i.e., determinants) need to be characterized, especially among patients living in rural areas or those receiving treatment outside academic medical centers.
Methods
Between 2020 and 2021, advanced stage lung cancer patients (n = 77; 62% rural; 58% receiving care in the community) completed a one-time survey assessing palliative care use and its determinants. Univariate and bivariate analyses described palliative care use and determinants and compared scores by patient demographic (e.g., rural vs. urban) and treatment setting (e.g., community vs. academic medical center) factors.
Results
Roughly half said they had never met with a palliative care doctor (49.4%) or nurse (58.4%) as part of cancer care. Only 18% said they knew what palliative care was and could explain it; 17% thought it was the same as hospice. After palliative care was distinguished from hospice, the most frequently cited reasons patients stated they would not seek palliative care were uncertainty about what it would offer (65%), concerns about insurance coverage (63%), difficulty attending multiple appointments (60%), and lack of discussion with an oncologist (59%). The most common reasons patients stated they would seek palliative care were a desire to control pain (62%), oncologist recommendation (58%), and coping support for family and friends (55%).
Conclusion
Interventions should address knowledge and misconceptions, assess care needs, and facilitate communication between patients and oncologists about palliative care.
Similar content being viewed by others
Introduction
Lung cancer is the leading cause of cancer mortality in the United States and the second most common cancer among men and women [1]. Psychosocial and physical concerns are prevalent among lung cancer patients[2, 3]. Rigorous randomized controlled trials have shown providing patients with outpatient specialty palliative care during lung cancer treatment addresses common psychosocial and physical concerns, improves quality of life and facilitates end-of-life care[4,5,6]. As such, practice guidelines recommend palliative care be delivered concurrently with cancer treatment for advanced stage lung cancer patients [7].
Unfortunately, less than 30% of patients with advanced stage lung cancer receive palliative care within a year of diagnosis[8]. Patients who reside in rural areas or receive care in the community (vs. academic medical center) may be at increased risk for underutilization[9], presumably because of palliative care provider scarcity. However, research conducted in academic medical centers where palliative care is readily available, yet underutilized, suggest palliative care utilization is determined by intrapersonal (e.g., knowledge, attitudes, beliefs) and interpersonal factors (e.g., patient-provider communication)[10]. These factors have not been well-described among advanced stage lung cancer patients, especially among those residing in rural areas or receiving care in the community. This is a major limitation, as lung cancer is more common in rural areas [11], most patients are treated in the community [12, 13], and rural and community-treated patients may have less exposure to palliative care in their social networks and face more attitudinal and logistical barriers to seeking supportive care. [14]
The goal of the current study was to identify palliative care use and determinants (i.e., knowledge, misperceptions, and reasons for or against using palliative care) among patients receiving treatment for advanced stage lung cancer in an academic medical center or community practice. A secondary goal was to examine palliative care use and determinants based on patient residence (rural vs. urban), treatment setting (academic vs. community), age, and sex. We chose these factors based on the PROGRESS-Plus Framework of social determinants of health and prior literature [14,15,16]. We hypothesized patients who resided in rural areas, received treatment in the community, were older, and male would have less knowledge of palliative care and be more likely to report palliative care misperceptions.
Methods and materials
Study design
Data were collected from a National Cancer Institute-designated Cancer Center and three community oncology sites in Kentucky, US, as part of a multilevel assessment (i.e., patients, providers, and administrators) of palliative care determinants. Community sites were located 1–2 h from the academic medical center. All community sites were accredited by the American College of Surgeons Commission on Cancer and assessed no more than 500 new cancer cases a year. Because of Commission on Cancer accreditation, all had been required to provide palliative care on site or by referral since 2012. At the time of this study, two sites offered outpatient palliative care; the NCI-designated academic medical center and remaining community site only offered inpatient palliative care. Recruitment occurred between July 2020 and July 2021. The recruitment period was prolonged from an intended 6-month target due to COVID-related research support staffing shortages at community sites. Patients were identified by screening oncology schedules using the electronic medical record system. Site coordinators approached eligible patients in clinic or remotely and reviewed a study information sheet. All patients provided informed consent. The University of Kentucky Medical Institutional Review Board approved this study (#55171). Participants received $30.
Participants
Patients were eligible if they were age 18 years or older, spoke English, and were undergoing treatment for advanced stage lung cancer (stage IIIb, IIIc, IV non-small cell lung cancer; extensive stage small cell lung cancer).
Measures
Sociodemographic factors
Patients self-reported sex, age, race, ethnicity, education, employment status, insurance, travel time to cancer care, current and past cancer treatments (e.g., chemotherapy, radiation, immunotherapy) and history of other cancers. Rural residence was determined by the Federal Office of Rural Health Policy’s eligible ZIP codes; any ZIP code with more than 50% of the population residing in a non-metro county or rural census tract was considered rural. Current smoking status (i.e., past month) was assessed with the 4-item base of the Cancer Patient Tobacco Use Questionnaire[17].
Palliative care use
Patients self-reported whether they had met with a palliative care doctor and palliative care nurse as part of their cancer care. Response options included “Never,” “Occasionally,” “Often,” and “Don’t know.” For bivariate analyses, responses were collapsed to “Never,” “Occasionally/Often,” and “Don’t know.”
Palliative care knowledge
Items from the Health Information National Trends Survey[18] assessed perceived palliative care knowledge (e.g., “I know what palliative care is and could explain it to someone else,”), functions (4 items; e.g., “To me, the goal of palliative care is to manage pain and other physical symptoms), and perceptions (5 items). Three perception items were considered misconceptions (e.g., “If you accept palliative care, you must stop other treatments”). Participants responded to these items via a Likert-type scale, where 1 = “strongly disagree” and 4 = “strongly agree.” Participants could also respond “don’t know.” For analysis, responses were collapsed to “agree/strongly agree,” “strongly disagree/disagree,” or “don’t know”. Each item was examined separately. Patients were considered to have endorsed a misconception if they agreed or strongly agreed.
Non-hospice palliative care (NHPC) attitudes
After patients answered questions about palliative care use and knowledge, they were provided with the following description of “non-hospice palliative care” as part of instructions for completing the Palliative Care Attitudes Scale [19]: This section asks you some questions about your beliefs about aspects of health and healthcare, particularly something called “Non-hospice Palliative Care.” Non-hospice palliative care involves discussing ways to address physical symptoms, side effects, and emotional concerns, but it can also help patients and their families with difficult decisions and end-of-life issues during cancer treatment. Non-hospice palliative care can be delivered by a cancer doctor and/or with a team of providers, such as a doctor, a nurse, a psychologist, a nutritionist, and/or a social worker. The term “non-hospice palliative care,” a term standardly used to help differentiate end-of-life palliative care from palliative care provided alongside life-prolonging treatments [20, 21], was used intentionally to help ensure patients answered subsequent questions without mistakenly conflating palliative care with hospice. The Palliative Care Attitudes Scale (PCAS) contains nine items (e.g., “Do you think the visits would help with feelings of sadness and depression?”) related to palliative care. Items were modified to substitute “non-hospice palliative care” for “palliative care,” were responded to on 5-point Likert-type scales with response options that varied by subscale, and summed to yield a total score, with higher scores indicating more positive attitudes. Internal consistency in this sample was good (Cronbach’s α = 0.84).
Barriers and facilitators to non-hospice palliative care
This measure was adapted from another study [10] (see Supplemental Material) and administered after the PCAS. Patients were instructed to rate how factors would influence them to request a non-hospice palliative care visit (i.e., facilitator) or be a reason they would not want to have a non-hospice palliative care visit (i.e., barrier). Instructions further stated, “Starting non-hospice palliative care does not mean you have to stop cancer treatment.” Barriers (e.g., “I am afraid my insurance would not cover non-hospice palliative care”) and facilitators (e.g., “If my oncologist recommended I meet with non-hospice palliative care”) were responded to on a Likert-type scale (facilitators; 1 = very unlikely to 5 = very likely; barriers 1 = not at all a barrier to 5 = very much a barrier). Due to small cell sizes, response were collapsed for analysis ( “not at all”/”slight” = not a barrier; “somewhat”/”moderate”/”very much” = barrier; “very unlikely”/ “unlikely”/””neutral” = not facilitator; “likely”/”very likely” = facilitator). We also examined the proportion reporting each as a major barrier (“very much a barrier”) or strong facilitator (“very likely facilitator”). In analyses examining whether barriers or facilitators differed by clinical or sociodemographic characteristics, we used three barrier (“not at all”/”slight” = not a barrier; “somewhat/moderate” = moderate barrier; “very much” = major barrier) and facilitator categories (“very unlikely”/”unlikely”/”neutral” = not facilitator; “likely” = facilitator; “very likely” = strong facilitator).
Statistical analyses
Univariate means and standard deviations and percentages were used to describe palliative care outcomes. Bivariate tests compared patients within two designations of rural residence (i.e., rural vs. urban) and cancer care facility (i.e., academic medical vs. community cancer center) for these variables. Follow-up analyses compared outcomes by outpatient palliative care access at sites (outpatient services available/not available). We used chi-square or Fisher’s exact tests for categorical variables and two-sample t-tests or one-way ANOVA for continuous variables. All analyses were conducted in SPSS. A two-tailed alpha of 0.05 was used.
Results
Study population
Screening identified 137 eligible patients, of whom 110 were contacted and approached; 77 (70%) completed the survey; 24 (22%) refused; nine (8%) were lost to follow-up. Reasons for refusal included: “Just do not want to” (n = 6); “Too much going on” (n = 6); “Topic not of interest” (n = 5); “Not feeling well enough physically” (n = 2); “Not feeling well enough mentally” (n = 2); and “Do not have time” (n = 2). Refusal reason was missing for one patient. Patients who refused to participate were not significantly different from those who enrolled with respect to age, sex or education.
See Table 1 for demographic and clinical characteristics. Age, education, sex, and health literacy were not significantly different based on rural residence or cancer facility. Rural patients comprised 53.3% of the sample from a community site vs. 75.0% of the sample from the academic medical center (p = 0.06). 62.5% of patients treated in the academic medical center traveled an hour or more for cancer care vs. 8.9% of those treated in the community (p < 0.001).
Palliative care use
Roughly half (49.4%) reported they had never met with a palliative care doctor as part of their cancer care; 20.8% reported occasionally meeting with one; 11.7% reported often meeting with one; 15.6% did not know if they had met with a palliative care doctor. Over half (58.4%) reported they had never met with a palliative care nurse as part of their cancer care; 11.7% reported occasionally meeting with one; 10.4% reported often meeting with one; and 15.6% did not know.
Patients treated in the community were more likely to report having seen a palliative care doctor compared to patients treated in an academic medical center (45.5% vs. 16.2%, p = 0.024). Follow-up analysis suggested this difference was driven by two community sites in which 50% and 53.8% of patients reported having seen a palliative care doctor compared to 16.2% (academic medical center) and 25% (third community site; p = 0.129); both community sites with at least 50% reporting they had seen a palliative care doctor offered outpatient palliative care onsite. None of the other pre-specified factors were associated with palliative care use.
Palliative care knowledge, misconceptions, and functions
Only 18.2% (n = 14) reported they knew what palliative care was and could explain it (Table 2). Patients’ self-reported knowledge of palliative care was not significantly different by cancer treatment facility (community vs. academic medical center), residence (rural vs. urban), or availability of outpatient palliative care onsite (Table 2). 34.2% of women vs. 52.6% of men had never heard of palliative care (p = 0.052). Age was not significantly different across knowledge responses (M age for those who had never heard of palliative care = 66.7; SD = 10.0; M age for those who knew a little = 64.3, SD = 10.6; knew what it was and could explain it = 60.4; SD = 10.0, p = 0.158).
When presented with misconceptions (e.g., accepting palliative care means giving up), between 30–38% said they did not know (Fig. 1a). 16.9% (n = 13) reported palliative care was the same as hospice and using it meant giving up. Between 26–32% did not know whether some of the functions of palliative care were accurate (e.g., helps manage pain and other physical symptoms; Fig. 1b). Most (53.3%; n = 41) thought it was a doctor’s responsibility to inform patients of the option of palliative care (Fig. 1b).
a Proportion of patients endorsing misconceptions of palliative care (N = 77). Note: “PC” = Palliative care. b Perception of palliative care functions and doctor obligation’s to discuss it (N = 77). Note: “It’s the doctor’s obligation” – verbatim item was “It is the doctor’s obligation to inform all patients with cancer about the option of palliative care”. Percentages do not sum to 100% as responses were missing from 2-3 people
Non-hospice palliative care (NHPC)
Attitudes
Patients reported positive attitudes towards NHPC (M = 24.83; SD = 7.98; range = 6–45). Attitudes towards NHPC were not significantly different by cancer treatment facility (M = 23.2; SD = 7.16 among academic medical center patients vs. M = 26.0; SD = 8.41 among community cancer patients; p = 0.14) or whether outpatient palliative care was available onsite (M = 23.88; SD = 8.25 among patients treated where outpatient palliative care was not available vs. M = 26.17; SD = 7.52 among those where outpatient palliative care was available, p = 0.233). Attitudes towards NHPC were also not significantly different by residence (M = 24.54, SD = 7.17 for rural patients; M = 25.35, SD = 9.38 for urban patients, p = 0.71), age (r = -0.01, p = 0.93), or sex (M men = 24.5; SD = 7.4; M female = 25.2; SD = 8.6, p = 0.73).
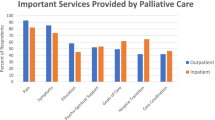
Barriers to non-hospice palliative care
The most common stated barrier to seeking non-hospice palliative care was being unsure what it would offer (64.9%, n = 50; Fig. 2a), followed by insurance coverage concerns (62.3%, n = 48), oncologist not discussing it (59.7%, n = 46) and difficulty attending multiple appointments (59.7%, n = 46). Of stated barriers, the most common “major barrier” was concern insurance would not cover it (28.6%; n = 22; Fig. 2a), followed by an oncologist not discussing it with them (23.4%; n = 18). Barriers were not significantly different based on pre-specified patient demographic factors, treatment facility, or availability of outpatient palliative care onsite, though several differences in magnitude were in the expected direction (Supplemental Table 1).
Facilitators to non-hospice palliative care
The most common reasons patients reported they would seek non-hospice palliative care were to manage uncontrolled pain (62.4%; n = 48; Fig. 2b), if an oncologist recommended it (58.5%; n = 45), or to help family and friends cope (54.6%; n = 42). These facilitators were also the most frequently reported “very likely” facilitators (Fig. 2b).
Facilitators were not significantly different based on cancer treatment facility, patient residence, or availability of outpatient palliative care onsite (Supplemental Table 2). Women were more likely to report that a weak support system would be a reason for them to seek non-hospice palliative (32.4% of women vs. 8.6% of men, p = 0.047). Older patients were more likely to report an oncologist recommending non-hospice palliative care would be a reason for them to seek it (Mage “not facilitator” = 59.5, SD = 10.6, “likely facilitator” = 65.3, SD = 10.3, “very likely facilitator” = 67.5, SD = 7.3, p = 0.02).
Discussion
This is among the first studies to describe palliative care use and determinants among patients with advanced stage lung cancer and the first to examine patient perspectives from both academic and community-based treatment facilities [10]. Overall, we found that although many patients reported having seen a palliative care provider during cancer care, palliative care knowledge was low and many mistakenly conflated it with hospice. The barriers and facilitators identified to using palliative care once we differentiated it from hospice suggested that (beyond addressing misconceptions) patient-level interventions to increase palliative care use among advanced stage lung cancer patients should: educate patients about palliative care’s role in cancer treatment; discuss insurance coverage and costs of using palliative care; facilitate palliative care discussions with oncology providers; and reduce the burden of additional medical appointments associated with palliative care. In most instances, subgroup analyses did not suggest determinants differed based on patient characteristics, treatment setting, or availability of outpatient palliative care onsite, suggesting patient-level intervention strategies identified may be broadly applicable.
Encouragingly, about half of patients reported having seen a palliative care provider as part of their cancer care – a significantly higher proportion than the estimated 12–30% from electronic health record and claims data studies [8, 22]. Because two community sites sampled offered outpatient palliative care on site, it is possible this high proportion reflects use when palliative care is better integrated into routine oncology care. Indeed, patients treated at our NCI-designated cancer center which did not offer outpatient palliative care were less likely to report having seen a palliative care doctor. However, it is also possible, and perhaps more likely, that some patients may have mistakenly reported seeing a palliative care provider, as over 40% had never heard of palliative care.
Patients in this study had very low knowledge of palliative care regardless of treatment facility, outpatient palliative care availability onsite, and patient residence. Though not statistically significant, a higher proportion of men vs. women had never heard of palliative care. By virtue of being less likely to assume a role of informal caregiver [23], men may have had less exposure to palliative care. It is also possible men may have been less likely to receive information about palliative care because they are assumed to be less interested in it. Contrary to our findings, prior research has found men have less favorable attitudes towards palliative care and are less likely to receive it (though, interestingly, men seemed to benefit more from palliative care in the landmark trial of palliative care in lung cancer)[24, 25]. Sex differences in palliative care use and determinants should continue to be studied to inform intervention tailoring.
In addition to low stated knowledge of palliative care, we found knowledge deficits regarding palliative care’s distinction from hospice and its role in cancer treatment. Between 12–20% endorsed common misconceptions about palliative care, mistakenly assuming it is the same as hospice; means giving up; or requires stopping cancer treatment. Further, between 26–32% did not know about palliative care’s role in treatment (e.g., that it could help manage pain and other physical symptoms). The proportion of patients endorsing misconceptions was much lower than in other studies [26,27,28], presumably because we allowed “don’t know” responding. About a third of the sample responded “don’t know” to misconception items. Particularly for patients who conflated palliative care with solely end-of-life care, “don’t know” responses could have functioned as a way to avoid experiencing uncomfortable thoughts associated with palliative care [29].
A unique strength of this study was that after assessing palliative care knowledge and misconceptions, we provided patients with a description of palliative care that we thought would address the major misconceptions patients have about it (i.e., that it is the same as hospice and using it means stopping treatment) and then asked patients to indicate reasons they would or would not use “non-hospice palliative care” [20, 21]. We did this to identify determinants beyond the most identified barriers of conflating palliative care with hospice or “giving up”[30, 31]. Patients reported they would seek non-hospice palliative care to manage a variety of concerns and care needs, including uncontrolled pain, treatment side effects, and depression and anxiety, to support friends and family’s coping, and to discuss goals of care. They also stated they would seek non-hospice palliative care if their oncologist recommended it. An oncologist’s recommendation seemed particularly important to older patients, which is consistent with prior research suggesting older people prefer to receive information from a provider vs. other source [22]. Patients also endorsed several reasons for not using non-hospice palliative care, including uncertainty about its benefits; lack of discussion with an oncologist; difficulty attending additional medical appointments (perhaps more so for patients at an academic medical center); and concern about insurance coverage. These results align with other findings pointing to the critical role of oncology providers’ support of palliative care [32], need for remote delivery options[33], and cost discussions and assistance [34].
This study was conducted during the height of the initial wave of the COVID-19 pandemic, which likely reduced participation, though our participation rate was still relatively high (70%). Other study limitations include a cross-sectional design, limited statistical power for detecting subgroup differences, self-report of palliative care utilization, and a predominantly White, non-Hispanic sample. This reflects the demographics of the region but limits generalizability. We did not assess other barriers and facilitators that may be salient among people from other backgrounds [35]. We also asked patients to indicate hypothetical reasons they would or would not use “non-hospice palliative care,” and not reasons why they had or had not already seen a palliative care provider. However, because palliative care knowledge deficits and misconceptions are common and a major deterrent to palliative care use [36], identifying additional determinants almost requires a hypothetical framework like we used to further assess determinants in this study. Additional strengths include a high response rate; assessment of patients from both an academic and community setting; and strong rural representation.
Conclusion
Interventions to increase palliative care utilization among patients with advanced stage lung cancer need to address knowledge, misconceptions, and care delivery barriers, including lack of oncology provider discussions of palliative care during cancer treatment and cost and time concerns. Interventions should also assess patients’ care needs and inform patients of palliative care’s role in addressing those needs with their oncologist.
Availability of data and materials
The dataset generated and analyzed in this study is available from the corresponding author upon reasonable request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33
Vijayvergia N, Shah PC, Denlinger CS (2015) “Survivorship in Non-Small Cell Lung Cancer: Challenges Faced and Steps Forward,” (in eng). J Natl Compr Cancer Netw JNCCN 13(9):1151–1161
LeBlanc TW, Nickolich M, Rushing CN, Samsa GP, Locke SC, Abernethy AP (2015) What bothers lung cancer patients the most? A prospective, longitudinal electronic patient-reported outcomes study in advanced non-small cell lung cancer. Support Care Cancer J Article 23(12):3455–3463. https://doi.org/10.1007/s00520-015-2699-4
Bakitas MA et al (2015) Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol 33(13):1438
Bakitas M et al (2009) Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 302(7):741–749
Temel JS et al (2010) Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N Engl J Med 363(8):733–742. https://doi.org/10.1056/NEJMoa1000678
Ferrell BR et al (2017) “Integration of Palliative Care Into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update,” (in eng). J Clin Oncol 35(1):96–112. https://doi.org/10.1200/jco.2016.70.1474
Huo J, Hong YR, Turner K, Bian J, Grewal R, Wilkie DJ (2019) “Utilization pattern and service settings of palliative care for patients with metastatic non-small cell lung cancer,” (in eng). Cancer 125(24):4481–4489. https://doi.org/10.1002/cncr.32478
Huo J et al (2021) “Geographic variation in palliative care delivery among patients diagnosed with metastatic lung cancer in the USA: Medicare population-based study,” (in eng). Support Care Cancer 29(2):813–821. https://doi.org/10.1007/s00520-020-05549-z
Feld E, Singhi EK, Phillips S, Huang LC, Shyr Y, Horn L (2019) “Palliative Care Referrals for Advanced Non-small-cell Lung Cancer (NSCLC): Patient and Provider Attitudes and Practices,” (in eng). Clin Lung Cancer 20(3):e291–e298. https://doi.org/10.1016/j.cllc.2019.02.002
Atkins GT, Kim T, Munson J (2017) “Residence in Rural Areas of the United States and Lung Cancer Mortality. Disease Incidence, Treatment Disparities, and Stage-Specific Survival,” (in eng). Ann Am Thorac Soc 14(3):403–411. https://doi.org/10.1513/AnnalsATS.201606-469OC
Green LA, Fryer GE Jr, Yawn BP, Lanier D, Dovey SM (2001) “The ecology of medical care revisited,” (in eng). N Engl J Med 344(26):2021–2025. https://doi.org/10.1056/nejm200106283442611
Clauser SB, Johnson MR, O’Brien DM, Beveridge JM, Fennell ML, Kaluzny AD (2009) “Improving clinical research and cancer care delivery in community settings: evaluating the NCI community cancer centers program,” (in eng). Implement Sci 4:63. https://doi.org/10.1186/1748-5908-4-63
Andrykowski MA, Burris JL (2010) “Use of formal and informal mental health resources by cancer survivors: differences between rural and nonrural survivors and a preliminary test of the theory of planned behavior,” (in eng). Psychooncology 19(11):1148–1155. https://doi.org/10.1002/pon.1669
O’Neill J et al (2014) “Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health,” (in eng). J Clin Epidemiol 67(1):56–64. https://doi.org/10.1016/j.jclinepi.2013.08.005
Mackenzie CS, Gekoski WL, Knox VJ (2006) “Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes,” (in eng). Aging Ment Health 10(6):574–582. https://doi.org/10.1080/13607860600641200
Land SR et al (2016) “Cognitive testing of tobacco use items for administration to patients with cancer and cancer survivors in clinical research,” (in eng). Cancer 122(11):1728–1734. https://doi.org/10.1002/cncr.29964
Nelson DE et al (2004) “The Health Information National Trends Survey (HINTS): development, design, and dissemination,” (in eng). J Health Commun 9(5):443–60. https://doi.org/10.1080/10810730490504233. (discussion 81-4)
Perry LM, Hoerger M, Malhotra S, Gerhart JI, Mohile S, Duberstein PR (2020) “Development and Validation of the Palliative Care Attitudes Scale (PCAS-9): A Measure of Patient Attitudes Toward Palliative Care,” (in eng). J Pain Symptom Manage 59(2):293-301.e8. https://doi.org/10.1016/j.jpainsymman.2019.09.008
Kelley AS, Meier DE (2010) Palliative Care — A Shifting Paradigm. N Engl J Med 363(8):781–782. https://doi.org/10.1056/NEJMe1004139
Beasley A, Bakitas MA, Edwards R, Kavalieratos D (2018) Models of non-hospice palliative care: a review. Ann Palliat Med 8(Suppl 1):S15–S21
Chaudhuri S, Le T, White C, Thompson H, Demiris G (2013) “Examining health information-seeking behaviors of older adults,” (in eng). Comput Inform Nurs 31(11):547–553. https://doi.org/10.1097/01.NCN.0000432131.92020.42
N. A. f. C. Caregiving (2016) Cancer Caregiving in the U.S.: An Intense, Episodic, and Challenging Care Experience. Bethesda, MD. Available: https://www.caregiving.org/wp-content/uploads/2020/05/CancerCaregivingReport_FINAL_June-17-2016.pdf
Saeed F, Hoerger M, Norton SA, Guancial E, Epstein RM, Duberstein PR (2018) Preference for Palliative Care in Cancer Patients: Are Men and Women Alike? J Pain Symptom Manag 56(1):1-6.e1. https://doi.org/10.1016/j.jpainsymman.2018.03.014
Nipp RD et al (2016) “Age and Gender Moderate the Impact of Early Palliative Care in Metastatic Non-Small Cell Lung Cancer,” (in eng). Oncologist 21(1):119–126. https://doi.org/10.1634/theoncologist.2015-0232
Trivedi N, Peterson EB, Ellis EM, Ferrer RA, Kent EE, Chou WS (2019) “Awareness of Palliative Care among a Nationally Representative Sample of U.S. Adults,” (in eng). J Palliat Med 22(12):1578–1582. https://doi.org/10.1089/jpm.2018.0656
Zhu Y, Enguídanos S (2019) “When Patients Say They Know About Palliative Care, How Much Do They Really Understand?,” (in eng). J Pain Symptom Manage 58(3):460–464. https://doi.org/10.1016/j.jpainsymman.2019.05.008
Flieger SP, Chui K, Koch-Weser S (2020) “Lack of Awareness and Common Misconceptions About Palliative Care Among Adults: Insights from a National Survey,” (in eng). J Gen Intern Med 35(7):2059–2064. https://doi.org/10.1007/s11606-020-05730-4
Shen MJ, Wellman JD (2019) “Evidence of palliative care stigma: The role of negative stereotypes in preventing willingness to use palliative care,” (in eng). Palliat Support Care 17(4):374–380. https://doi.org/10.1017/s1478951518000834
Zimmermann C et al (2016) “Perceptions of palliative care among patients with advanced cancer and their caregivers,” (in eng). CMAJ 188(10):E217-e227. https://doi.org/10.1503/cmaj.151171
Kumar P et al (2012) “Utilization of supportive and palliative care services among oncology outpatients at one academic cancer center: determinants of use and barriers to access,” (in eng). J Palliat Med 15(8):923–930. https://doi.org/10.1089/jpm.2011.0217
Schenker Y, Park SY, Maciasz R, Arnold RM (2014) “Do patients with advanced cancer and unmet palliative care needs have an interest in receiving palliative care services?,” (in eng). J Palliat Med 17(6):667–672. https://doi.org/10.1089/jpm.2013.0537
Finlay E, Newport K, Sivendran S, Kilpatrick L, Owens M, Buss MK (2019) Models of Outpatient Palliative Care Clinics for Patients With Cancer. J Oncol Pract 15(4):187–193. https://doi.org/10.1200/jop.18.00634
Haverfield MC, Singer AE, Gray C, Shelley A, Nash A, Lorenz KA (2020) Implementing routine communication about costs of cancer treatment: perspectives of providers, patients, and caregivers. Support Care Cancer 28(9):4255–4262. https://doi.org/10.1007/s00520-019-05274-2
Johnson KS (2013) “Racial and ethnic disparities in palliative care,” (in eng). J Palliat Med 16(11):1329–1334. https://doi.org/10.1089/jpm.2013.9468
Steffen L et al (2018) Prognostic understanding and barriers to palliative care in patients with metastatic lung cancer on immunotherapy. J Clin Oncol 36(34_suppl):36–36. https://doi.org/10.1200/JCO.2018.36.34_suppl.36
Acknowledgements
This research was supported by the Patient-Oriented and Population Sciences Shared Resource of the University of Kentucky Markey Cancer Center (P30CA177558). Shaylla Shelton was supported by the University of Kentucky Markey Cancer Center’s Appalachian Career Training in Oncology (ACTION) Program (NC R25 CA221765). We would like to acknowledge Trey Alexander and John Kim for their assistance with coordinating across community cancer care facilities and the Markey Cancer Center Research Communication Office for their assistance preparing the manuscript.
Funding
16–182-28, American Cancer Society Institutional Research Grant (LEM).
P30CA177558
134,579-RSG-20–058-01-PCSM, Hoerger (PI), American Cancer Society.
2KL2TR001996-05A1 (LEM)
R25CA221765 (SS)
Author information
Authors and Affiliations
Contributions
Laurie McLouth, Michael Hoerger, Marc Kiviniemi, Jamie Studts, Timothy Mullett, Jessica McFarlin, Jerod Stapleton, and Nancy Schoenberg contributed to study conception and design. Material preparation was conducted by Laurie McLouth, Vilma Bursac, Michael Hoerger, Jessica McFarlin, Timothy Mullett, and Nancy Schoenberg. Data collection was conducted by Laurie McLouth, Vilma Bursac, David Goebel, Ravneet Thind, and Laura Trice. Data analysis was conducted by Laurie McLouth, Brent Shelton, and Andrew Shearer. The first draft of the manuscript was written by Laurie McLouth, Tia Borger, and Shaylla Shelton. All authors commented on drafts and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board at the University of Kentucky (#55171). All participants provided informed consent. Written documentation of informed consent was waived for this study.
Consent for Publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McLouth, L.E., Borger, T., Bursac, V. et al. Palliative care use and utilization determinants among patients treated for advanced stage lung cancer care in the community and academic medical setting. Support Care Cancer 31, 190 (2023). https://doi.org/10.1007/s00520-023-07649-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07649-y