Abstract
Objective
This study aims to explore the 5Ts teach-back(5Ts) to improve oral nutritional supplements (ONS) compliance of discharged patients after gastric cancer surgery.
Setting and methods
Patients were recruited from the Bethune First Hospital of Jilin University. The patients were randomly assigned to 5Ts (n = 54) and routine health education (n = 54). Weekly ONS compliance was collected by “weekly ONS diary.” ONS knowledge, health literacy, and health education satisfaction were collected at baseline and 5 weeks after discharge. Chi-square test, Mann–Whitney U test, and T test were used for data analysis.
Results
At the end of the intervention, there were 41 and 40 patients in intervention and control group. 5Ts significantly improve ONS compliance, ONS knowledge level (P = 0.000), health literacy level (P = 0.011), and health education satisfaction (P = 0.009) of patients. At the end of follow-up, there were 30 and 27 patients in two groups, and no significant difference in ONS compliance (P = 0.728).
Conclusion
The 5Ts can significantly improve patients’ ONS compliance and the effect of health education.
Trial registration number
This prospective trial was registered in the Chinese Clinical Trial Registry at ChiCTR2000040986 (http://www.chictr.org.cn).
Patient or public contribution
Jia Wang and Haiyan Hu contributed to the performance of the study, analysis and interpretation the data, and drafted the manuscript; Jianan Sun and Qing Zhang contributed to the supervision of the study and interpreted the data; Zhiming Chen contributed to the analysis and interpretation the data; Qiuchen Wang contributed to the performance of the study and revised the manuscript; Mingyue Zhu contributed to interpretation the data; Jiannan Yao contributed to revise the manuscript; Hua Yuan and Xiuying Zhang contributed to the conception of the study, performed the study, interpreted the data, and significantly revised the manuscript. All authors screened the final version of the manuscript.
Similar content being viewed by others
Introduction
Gastric cancer was the fifth most common cause of cancer worldwide and was currently the third most common cause of cancer death [1]. At present, although medical treatment has made great progress, surgery excision was still the main effective treatment for gastric cancer [2]. However, gastrectomy and intraoperative digestive tract reconstruction will cause metabolic changes and absorption disorders in patients, resulting in reduced nutritional intake and seriously affecting the nutritional status of patients [3]. In addition, the average length of hospital stay in China was limited and patients did not have enough time to fully recover, leading to a high incidence of malnutrition and worsening nutritional status after discharge [4]. Numerous studies had shown that approximately 40 to 80% of gastrectomy patients suffered from malnutrition [5, 6], which may further lead to numerous negative consequences for patients after discharge [7], including reduced chemotherapy tolerance, impaired quality of life, increased morbidity, and reduced survival [8, 9]. Therefore, appropriate nutritional support is of great significance to improve the nutritional status of post-discharge patients after surgery for gastric cancer.
The European Society of Clinical Nutrition and Metabolism (ESPEN) guidelines recommend oral nutritional supplements (ONS) as first-line nutritional therapy for malnutrition after tumor surgery [10]. Numerous clinical studies and systematic analyses have shown that ONS can improve nutritional status and clinical outcomes for hospitalized patients or medical patients in community and nursing home Settings, and further save overall health care costs [11,12,13]. According to the consensus, discharged patients after gastric cancer surgery should continue to receive nutritional therapy based on ONS for three months or more as needed, depending on their eating and nutritional status [3]. Patient compliance to ONS was the key to the smooth implementation of ONS [14]. However, the ONS compliance was at a poor level due to age, lack of ONS education, lack of relevant knowledge, taste and other reasons [15]. For example, the study of Wan et al. showed that the average compliance of patients with gastric cancer was only 30.59% at 12 weeks (w), and the compliance decreased obviously at 5w [16]. It was worth noting that some researchers had pointed out that lack of ONS education was a significant barrier to ONS compliance [17, 18].
Effective health education could improve the patient’s understanding of the disease, so that the patient could consciously cooperate with the treatment [19]. However, in the current clinical practice, the health education mode of medical staff to patients was mostly oral education or distribution of brochures [20], which was a kind of infusing education, was unilateral knowledge input to patients, ignoring the understanding degree of patients to input knowledge [21]; some patients and their families complained that medical staff convey information in ways they could not understand, resulting in poor communication between the two sides[22]. In addition, health literacy(HL) reflected an individual’s ability to acquire, understand and process basic health information and services, and to make appropriate health decisions to maintain and promote their own health [23]. Currently, the majority of cancer patients had low levels of HL, such patients had low problem solving ability, treatment motivation and compliance [24]. Therefore, clarifying patients’ understanding level of disease knowledge, effectively promoting doctor-patient communication and enhancing patients' HL are conducive to enhancing patients' awareness of self-management, which may be the key issues to be solved in health education programs for patients with gastric cancer.
The teach-back method was a teaching strategy of two-way transmission of information. Health Care Personnel (HCP) conducted health education to the patients in plain language, and then let the patients describe in their own language to determine their level of understanding or what they had forgotten. If there was wrong or not understood information, HCP will emphasize again and cycle until the patients understands and grasps it correctly [25]. A preliminary review of the literatures showed that the teach-back method had been used as an educational strategy for low-income women [26], people with low HL [27], and people with chronic diseases [28], which could improve patient understanding [29], informed consent [30], and improve dietary compliance [31]. However, the operating steps of the teach-back method have not been completely unified in various studies at present [32]. Based on previous studies on the teach-back method, Kathryn and other researchers developed the 5Ts for Teach Back (5Ts), which was a standardized and operable scheme [33]. Therefore, in this study, the health education program developed based on the 5Ts was expected to improve the ONS compliance of post-discharge patients with gastric cancer after gastrectomy.
Methods
Study design
This study was a single-center, prospective randomized controlled trial. From January 2021 to October 2021, we evaluated the effect of the health education based on 5Ts of post-discharge after gastric cancer surgery. The study was conducted at the Bethune First Hospital of Jilin University. All patients received intervention for 5w (T1) and were followed up to 12w (T2) after discharge. Primary outcomes were ONS compliance, HL, and ONS knowledge level. Secondary outcomes included health education compliance and satisfaction.
Participants
During the study, all eligible patients were screened for inclusion in the study. Inclusion criteria: age ≥ 18 years; All patients were pathologically diagnosed as gastric cancer stage I, II, and III before surgery; subtotal gastrectomy or total gastrectomy; nutritional risk screening 2002 (NRS2002) score ≥ 3; patient-generated subjective global assessment (PG-SGA) grades of B or C; There were no preoperative gastrectomy, radiotherapy or chemotherapy; the patient was capable of oral feeding; patients or their family members had smartphones and could use WeChat; patients were written informed consent. Patients with concomitants of other cancers, allergies to components in ONS, mental illness, impaired consciousness, and inability to communicate normally were excluded from the study.
The sample size was 40 patients in each group at the end of the intervention, allowing 10% dropped loss and 10% mortality. The calculation formula was as follows: n1 = n2 = (Uα + Uβ) 22P (1-P) / (P1-P2)2, consider α = 0.05, Uα = 1.96; β = 0.1, Uβ = 1.28, based on the study of Xu et al.[34].
Randomization, allocation concealment, and blinding
The block random grouping method was adopted, and the length of block was six. According to the order of admission, every six subjects are divided into one group, which is grouped by simple random grouping method. The specific steps are as follows:
-
1.
Number the patients according to the sequence of admission time;
-
2.
Using the rand function in Excel, give each patient a random number;
-
3.
The random numbers were arranged from small to large. The patients ranked one-three were taken as the experimental group and the patients ranked four-six were taken as the control group. Patients were given opaque envelopes containing results presented in forms of one (intervention group) and two (control group). The nurses who issued the envelopes and statistical analysts were unaware of the grouping results.
Procedures
Health education content
The members of the research team include professors in the field of gastric cancer nutrition in the Nursing College and nutrition specialist nurses in gastrointestinal surgery. According to the content of conventional health education and clinical practice, on the basis of studies, books, guidelines and consensus [3, 14, 35], this study developed ONS health education content and made health education manuals, including five themes. They are as follows: nutrition and malnutrition; the definition and function of ONS; forms and types of ONS; ONS administration method and precautions; adverse reactions and treatment measures of ONS. After the health education program is formed, the members of the research team will discuss the content together and modify the inappropriate points. After the modification, the program will be further implemented in clinical practice. In our study, patients’ primary physicians prescribed ONS for their first postoperative exhaust, usually within 7 days after surgery. At this point, the researchers will begin a health education program for both groups of patients.
Intervention group
The intervention group received a health education program based on the 5Ts. Kathryn et al. developed the 5Ts in order to make the process of teach-back more specific and convenient for learning. 5Ts was a standardized, actionable definition of Teach Back with five specific, observable steps: Triage, Tools, Take Responsibility, Tell Me, and Try Again. The Triage, Tools, and Try Again steps were used to effectively delivery information, while the Take Responsibility and Tell Me steps were used to assess whether the patient had received the information [33].
Triage: In the triage step, the HCP determined the most important educational topics. Research showed that the more information a clinician provided, the less information a patient remembered correctly. Therefore, an HCP with several pieces of information to cover must categorize the information by selecting what was most important for the patient to remember or understand. This step was key and prevented the HCP from providing too much information. For example, in the topic “Nutrition and malnutrition,” the researchers identified information that was most important to patients, such as the concept of malnutrition and its impact on patients. In the process of information delivery, it was necessary to pay attention to replace medical terms involved in educational information with daily terms, so that patients can better understand.
Tools: A tool was broadly defined as anything that helped the HCP provide a clear explanation. Flyers, simple pen and paper drawings, models, diagrams or videos, using HCP’s own body (such as a fist to represent a beating heart), or even a related story were all possible tools. In this study, the tools used to deliver educational information included a 17-min video, ONS instruction sheets and HCP's own body, etc.
Take Responsibility: The “Take Responsibility” step was crucial to no-shaming in the definition of Teach-back. This step occurred after the HCP passed the topic information. The ideal “taking responsibility” involved two things. The first was an acknowledgement of the amount or complexity of the information given. If a misunderstanding did occur, this could normalize the misunderstanding, thereby reducing the patient's sense of shame. The second implication was that HCP rather than the patient was being tested, a factor that also reduced the burden on the patient. In this study, when patients had misunderstandings, the researcher would say, “It's a lot of information and it's hard to remember all of it at once, so I want to make sure I have a good explanation.”
Tell Me: In the “Tell Me” phase, HCP invited patients to state what they understood in their own words. Suppose an HCP spend 20 min explaining “adverse reactions and treatment measures of ONS” and then said, “Tell me what you've learned about ONS.” In this case, the patient might be overwhelmed by the amount of information she needed to answer and might not know where to start. Tell me more specifically, for example, “What are the adverse effects of ONS?” "What happens when you have diarrhea after taking ONS?” This approach allowed the patient and the HCP to focus on a specific piece of information.
Try Again: If the patient did not understand, the HCP must explain it again and modify the explanation to make it clearer. Depending on the size of the error, another round of teach-back might be required. HCP can take responsibility for mistakes by going back to the “take responsibility” step, for example, “I'm sorry, I must have not explained it well enough.” Taking responsibility again reduced the shame patients feel about mistakes.
In order to ensure the quality of health education, each round of education focused on only one health education item. Repeated the 5Ts for the next round of health education. Within 1w to 5w after discharge, patients' recall of educational themes will be evaluated by telephone or WeChat(a popular social media app in China) [36] by asking questions. Patients with incorrect answers will be re-educated on the wrong themes through 5Ts.
Control group
The control group received traditional health education in the gastrointestinal surgery department. According to ONS health education manual, oral health education was delivered to patients and their families by researcher. Within 5w after discharge, the patients’ recall of educational themes was also evaluated weekly by telephone or WeChat. If the patients had any questions and actively sought answers, the researchers would answer them.
Data collection
Demographic and clinical information questionnaire
Demographic and clinical information was collected at baseline (T0) using questionnaires and collected by specialized researcher who was unaware of the grouping. Demographic information included age, sex, education level, comorbidities, and other data. Preoperative height, weight, body mass index (BMI), NRS2002 [37], and PG-SGA [38] were assessed by clinical dietitians. And the hospital’s medical record system was used to collect surgical information, pathological stages, and whether patients received chemotherapy.
Primary endpoints
ONS compliance
“Weekly ONS diary” were collected to calculate ONS compliance [16]. The “weekly ONS diary” produced by Wan et al., contains the date, the name of ONS, the amount of taking ONS, and adverse reactions. Calculation method of compliance: weekly compliance rate (%) = dosage taken/prescribed dosage *100% weekly. In this study, the weekly compliance rate of patients within 12w after discharge was collected, and the compliance rate at 5w and 12w as well as the average compliance rate within 5w and 12w were statistically analyzed.
In this study, patients were divided into compliance groups with dual indicators of Dose and days every week after discharge, and then the trend of ONS compliance of discharged patients after gastric cancer surgery was analyzed: Full Dose and Full Time (DT); Full Dose and Insufficient time (Dt); Insufficient dose and Full Time (dT); Insufficient dose and Insufficient time (dt). The average patient compliance rate was calculated by adding the compliance rate per patient divided by the total number of patients.
ONS knowledge level
ONS knowledge level was designed by researchers according to health education content [3, 14, 35], including five themes, a total of 20 questions, 5 points for each question. The total score ranged from 0 to 100, and the higher the score, the higher the ONS knowledge level.
HL
HL was measured by the Chinese version of Health Literacy Management Scale (HeLMS) translated [39], which contained 24 items in 4 dimensions. It included the ability to acquire information (9 items), the ability to communicate and interact (9 items), the willingness to improve health (4 items) and the willingness to provide financial support (2 items). Likert 5 score was adopted, 1 meant “very difficult or very unwilling” and 5 meant “no difficulty or very willing.” The total score ranged from 24 to 120. The higher the score is, the higher the health literacy level is. The coefficient of total Amount Table Cronbach’s α is 0.901, Cronbach’s in each dimension α are 0.885–0.925, the reliability and validity are good. HL and ONS knowledge level will be collected at T1.
Secondary endpoints
Health education compliance
Because of the total number of health education participation was 6, the calculation method of health education compliance was: participation times / 6 * 100%.
Health education satisfaction
Based on the Chinese version of “Ware's” Patient Satisfaction Questionnaire (PSQ-18) translated by Cui et al. [40], this study was modified to form the health education satisfaction questionnaire. PSQ-18 was divided into 7 dimensions, including overall satisfaction, technical service quality, nurses’ interpersonal communication ability, nurse-patient communication level, service economy, service timeliness, and service accessibility. Each dimension included forward and reverse questioning methods. The corresponding questions were normalized before statistical analysis, and the higher the score, the better the satisfaction. PSQ-18’s maximum satisfaction score for each question was 5 points, with a full score of 90 points. The coefficient of total Cronbach’s α is 0.852, split half reliability is 0.813, and KMO is 0.867, indicating good reliability and validity. Health education compliance and satisfaction will be collected at T1.
In order to exclude the influence of diet, we calculated and collected the calories in patients' daily diet based on the Chinese local diet assessment Form (1–5 points) [41].
Ethics
The study was conducted at the Bethune First Hospital of Jilin University. The study was approved by our Institutional Review Board (No.2020082802) and carried out in accordance with the Declaration of Helsinki (as revised in 2013) and its subsequent amendments to ethical standards. In addition, all participants provided written informed consent forms.
Statistical analysis
All statistical analyses were performed using SPSS25.0 software (SPSS Inc., Chicago, IL). Normal distribution data were expressed by median ± standard deviation (M ± SD). Non-normally distributed data are summarized and compared by median (P25, P75), and classified variables are expressed in numbers and percentages. Wilcoxon rank sum test was used to evaluate changes in weight and BMI at T0, T1 and T2 in two groups. Chi-square test, Mann–Whitney U test, and T-test were used to assess differences in baseline characteristics and other outcome measures between the two groups. When P value < 0.05, the difference was considered statistically significant.
Results
Patients characteristics
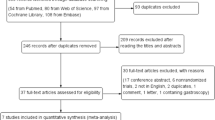
Of the 160 patients, 108 met the inclusion criteria and were randomized, with 54 assigned to the intervention group and 54 to the control group. Baseline demographic and clinical characteristics of patients, as shown in Table 1, showed no significant difference between the two groups (P > 0.05). During the intervention, 13 patients in the intervention group and 14 patients in the control group were lost due to death, complications, loss of contact and other reasons, but no patients changed from the control group to the intervention group. In addition, during the follow-up from 5 to 12w after discharge, 11 patients and 13 patients in the two groups were lost due to death and non-compliance, respectively. Finally, data of 81 patients were included for analysis at T1 and 57 patients were included for analysis at T2 (Fig. 1).
Primary endpoints
Comparison of ONS compliance between the two groups within 12w after discharge
As can be seen from Fig. 2, ONS compliance of all patients from discharge to T2 showed a decreasing trend over time. At T1, the compliance rate of patients in the intervention group (55.69%) was significantly higher than that of the control group (32.86%) (P = 0.009), while at T2, the compliance rate of patients in the intervention group was higher than that of the control group (25.95% vs 21.40%). But there was no significant difference (P = 0.728). In addition, the average compliance rate at T1 in the intervention group (65.70%) was significantly higher than that in the control group (43.73%) (P = 0.005). The average compliance rate at T2 between the two groups showed the same results (48.14% vs 32.77%, P = 0.020). In addition, patients in the intervention group showed a sharp decline in compliance 4-5w after discharge, but the decline rate slowed down 5-6w after discharge.
The number of dT was highest in both groups within 12w after discharge. In Fig. 3, the number of DT in the intervention group decreased gradually throughout the 12-week follow-up period, from more than 20 to less than 10, but remained stable at less than 10 after 9w; the number of dT gradually increased and stabilized at 10w. The number of Dt patients was the lowest, and decreased gradually in the first 5w after discharge, and disappeared at 10w. The number of dt was increasing during 12w after discharge. Figure 4 reflects the change of ONS compliance in the control group within 12w after discharge. With the change of time, the number of DT gradually decreased, stabilized at less than 10 from the second week, and remained unchanged from the 8–12w. DT occupies the largest proportion, but the number is gradually decreasing with the change of time. Dt had the lowest number and disappeared in 9w.
Comparison of ONS knowledge level between the two groups before and after intervention
At T0, there was no significant difference in the scores and total scores of all dimensions between the two groups (P > 0.05). Nutrition and malnutrition, ONS Administration Method and Precautions, Adverse reactions and treatment measures of ONS, and Total scores reported by the intervention group were significantly higher than those of control group at T1 (P = 0.036; 0.006; 0.012; 0.000). There were no significant differences between the two groups in other outcomes of ONS knowledge level (P > 0.05) (Table 2).
Comparison of HL level between the two groups before and after intervention
From Table 3, at T0, there was no significant difference between the two groups in the scores of all dimensions and total scores (P > 0.05). At T1, compared to the control group, patients in the intervention group had significant improvement in three dimensions: the ability to acquire information, the ability to communicate and interact, and the willingness to improve health and total scores (P = 0.041; 0.020; 0.014; 0.011). And the total HL score in both groups was at a high level. However, there was no significant difference between the two groups in “The willingness to provide financial support” (P = 0.411).
Secondary endpoints
Comparison of health education compliance between two groups
75.92% of patients randomly assigned to the intervention group received 6 times of health education, while 74.07% of patients in the control group received 6 times of health education, and there was no significant difference between the two groups (P = 0.780).
Comparison of health education satisfaction between two groups
From Table 4, regarding the score of health education satisfaction, Nurses' interpersonal communication ability (P = 0.018), nurse-patient communication level (P = 0.031), service timeliness (P = 0.023), service accessibility (P = 0.007), and total scores (P = 0.009), there existed significant differences among the two groups at T1.
Number of lost to follow-up
Within 12w after discharge, the number of patients lost to follow-up gradually increased with time, and the number of patients lost to follow-up in the control group was slightly higher than that in the intervention group. During the period from 5 to 6w, the number of lost visits increased considerably (Fig. 5). The number of people who dropped follow-up at 10–12w did not increase in the intervention group, but increased slowly to 11–12w in the control group.
Discussion
Although ONS therapy was the preferred way to prevent and treat malnutrition in patients with gastric cancer, improve the nutritional status of patients and reduce the cost of nutrition-related treatment, ONS compliance had become a major obstacle to the effective role of ONS. This study showed that health education based on 5Ts could improve the ONS compliance of discharged patients with nutritional risk after gastric cancer surgery, increased the understanding of ONS knowledge, and improved the HL level of patients. In addition, health education based on 5Ts also promoted the satisfaction of patients with health education and the communication between nurses and patients. These results had important significance for HCP optimized health education program to improve post-discharge ONS compliance and improve the treatment outcome of patients with nutritional risk after gastric cancer surgery.
The intake of ONS was often lower than the recommended dose, which made the intake of nutrients unable to meet the target amount of individual needs and affected the effect of nutritional treatment [15, 42]. Chu et al. explored the effect of teach-back method on ONS health education of discharged patients after gastrointestinal tumor surgery, and the results showed that the ONS compliance of patients in the intervention group was significantly higher. However, it only collected the ONS compliance of patients 7–10 days after discharge, which was relatively short [43]. This study revealed the effect of 5Ts on ONS compliance of discharged patients with gastric cancer, and further explored its long-term effects. The results showed that health education based on 5Ts could effectively improve the average compliance rate within 5w and 12w after discharge, and the compliance rate at 5w was significantly higher than that of the control group (55.69% vs 32.86%), but no significant difference was found at 12w (25.95% vs 21.40%). A previous study showed that patients with gastric cancer had an average ONS compliance of 30.59% within 12w after surgery and 12.9% compliance at 12w [16]. Obviously, in our study results, both the average compliance within 12w and the compliance at 12w of patients in the control group were higher than those in the Wan et al.’s study [16]. The prevention and management of adverse effects of ONS should be included in health education [3, 44], in this study, health education programs in both groups focused more on symptom management, which may have contributed to improved ONS compliance. This conformed that Marusic et al. study’s opinion that adding prevention and early detection of adverse drug reactions in health education can improve patients’ drug compliance [45]. Therefore, this study confirmed that the prevention and management of adverse effects of ONS was an indispensable part of health education for cancer patients after discharge. In addition, patients in the intervention group showed a sharp decline in compliance 4–5w after discharge, but the decline rate slowed down 5–6w after discharge. Four to six weeks after surgery was the peak of chemotherapy for cancer patients [46, 47]. During chemotherapy, patients gave up taking ONS due to the taste of ONS and adverse reactions, but will choose to resume taking ONS after chemotherapy due to the effect of peer support [16]. This seemed to explain this phenomenon. In future studies, we need to pay attention to the role of peer support in improving patients’ ONS compliance.
More surprisingly, our results showed that there were four different states of ONS compliance in gastric cancer patients during their stay at home. Patients were divided into groups of compliance with dual indicators of dose and days every week after discharge. We found that dT consistently predominated in both groups at 12w after discharge. This was consistent with Wan et al.’s findings [16]. Patients in the dT group, account for a large proportion, were able to meet the demand for times, but not for doses. This might be due to the digestive tract symptoms, such as nausea and vomiting, after taking ONS, causing patients to reduce the dose of ONS. The studies had reported that 21–60% of patients will stop taking ONS after adverse reactions [44]. Therefore, we suggest that during the follow-up of patients, regardless of whether the patients correctly answered the questions raised by researchers on the topic of “prevention and management of adverse effects of ONS,” we will conduct health education for patients according to the steps of 5Ts. How to identify and target such patients to strengthen the dose of ONS to improve compliance is worthy of further exploration by researchers. Based on qualitative interview results from previous study, patients may be supported by their peers to take ONS every day.
The study had demonstrated that knowledge of ONS treatment and disease plays an important role in long-term ONS compliance in patients with cancer malnutrition [35]. The results of our study showed that health education based on 5Ts could significantly improve patients’ ONS knowledge level. In this study, the content of ONS health education included five themes, among which “The Definition and Function of ONS” and “Forms and types of ONS” showed no significant difference between two groups, but improved compared with T0. This might be because when patients were discharged, doctors will prescribe ONS suitable for them according to their nutritional status and personal conditions. When they occurred adverse reactions after taking ONS at home, the researchers assessed the causes and treatment measures of the adverse reactions by asking questions. If the adverse reactions were not alleviated after correct treatment, the type or brand of ONS would be changed. At this point, the researchers will again educate the patients on the “Administration Method and Precautions” of the replacement ONS through 5Ts. So patients might be more relatively familiar with only the ONS they regularly took. However, there were still some patients who interrupted follow-up and gave up taking ONS. A mixed study showed that some patients might believe that tonics were more effective than ONS because of traditional Chinese beliefs [16]. And the other study had also shown that patients might be unaware of the function of ONS and thus affect compliance [48]. Therefore, future studies can further improve patients' understanding of the functions and types of ONS, change patients' traditional and inherent concepts, and strengthen patients' motivation to take ONS.
The studies had shown that patients with high HL level had the motivation and ability to acquire, understand and use information, and were more likely to take correct self-management measures to improve medication compliance [49]. In our study, both groups of patients had moderate levels of HL after admission. After 5w of intervention, the HL of patients in the intervention group was significantly higher than that in the control group. Although our study also found that the health education compliance rate of patients in the intervention group was slightly higher than that in the control group (75.92% vs 74.07%), as can be seen from the observation of long-term effect, the number of DT in the two groups gradually decreased with the passage of time, but the number of DT in the intervention group was higher than that in the control group. In addition, the number of patients lost to follow-up within 12w after discharge increased with time, but the number of patients lost to follow-up in the intervention group was less than the control group. It may be that 5Ts improves compliance by enhancing the patient's HL and thereby enhancing their self-management level. However, the direct relationship between them needs to be further determined, and how to improve patients’ long-term follow-up compliance in future studies needs to be further explored. It’s worth noting that in the dimension of “The willingness to provide financial support,” there was no significant difference between the two groups. In this study, health education was free of charge and did not increase the treatment cost of patients, causing additional economic burden to patients.
The results of this study showed that health education based on 5Ts could effectively strengthen the communication between HCP and patients, and significantly improve patients' satisfaction with health education. Although there was no significant difference in overall satisfaction, technical service quality and service economy between the two groups, they were all at a high level. Hu et al.’s study showed that under the continuous inquiry and guidance of HCP, on one hand, patients’ health needs were met and their health knowledge level was improved; On the other hand, patients and their families could truly feel respected and loved, which was conducive to the establishment of a harmonious and equal relationship between HCP and patients, so that HCP could maximize the understanding and trust of patients and their families, and ultimately improve patient satisfaction [50]. In the study of Li et al., a self-developed satisfaction scale was used to evaluate tongue cancer patients, and the results showed that the satisfaction of patients in the intervention group was significantly higher than that in the control group after the intervention of the teach-back health education model [51]. Our results also confirmed this.
Finally, there were some limitations in this study. First, this was a single-center study, and there may have been some degree of bias. Second, due to the impact of COVID-19, we cannot require all patients to return to the hospital for blood nutrition measurements and re-evaluation of PG-SGA. Therefore, we only use body weight and BMI to measure the nutritional status of patients. This was not only a traditional parameter, but also a simpler and more convenient nutrition assessment tool [4]. It had been reported that these parameters had a good prognosis for patients undergoing gastrectomy [52, 53]. Third, the number of patients in this study was continuously lost during the intervention process, resulting in the loss of a large number of samples. But given the possibility of such a situation, we recruited as many patients as possible at the beginning of the study and reached the required sample size at the end of the intervention.
Conclusion
To our knowledge, this is the first report of health education based on 5TS improving ONS compliance in discharged patients after gastric cancer surgery. Our study showed that such health education can improve patients’ short-term and long-term ONS compliance, and their ONS knowledge level, HL level and health education satisfaction. Future health education should pay more attention to the functions and types of ONS, so as to further strengthen the motivation of patients to take ONS.
Data availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper.
Code availability
No code.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 68(6):394–424
Yu J, Huang C, Sun Y, Su X, Cao H, Hu J, Wang K, Suo J, Tao K, He X et al (2019) Effect of Laparoscopic vs Open Distal Gastrectomy on 3-Year Disease-Free Survival in Patients With Locally Advanced Gastric Cancer: The CLASS-01 Randomized Clinical Trial. JAMA 321(20):1983–1992
Ziyu Li CY, Shen Li (2020) Consensus of Chinese expert panel on perioperation nutriton therapy of gastric cancer (2019 edition). Chin J Pract Surg 40(02):145–151
Oh SE, Choi MG, Seo JM, An JY, Lee JH, Sohn TS, Bae JM, Kim S (2019) Prognostic significance of perioperative nutritional parameters in patients with gastric cancer. Clin Nutr (Edinburgh, Scotland) 38(2):870–876
Adiamah A, Skořepa P, Weimann A, Lobo DN (2019) The Impact of Preoperative Immune Modulating Nutrition on Outcomes in Patients Undergoing Surgery for Gastrointestinal Cancer: A Systematic Review and Meta-analysis. Ann Surg 270(2):247–256
Chen X, Yang K, Zhang X, Li K (2020) Meta-analysis of preoperative oral nutritional supplements for patients with gastric cancer: East Asian experience. Eur J Clin Nutr 74(7):991–1000
Zhu MW, Yang X, Xiu DR, Yang Y, Li GX, Hu WG, Wang ZG, Cui HY, Wei JM (2019) Effect of oral nutritional supplementation on the post-discharge nutritional status and quality of life of gastrointestinal cancer patients after surgery: a multi-center study. Asia Pac J Clin Nutr 28(3):450–456
Kocarnik JM, Hua X, Hardikar S, Robinson J, Lindor NM, Win AK, Hopper JL, Figueiredo JC, Potter JD, Campbell PT et al (2017) Long-term weight loss after colorectal cancer diagnosis is associated with lower survival: The Colon Cancer Family Registry. Cancer 123(23):4701–4708
Seretis C, Kaisari P, Wanigasooriya K, Shariff U, Youssef H (2018) Malnutrition is associated with adverse postoperative outcome in patients undergoing elective colorectal cancer resections. J BUON 23(1):36–41
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hütterer E, Isenring E, Kaasa S et al (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr (Edinburgh, Scotland) 36(1):11–48
Elia M, Normand C, Norman K, Laviano A (2016) A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr (Edinburgh, Scotland) 35(2):370–380
de van der Schueren MAE, (2019) Use and effects of oral nutritional supplements in patients with cancer. Nutrition (Burbank, Los Angeles County, Calif) 67–68:110550
Kim SH, Lee SM, Jeung HC, Lee IJ, Park JS, Song M, Lee DK, Lee SM (2019) The Effect of Nutrition Intervention with Oral Nutritional Supplements on Pancreatic and Bile Duct Cancer Patients Undergoing Chemotherapy. Nutrients 11(5)
Chuangqi Chen HJ, Jianhui Chen, Zhanyu Li (2018) Oral nutritional supplement for the management of accelerated rehabilitation of patients undergoing colorectal surgery: Lingnan expert consensus (2018 version)-Physician Association of Accelerated Rehabilitation Surgeons of Guangdong Province. J Dig Oncol (Electronic Version) 10(04):167–172
Ping He KX, Jiangnan Liu, Hanping Shi (2017) Affecting the compliance of oral nutritional supplements. Electronic Journal of Metabolism and Nutrition of Cancer 4(02):232–241
Wan GY, Yuan H, Xue H, Li HQ, Hu HY, Zhang XY (2021) Assessment of compliance with oral nutritional supplementation and exploration of barriers and facilitators for patients after gastrectomy: A mixed-methods study. J Adv Nurs 77(6):2845–2859
Hogan SE, Solomon MJ, Carey SK (2019) Exploring reasons behind patient compliance with nutrition supplements before pelvic exenteration surgery. Support Care Cancer 27(5):1853–1860
Lidoriki I, Schizas D, Mylonas KS, Frountzas M, Mastoraki A, Pikoulis E, Liakakos T, Karavokyros I (2020) Oral Nutritional Supplementation Following Upper Gastrointestinal Cancer Surgery: A Prospective Analysis Exploring Potential Barriers to Compliance. J Am Coll Nutr :1–7
Haixia Chen KC, Fei Wang (2020) Effect of health education nursing on knowledge cognition degree and llife quality of patients with chronic obstructive pulmonary disease. Hebei Med J 42(15):2385–2387+2391
Yoshida N, Baba Y, Shigaki H, Harada K, Iwatsuki M, Kurashige J, Sakamoto Y, Miyamoto Y, Ishimoto T, Kosumi K et al (2016) Preoperative Nutritional Assessment by Controlling Nutritional Status (CONUT) is Useful to estimate Postoperative Morbidity After Esophagectomy for Esophageal Cancer. World J Surg 40(8):1910–1917
Karsenty C, Landau M, Ferguson R (2013) Assessment of medical resident's attention to the health literacy level of newly admitted patients. J Community Hosp Intern Med Perspect 3(3–4)
Huang. L (2015) The Study of Using Teach Back in Perioperative Patients with Esophageal Cancer. Master. Fujian Medical University
LynnMarkDO F (2009) Health literacy and the elderly. In., vol. 1. Osteopathic Family Physician 64–69
Li Huang SP (2016) The Status and Influencing Factors of Health Literacy among Cancer Patients. Nursing J Chin People's Liberation Army 33(02):17–20+25
Tamura-Lis W (2013) Teach-Back for quality education and patient safety. Urologic Nursing 33(6):267–271, 298
Wilson FL, Baker LM, Nordstrom CK, Legwand C (2008) Using the teach-back and Orem’s Self-care Deficit Nursing theory to increase childhood immunization communication among low-income mothers. Issues Compr Pediatr Nurs 31(1):7–22
Kountz DS (2009) Strategies for improving low health literacy. Postgrad Med 121(5):171–177
Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S (2016) The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database System Rev Implement Rep 14(1):210–247
Griffey RT, Shin N, Jones S, Aginam N, Gross M, Kinsella Y, Williams JA, Carpenter CR, Goodman M, Kaphingst KA (2015) The impact of teach-back on comprehension of discharge instructions and satisfaction among emergency patients with limited health literacy: A randomized, controlled study. J Commun Healthc 8(1):10–21
Lorenzen B, Melby CE, Earles B (2008) Using principles of health literacy to enhance the informed consent process. AORN J 88(1):23–29
Negarandeh R, Mahmoodi H, Noktehdan H, Heshmat R, Shakibazadeh E (2013) Teach back and pictorial image educational strategies on knowledge about diabetes and medication/dietary adherence among low health literate patients with type 2 diabetes. Prim Care Diabetes 7(2):111–118
Shersher V, Haines TP, Sturgiss L, Weller C, Williams C (2020) Definitions and use of the teach-back method in healthcare consultations with patients: A systematic review and thematic synthesis. Patient education and counseling
Anderson KM, Leister S, De Rego R (2020) The 5Ts for Teach Back: An Operational Definition for Teach-Back Training. Health Lit Res Pract 4(2):e94–e103
Xu J (2020) Effect of teach-back health education on self-efficacy and prognosis of patients with intracerebral hemorrhage in EICU. Med Pharm Yunnan 41(02):201–203
Hanping Shi WC, Zhiwei Jiang, Weijun Tian, Junqiang Chen, Mingsong Li (2016) Clinical application of oral nutritional supplement. Electron J Metab Nutr Cancer 3(04):229–233
Yu Q, Xu L, Li L, Zhi M, Gu Y, Wang X, Guo H, Li Y, Fan Y, Yang B et al (2019) Internet and WeChat used by patients with Crohn’s disease in China: a multi-center questionnaire survey. BMC Gastroenterol 19(1):97
Kondrup J, Rasmussen HH, Hamberg O et al (2003) Nutritional Risk Screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 22:321–336
Bauer J, Capra S, Ferguson M (2002) Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr 56(8):779–785
Haolin Sun HP, Hua Fu (2013) Dimensional structure analysis of health Literacy Survey scale for Patients with Chronic Disease J Environ Occup Med 30(03):171–175
Jianglin Hu XL, Yuxiao Zhang, Mengyuan Tian, Xin Fang, Xiao Yin, Dan Cui (2017) Residents' satisfaction of community health service and its influencing factors with PSQ-18 scale. Modern Prev Med 44(11):1991–1994+1999
Rihua Cong HS (2018) The invention of a simple diet selfassessment tool for cancer patients. Electron J Metab Nutr Cancer 5(1):11–13
Hubbard GP, Elia M, Holdoway A, Stratton RJ (2012) A systematic review of compliance to oral nutritional supplements. Clin Nutr (Edinburgh, Scotland) 31(3):293–312
Yaqin Chu ZJ, Mingyue Shao, Cheng Zhang, Nanhai Peng (2020) Effect of teach-back teaching on oral nutritional supplements for discharged patients after gastrointestinal tumor operation. J Nurs (China) 27(07):69–72
Beiwen Wu XY, Suyun Li, Xiaoping Shao, Xiaoli Tang, Yongyi Zhan, Liyuan Qin, Qian Qi, Weixin Cao (2021) Expert consensus on improving the compliance to oral nutritional supplements in clinical practice. Electron J Metab Nutr Cancer 8(5):487–499
Marušić S, Meliš P, Lucijanić M, Grgurević I, Turčić P, Neto PRO, Bilić-Ćurčić I (2018) Impact of pharmacotherapeutic education on medication adherence and adverse outcomes in patients with type 2 diabetes mellitus: a prospective, randomized study. Croat Med J 59(6):290–297
Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, Nashimoto A, Fujii M, Nakajima T, Ohashi Y (2011) Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol 29(33):4387–4393
de van der Schueren MAE, Laviano A, Blanchard H, Jourdan M, Arends J, Baracos VE (2018) Systematic review and meta-analysis of the evidence for oral nutritional intervention on nutritional and clinical outcomes during chemo(radio)therapy: current evidence and guidance for design of future trials. Ann Oncol 29(5):1141-1153
Ginzburg Y, Shmilovitz I, Monastyrsky N et al (2018) Barriers for nutritional care in the transition from hospital to the community among older patients. Clin Nutr ESPEN 25:56–62
Liu H, Shen J, Li S, Song Y, Ju M (2021) Research on the Health Literacy Status and Compliance Behavior of Patients with Acute Coronary Syndrome. Comput Math Methods Med 2021:9648708
Jinxiu Hu QC, Hui Zhang,Juan Wang,Peng Zhu (2020) Study on the application of multiple health education combined with teach-back method in the perioperative period of esophageal cancer. Anhui Med J 41(06):724–726
Huichuan Li YW, Qiang Zhang (2019) The Application of Teach-back Health Education Model in Perioperative Period of Tongue Cancer Patients. J QILU Nurs 25(24):15–18
Kong SH, Lee HJ, Na JR, Kim WG, Han DS, Park SH, Hong H, Choi Y, Ahn HS, Suh YS et al (2018) Effect of perioperative oral nutritional supplementation in malnourished patients who undergo gastrectomy: A prospective randomized trial. Surgery 164(6):1263–1270
Komatsu H, Yagasaki K, Yamaguchi T (2016) Effects of a nurse-led medication self-management programme in cancer patients: protocol for a mixed-method randomised controlled trial. Bmc Nursing 15
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 31800895] to Xiuying Zhang, and the Higher Education Research Project[JGJX2019D10] of Jilin Province to Hua Yuan.
Author information
Authors and Affiliations
Contributions
Jia Wang and Haiyan Hu contributed to the performance of the study, analysis, and interpretation the data, and drafted the manuscript; Jianan Sun and Qing Zhang contributed to the supervision of the study and interpreted the data; Zhiming Chen contributed to the analysis and interpretation the data; Qiuchen Wang contributed to the performance of the study and revised the manuscript; Mingyue Zhu contributed to interpretation the data; Jiannan Yao contributed to revise the manuscript; Hua Yuan and Xiuying Zhang contributed to the conception of the study, performed the study, interpreted the data, and significantly revised the manuscript. All authors screened the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The study was approved by our Institutional Review Board (No.2020082802) and carried out in accordance with the Declaration of Helsinki (as revised in 2013) and its subsequent amendments to ethical standards. This trial was registered in the Chinese Clinical Trial Registry at ChiCTR2000040986 (http://www.chictr.org.cn).
Consent to participate
The authors declare that all participants provided written informed consent forms.
Consent for publication
The authors declare that they all agreed to publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jia Wang and Haiyan Hu are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Hu, H., Sun, J. et al. The effectiveness of health education based on the 5Ts for teach-back on oral nutritional supplements compliance of post-discharge patients after surgery for gastric cancer: a randomized controlled trial. Support Care Cancer 31, 157 (2023). https://doi.org/10.1007/s00520-023-07581-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07581-1